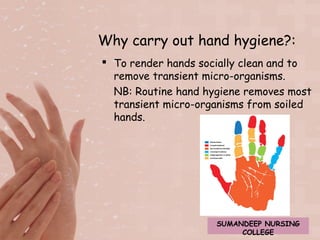
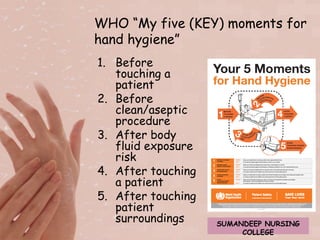
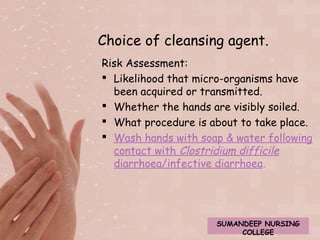
The document discusses the importance of hand hygiene for preventing the spread of infection. It states that hand hygiene is the single most important measure and is essential for patient safety. It provides details on proper hand hygiene technique, including washing hands with soap and water for 40-60 seconds, paying special attention to areas often missed like fingertips and webs between fingers. It emphasizes drying hands thoroughly to prevent microorganisms from thriving in moist environments.