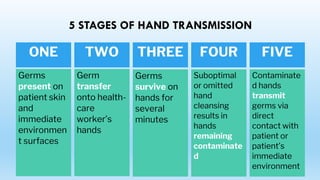
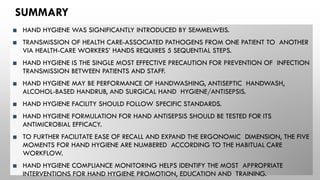
This document outlines key information on hand hygiene for healthcare workers, including:
I. The history of hand hygiene and how practices have evolved over time.
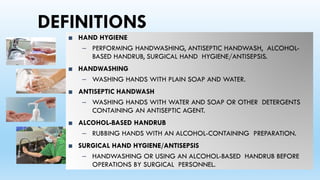
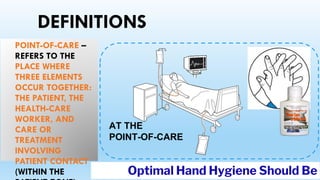
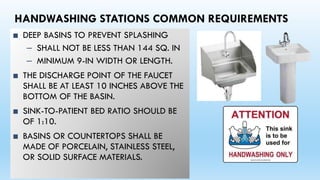
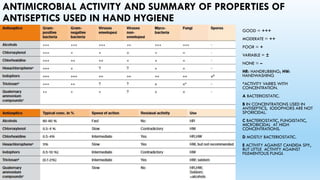
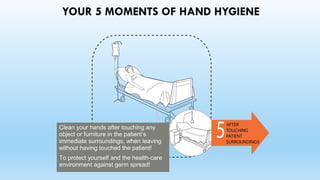
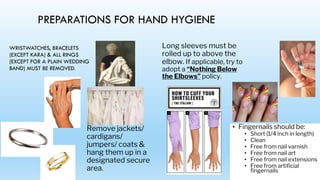
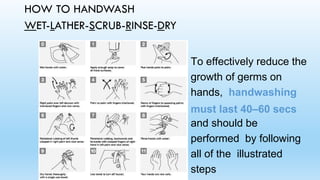
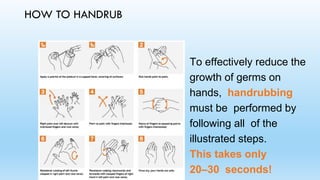
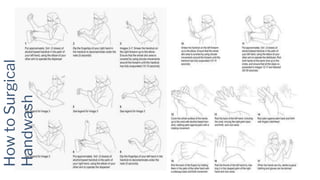
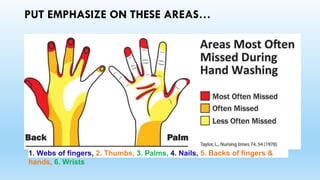
II. Important definitions related to hand hygiene techniques and the types of facilities needed to properly conduct hand hygiene.
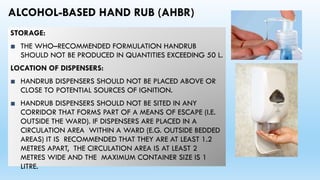
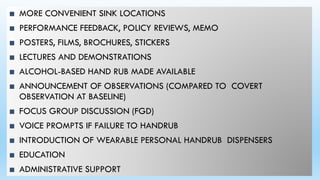
III. Proper hand hygiene requires access to running water, soap, drying methods, and alcohol-based hand rubs located at points of care.