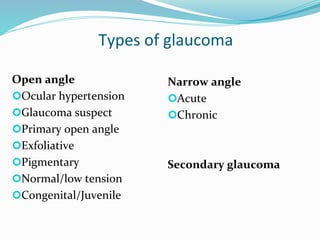
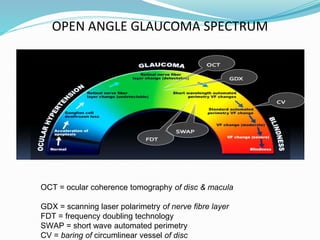
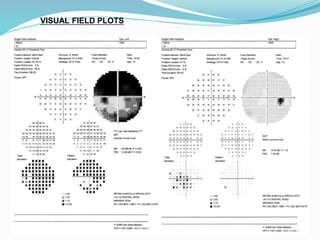
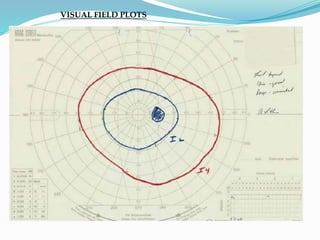
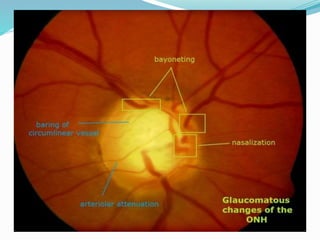
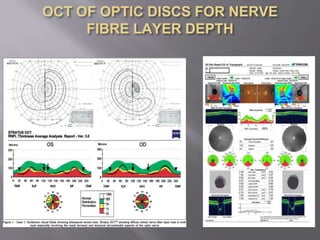
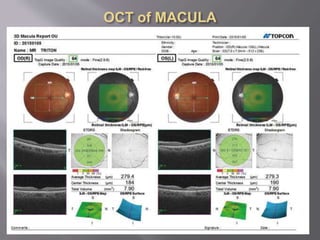
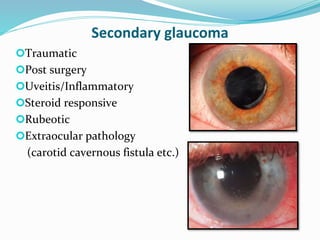
Glaucoma can be open angle or closed angle. Open angle glaucoma includes ocular hypertension, glaucoma suspect, primary open angle, exfoliative, pigmentary, normal/low tension, and congenital/juvenile types. It is assessed using visual field testing, intraocular pressure measurement, gonioscopy, optic disc examination, and imaging like OCT. Treatment involves eye drops like prostaglandin analogs, beta blockers, and surgeries like trabeculectomy. Monitoring intervals depend on whether pressure and disease are controlled. Primary angle closure glaucoma is less common but riskier, requiring treatment like laser iridotomy.