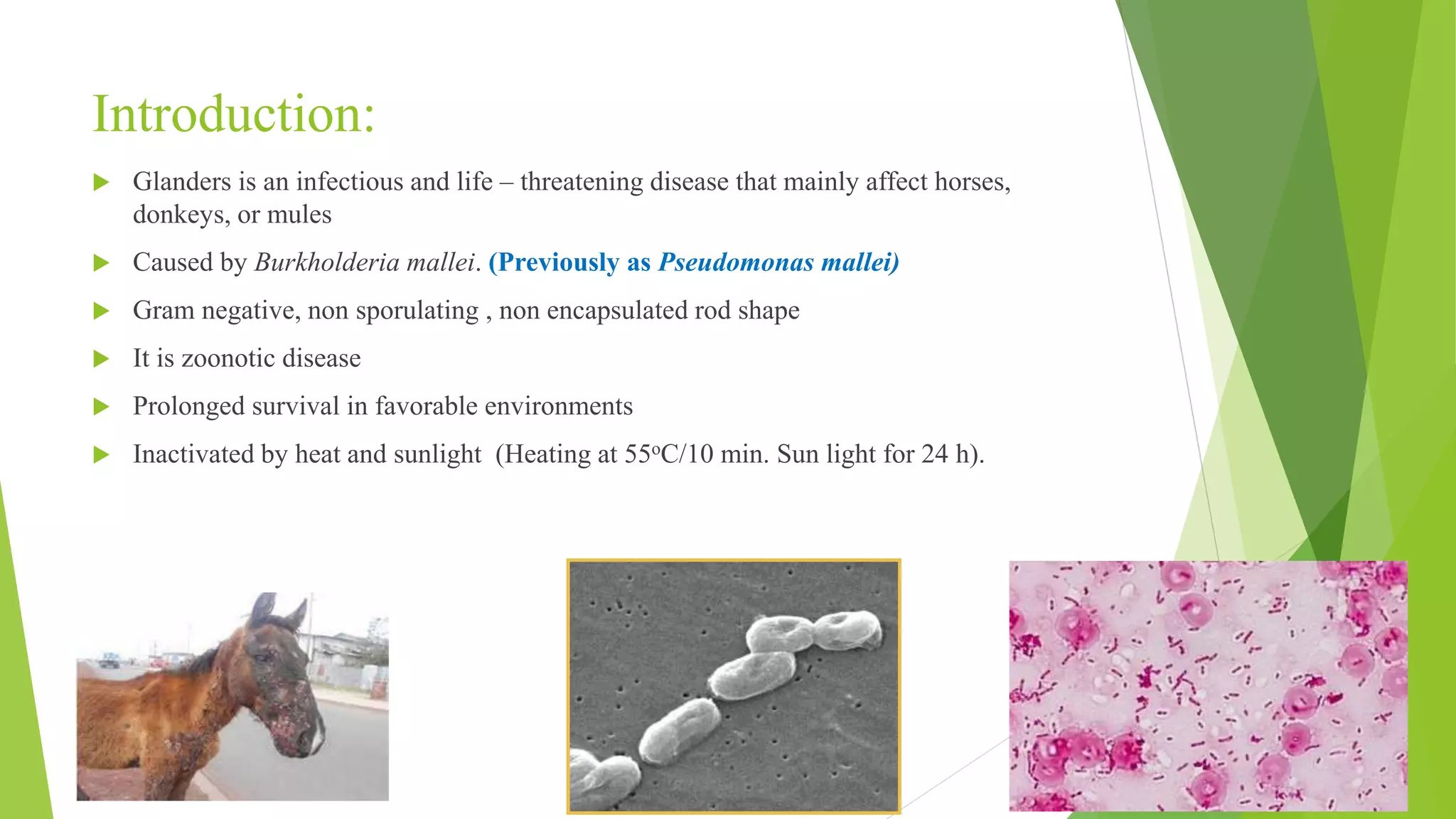
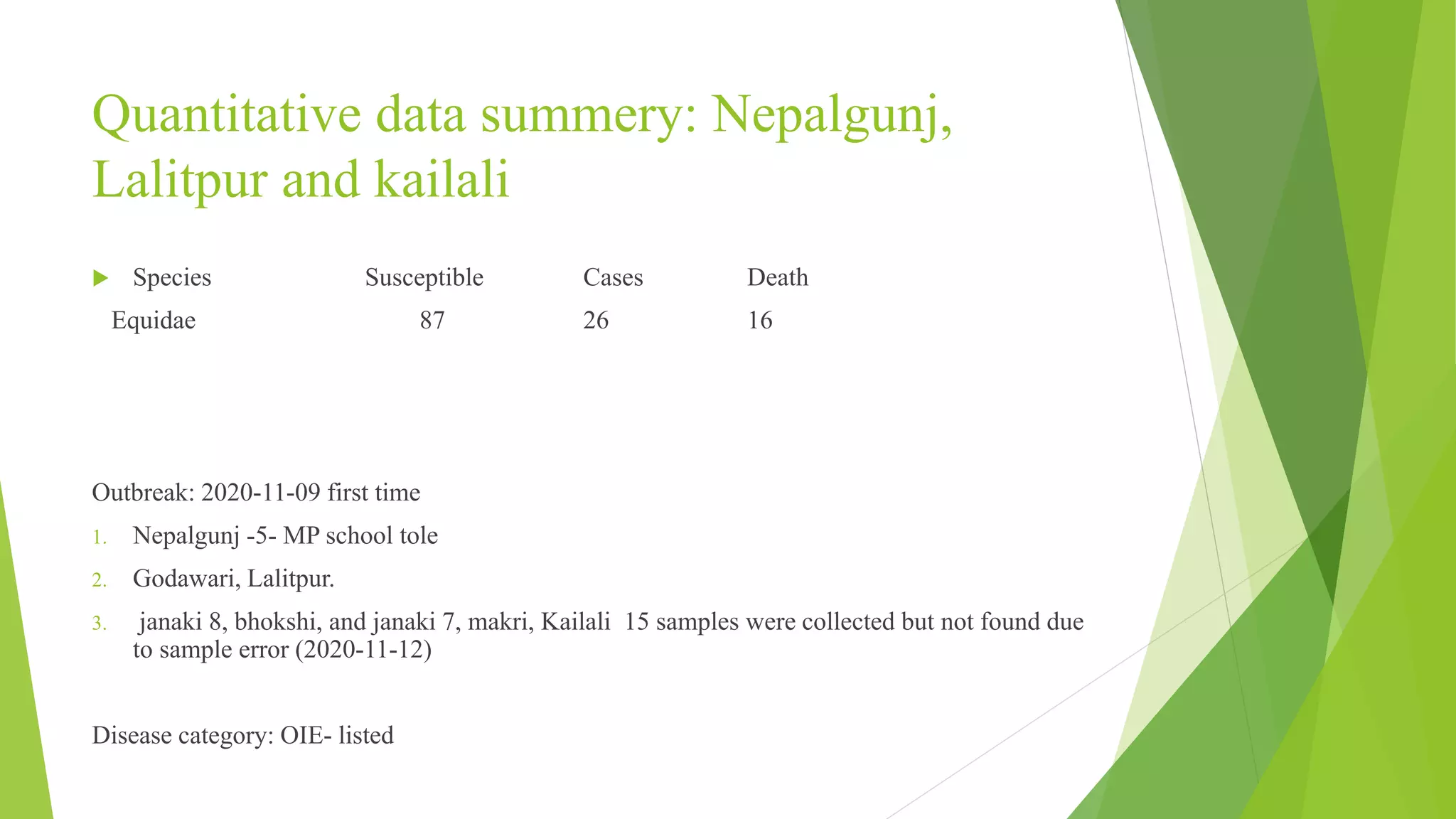
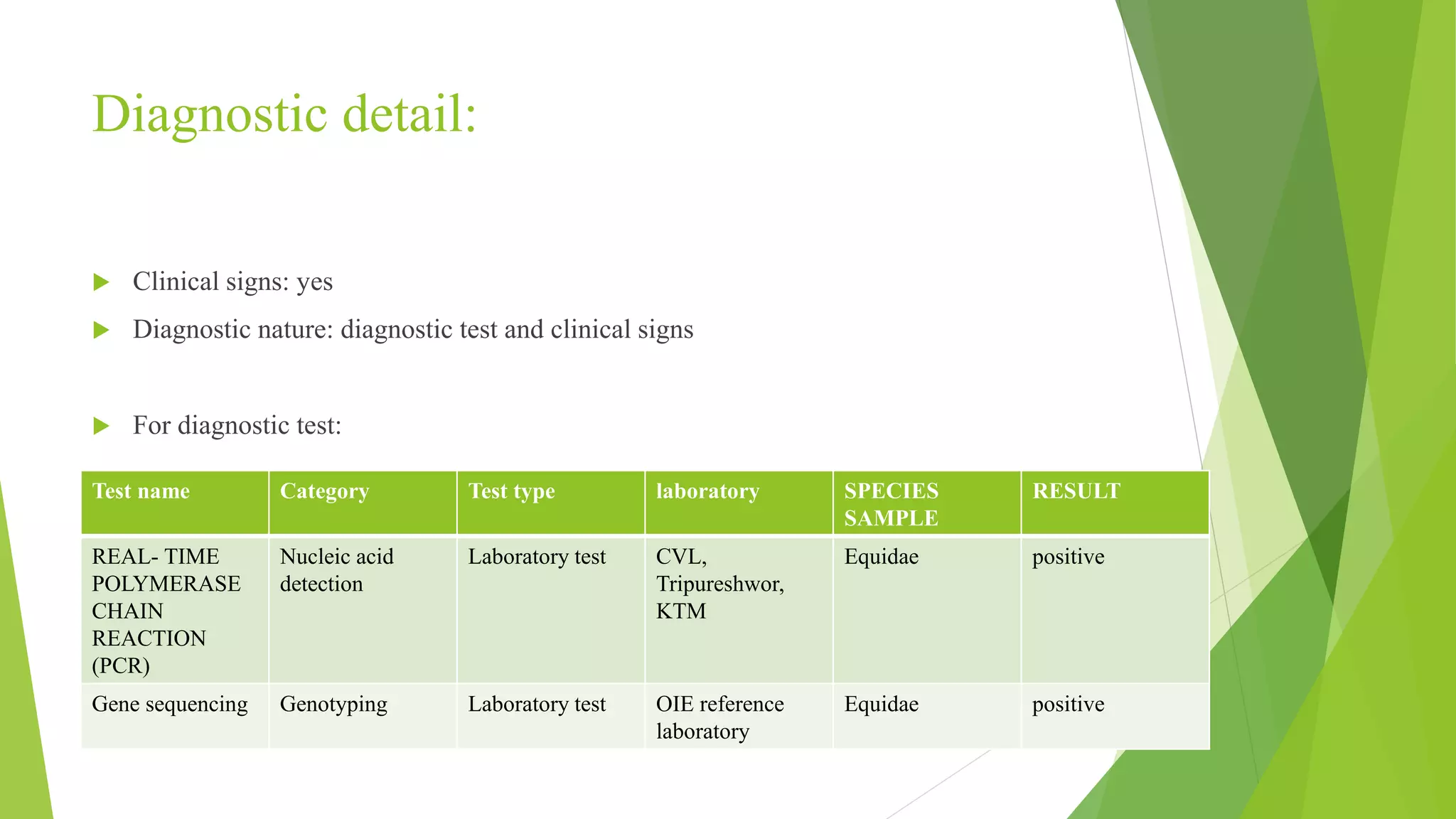
