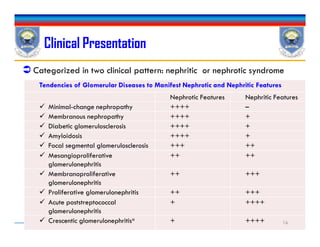
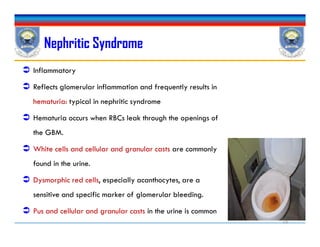
The document discusses glomerulonephritis, which refers to diseases of the glomeruli in the kidneys mediated by immune mechanisms. It can present as either a nephritic or nephrotic syndrome. Nephritic syndrome is characterized by hematuria, hypertension, and variable proteinuria, while nephrotic syndrome presents with massive proteinuria (>3.5 g/day), edema, hyperlipidemia, and sometimes a hypercoagulable state. The pathogenesis involves immune complex deposition or T-cell mediated responses targeting antigens in the glomerular basement membrane or mesangium. Treatment aims to control symptoms and slow disease progression using immunosuppressants or ACE inhibitors depending on the specific type
![Renal Disorders PharmacotherapyRenal Disorders Pharmacotherapy
Chapter 4
Glomerulonephritis
Renal Disorders Pharmacotherapy
By: Tsegaye Melaku
[B.Pharm, MSc, Clinical Pharmacist]
tsegayemlk@yahoo.com or tsegaye.melaku@ju.edu.et ++251913765609251913765609
Chapter 4
Glomerulonephritis](https://image.slidesharecdn.com/glomerulonephritis-170330071106/85/Glomerulonephritis-1-320.jpg)


![Introduction…
Glomerulonephritis: a collection of glomerular diseases mediated
by different immunologic pathogenic mechanisms.
The unique capillary bed of the glomerulus allows passage of small
non-protein plasma constituents up to the size of inulin [5.2 kDa];
exclude macromolecules equal to or larger than albumin (69 kDa).
The precise pathogenetic mechanisms of many glomerular diseases
remain unknown.
The available therapeutic regimens are still far from optimal.
Glomerulonephritis: a collection of glomerular diseases mediated
by different immunologic pathogenic mechanisms.
The unique capillary bed of the glomerulus allows passage of small
non-protein plasma constituents up to the size of inulin [5.2 kDa];
exclude macromolecules equal to or larger than albumin (69 kDa).
The precise pathogenetic mechanisms of many glomerular diseases
remain unknown.
The available therapeutic regimens are still far from optimal.
7](https://image.slidesharecdn.com/glomerulonephritis-170330071106/85/Glomerulonephritis-7-320.jpg)



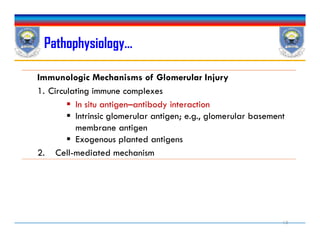
![ Production of antibodies to endogenous or exogenous antigens.
Endogenous antigens[intrinsic glomerular antigens]: Heymann
antigen on the epithelial cell or Goodpasture antigen on the GBM,
or previously sequestered antigens [DNA/thyroglobulin]
Exogenous antigens: viral, bacterial, parasitic, or fungal in origin.
Complexes of antigens and antibodies may be formed in the
circulation and then passively entrapped in the glomerular capillary
or mesangium.
The type and extent of glomerular damage are dependent on the
location of the immune complex formation and the rate at which it is
removed.
Impaired removal facilitates the growth of the complex and thus
increases the likelihood of glomerular damage.
Pathophysiology…
Production of antibodies to endogenous or exogenous antigens.
Endogenous antigens[intrinsic glomerular antigens]: Heymann
antigen on the epithelial cell or Goodpasture antigen on the GBM,
or previously sequestered antigens [DNA/thyroglobulin]
Exogenous antigens: viral, bacterial, parasitic, or fungal in origin.
Complexes of antigens and antibodies may be formed in the
circulation and then passively entrapped in the glomerular capillary
or mesangium.
The type and extent of glomerular damage are dependent on the
location of the immune complex formation and the rate at which it is
removed.
Impaired removal facilitates the growth of the complex and thus
increases the likelihood of glomerular damage. 12](https://image.slidesharecdn.com/glomerulonephritis-170330071106/85/Glomerulonephritis-12-320.jpg)




