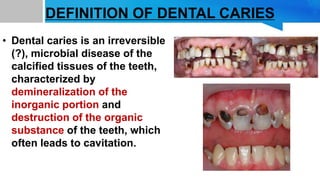
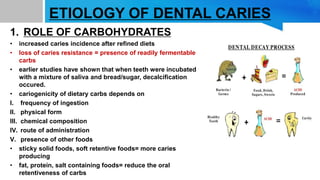
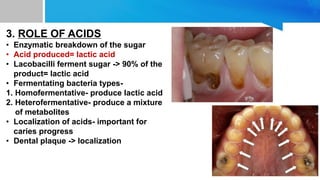
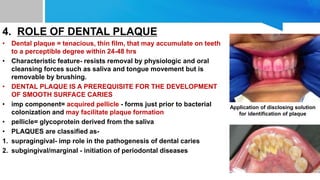
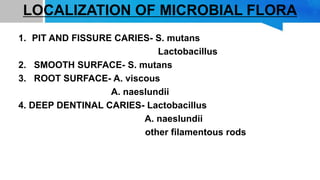
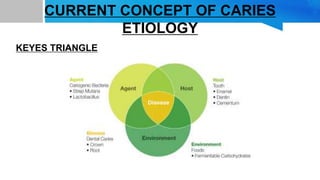
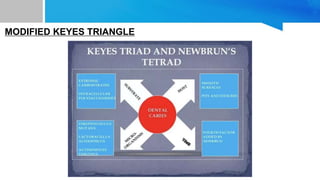
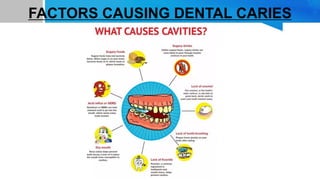
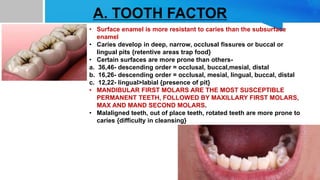
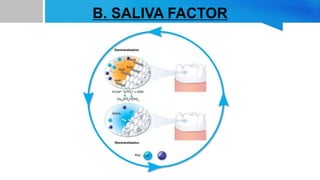
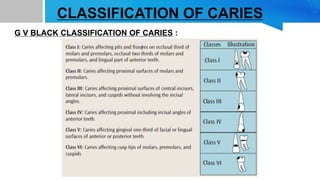
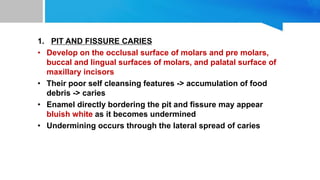
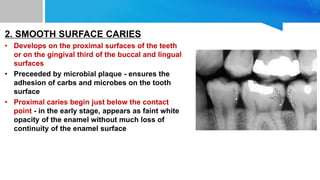
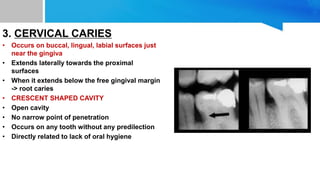
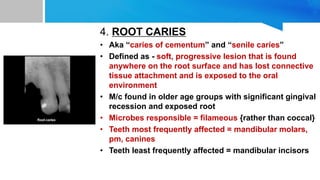
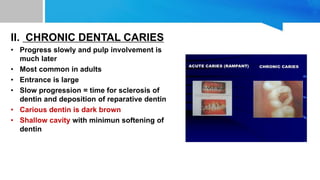
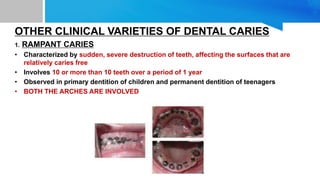
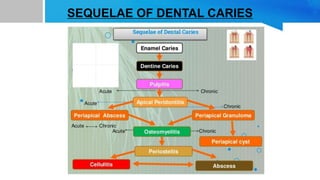
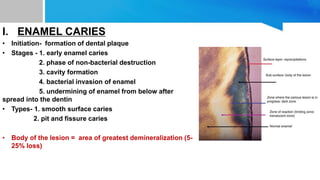
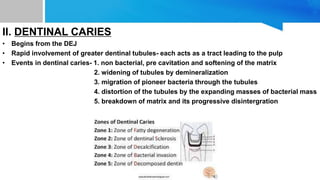
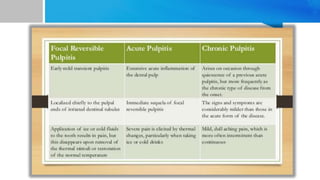
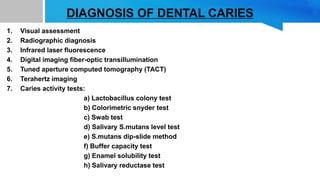
Dental caries is an irreversible microbial disease affecting tooth tissues, characterized by demineralization and cavitation due to factors like age, race, and diet. Key contributors to caries include carbohydrates, microorganisms (especially Streptococcus mutans), and dental plaque, with various classifications of caries based on their location and progression. Management of dental caries focuses on prevention through hygiene, diet, and fluoride application, and restorative treatments are required once cavities form.