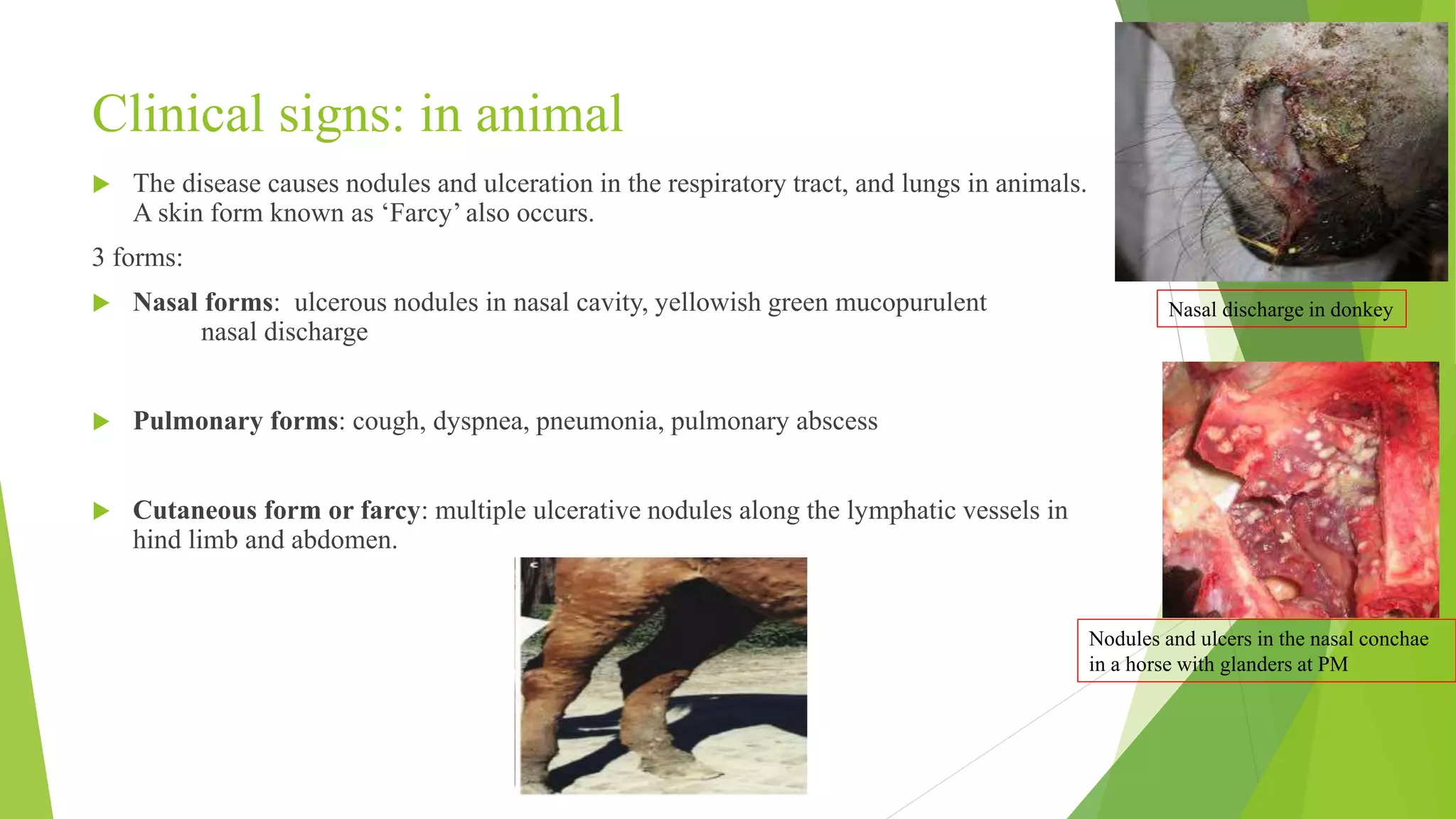
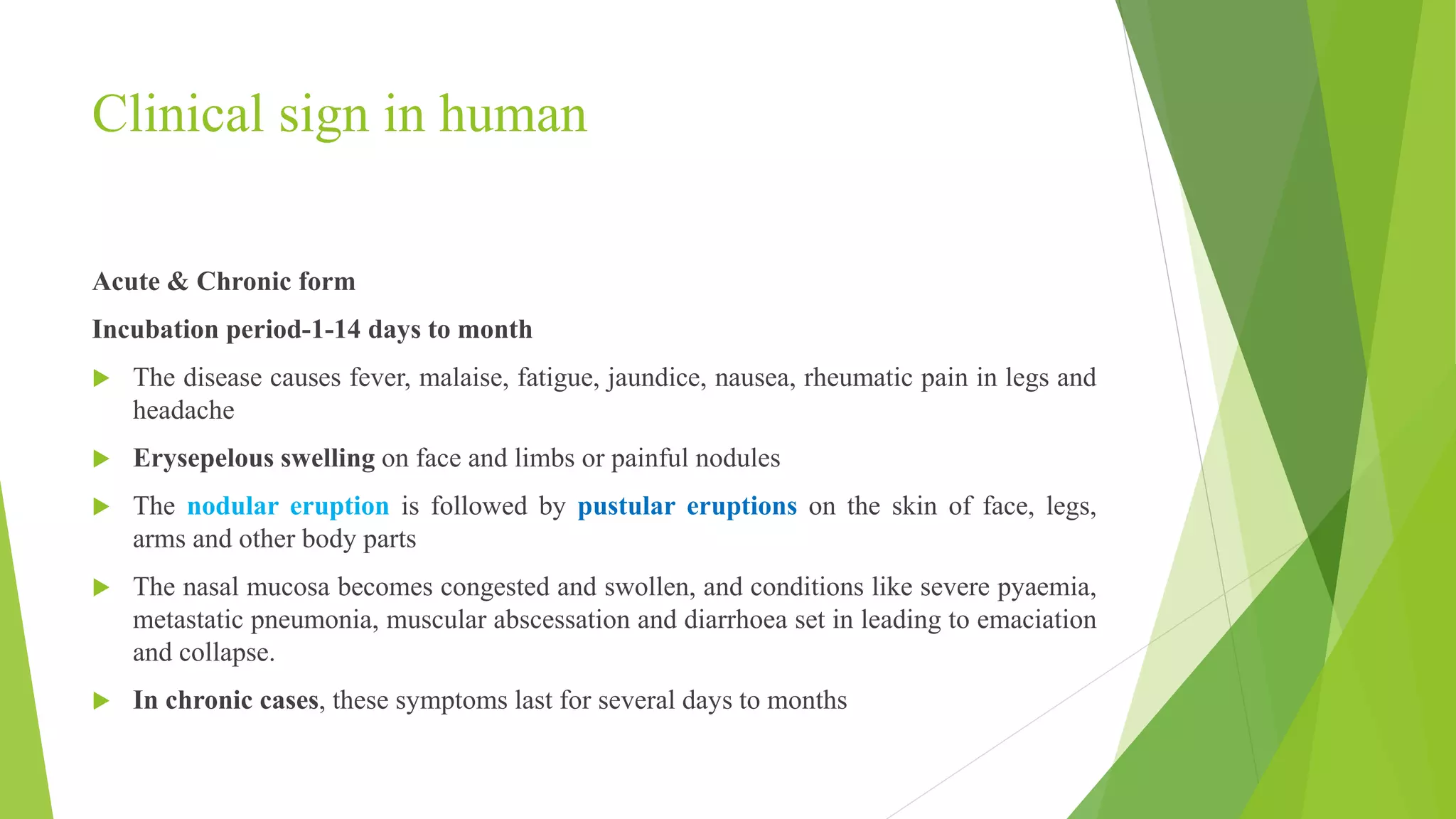
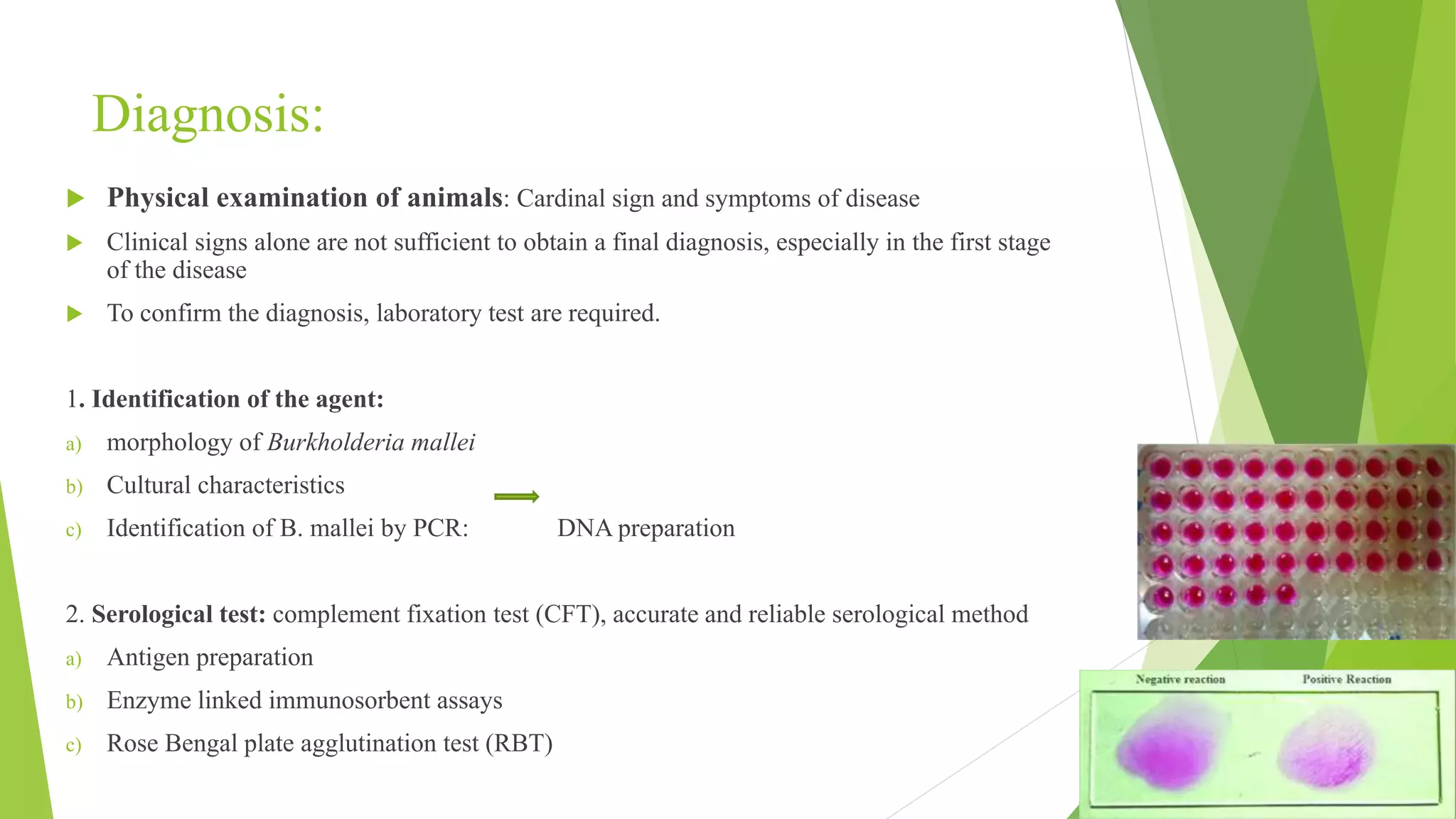