![The syndrome may be the result of primary diseases of the
glomerulus, or be associated with systemic diseases such as
diabetes mellitus, lupus, amyloidosis, and preeclampsia.
Albuminuria >3 g daily is associated with a significant increase in
serum cholesterol concentrations [increase in total cholesterol, TG,
VLDL, LDL]
Nephrotic Syndrome…
The syndrome may be the result of primary diseases of the
glomerulus, or be associated with systemic diseases such as
diabetes mellitus, lupus, amyloidosis, and preeclampsia.
Albuminuria >3 g daily is associated with a significant increase in
serum cholesterol concentrations [increase in total cholesterol, TG,
VLDL, LDL]
22](https://image.slidesharecdn.com/glomerulonephritis-170330071106/85/Glomerulonephritis-22-320.jpg)
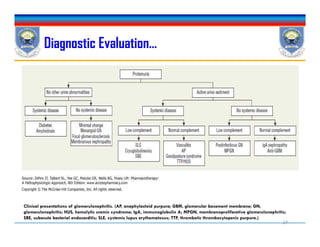
![Diagnostic Evaluation
Extensive medical history obtained to identify potential systemic
causes[see above table].
Medication, environmental, and occupational histories,
Physical examination and laboratory evaluation: for presence of
systemic diseases.
Patient's age, gender, and ethnic background: to pinpoint the
specific type of glomerular disease.
Proliferative glomerulonephritis <40 yrs
Membranous glomerulonephritis >50 yrs
Extensive medical history obtained to identify potential systemic
causes[see above table].
Medication, environmental, and occupational histories,
Physical examination and laboratory evaluation: for presence of
systemic diseases.
Patient's age, gender, and ethnic background: to pinpoint the
specific type of glomerular disease.
Proliferative glomerulonephritis <40 yrs
Membranous glomerulonephritis >50 yrs
24](https://image.slidesharecdn.com/glomerulonephritis-170330071106/85/Glomerulonephritis-24-320.jpg)



![Treatment
General Approach
Specific pharmacologic therapy for the glomerular disease
Supportive measures to prevent and/or treat the pathophysiologic
sequelae[hypertension, edema, and progression of renal disease].
Management of extrarenal complications of heavy proteinuria
[hypoalbuminaemia, hyperlipidemia, and thromboembolism].
General Approach
Specific pharmacologic therapy for the glomerular disease
Supportive measures to prevent and/or treat the pathophysiologic
sequelae[hypertension, edema, and progression of renal disease].
Management of extrarenal complications of heavy proteinuria
[hypoalbuminaemia, hyperlipidemia, and thromboembolism].
29](https://image.slidesharecdn.com/glomerulonephritis-170330071106/85/Glomerulonephritis-29-320.jpg)

