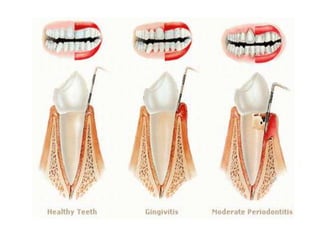
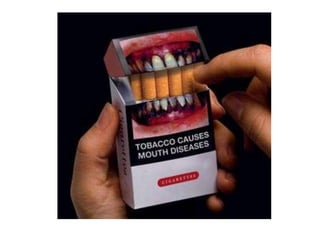
Gingivitis is a non-destructive periodontal disease caused by bacterial biofilms (plaque) on tooth surfaces. It is characterized by swollen, red or purple gums that bleed easily. While gingivitis is reversible with improved oral hygiene, it can progress to periodontitis if left untreated. Risk factors include poor oral hygiene, smoking, stress, certain medical conditions and medications. Gingivitis is treated by removing the bacterial plaque through regular brushing, flossing and professional cleanings.