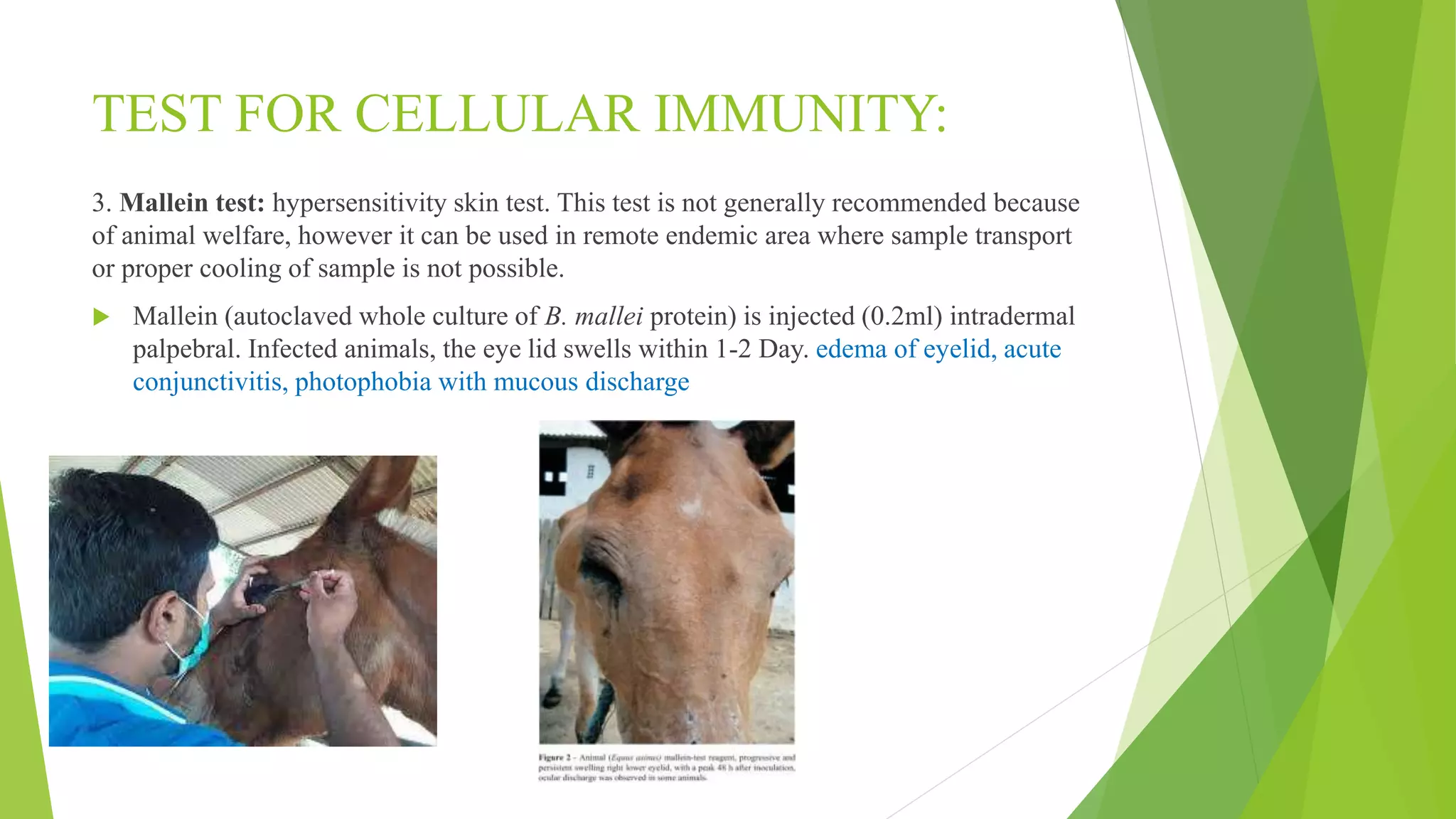
Glanders, caused by the bacterium Burkholderia mallei, is a life-threatening zoonotic disease primarily affecting horses, donkeys, and mules, with its first occurrence reported in Nepal in November 2020. The disease is diagnosed through clinical signs and laboratory tests, poses significant public health risks, and has no existing vaccine, with treatment possible only if administered quickly. Control measures involve early detection, quarantine, and public education to prevent transmission to humans.