![Pharmacologic Therapy
Immunosuppressive agents, alone or in combination: used to alter the
immune processes.
Consider corticosteroids
Immunosuppressive and anti-inflammatory activities.
reduce the production and/or release of inflammatory mediators PG, LTs, PAFs, TNF & IL-1.
Inhibit movement of leukocytes and macrophages to the site of inflammation.
Cytotoxic agents[cyclophosphamide, Chlorambucil, or azathioprine]
Cyclosporine: reduce lymphokine production by activated T lymphocytes, and it may
decrease proteinuria by improving the permselectivity of the GBM.
Mycophenolate mofetil: useful in different glomerulonephritis because of its effects on T- and
B-cell lymphocytes.
Immunosuppressive Agents
Immunosuppressive agents, alone or in combination: used to alter the
immune processes.
Consider corticosteroids
Immunosuppressive and anti-inflammatory activities.
reduce the production and/or release of inflammatory mediators PG, LTs, PAFs, TNF & IL-1.
Inhibit movement of leukocytes and macrophages to the site of inflammation.
Cytotoxic agents[cyclophosphamide, Chlorambucil, or azathioprine]
Cyclosporine: reduce lymphokine production by activated T lymphocytes, and it may
decrease proteinuria by improving the permselectivity of the GBM.
Mycophenolate mofetil: useful in different glomerulonephritis because of its effects on T- and
B-cell lymphocytes.
34](https://image.slidesharecdn.com/glomerulonephritis-170330071106/85/Glomerulonephritis-34-320.jpg)
![Diuretics
For management of nephrotic edema
In addition to salt restriction, bed rest, and use of support stockings.
Delivery of diuretic to the kidney tubules is normal
However, large amounts of protein in the urine promotes drug binding
reduces the availability of the diuretic to the luminal receptor sites.
Reduced sodium delivery to the distal tubule secondary to decreased glomerular
perfusion may also alter diuretic effectiveness.
Large doses of the loop diuretic[ e.g. Furosemide160 to 480 mg], may be
needed for patients with moderate edema
Thiazide diuretic or metolazone : added to enhance natriuresis.
For management of nephrotic edema
In addition to salt restriction, bed rest, and use of support stockings.
Delivery of diuretic to the kidney tubules is normal
However, large amounts of protein in the urine promotes drug binding
reduces the availability of the diuretic to the luminal receptor sites.
Reduced sodium delivery to the distal tubule secondary to decreased glomerular
perfusion may also alter diuretic effectiveness.
Large doses of the loop diuretic[ e.g. Furosemide160 to 480 mg], may be
needed for patients with moderate edema
Thiazide diuretic or metolazone : added to enhance natriuresis.
35](https://image.slidesharecdn.com/glomerulonephritis-170330071106/85/Glomerulonephritis-35-320.jpg)


![Statins
An abnormal lipoprotein profile increases the risk of atherosclerosis and coronary
heart.
A low-fat diet is usually not sufficient to correct hyperlipoproteinemia.
Includes: Lovastatin, pravastatin, simvastatin, and fluvastatin
They reduce total cholesterol LDL cholesterol, and TG
Therapy is especially needed for patients with
Concurrent atherosclerotic cardiovascular disease, or
Additional risk factors for atherosclerosis[smoking and hypertension]
Additionally: they confer renoprotection through
Reduction of cell proliferation and mesangial matrix accumulation
Anti-inflammatory and immunomodulatory effects.
Recent studies: show as if they can reduce proteinuria and delay renal function loss.
An abnormal lipoprotein profile increases the risk of atherosclerosis and coronary
heart.
A low-fat diet is usually not sufficient to correct hyperlipoproteinemia.
Includes: Lovastatin, pravastatin, simvastatin, and fluvastatin
They reduce total cholesterol LDL cholesterol, and TG
Therapy is especially needed for patients with
Concurrent atherosclerotic cardiovascular disease, or
Additional risk factors for atherosclerosis[smoking and hypertension]
Additionally: they confer renoprotection through
Reduction of cell proliferation and mesangial matrix accumulation
Anti-inflammatory and immunomodulatory effects.
Recent studies: show as if they can reduce proteinuria and delay renal function loss.
40](https://image.slidesharecdn.com/glomerulonephritis-170330071106/85/Glomerulonephritis-40-320.jpg)

![Aka: nil disease/minimal-change disease
Absence of definitive pathologic changes observed under light
and immunofluorescence microscopy.
Commonly found in children
85% to 90% of all cases of nephrotic syndrome in children[1-4yrs]
2°Cause: drug (e.g., NSAIDs, lithium, interferons), lupus, and various T-
cell–related disorders, such as Hodgkin’s disease and leukemias.
Frequently acute in onset
Minimal-Change Nephropathy
Aka: nil disease/minimal-change disease
Absence of definitive pathologic changes observed under light
and immunofluorescence microscopy.
Commonly found in children
85% to 90% of all cases of nephrotic syndrome in children[1-4yrs]
2°Cause: drug (e.g., NSAIDs, lithium, interferons), lupus, and various T-
cell–related disorders, such as Hodgkin’s disease and leukemias.
Frequently acute in onset
42](https://image.slidesharecdn.com/glomerulonephritis-170330071106/85/Glomerulonephritis-42-320.jpg)