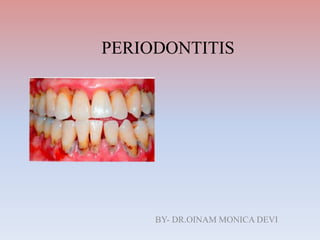
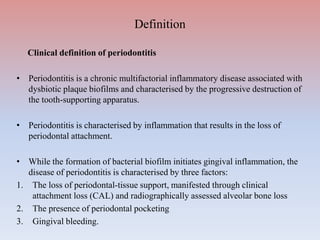
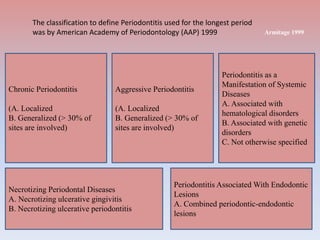
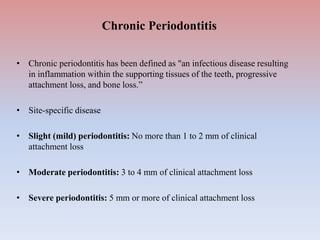
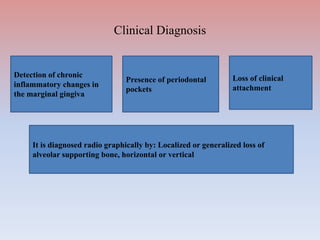
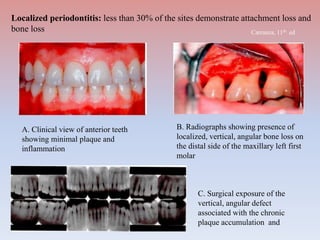
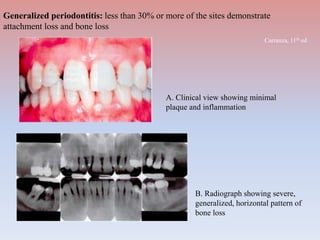
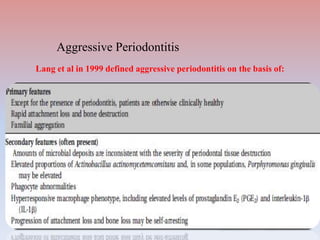
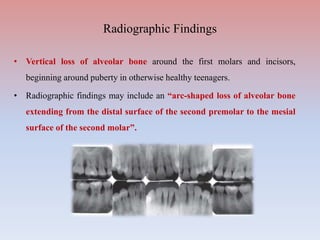
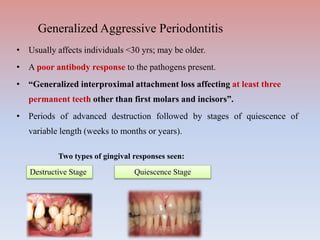
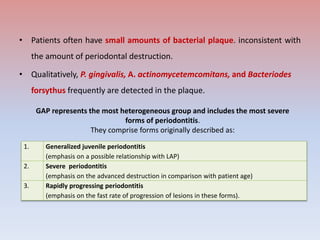
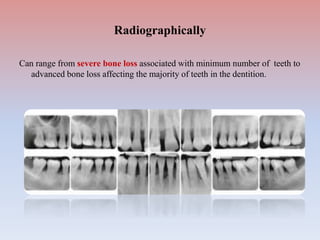
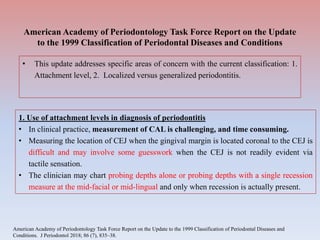
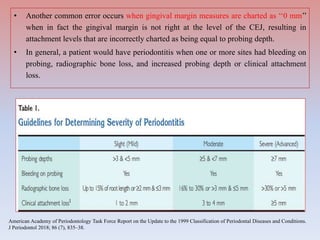
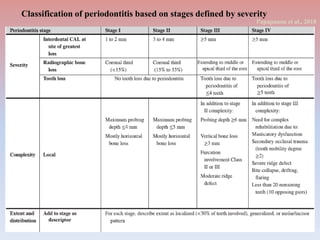
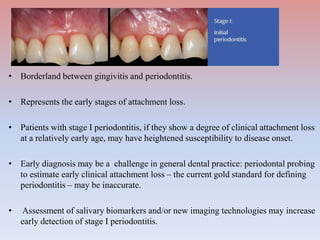
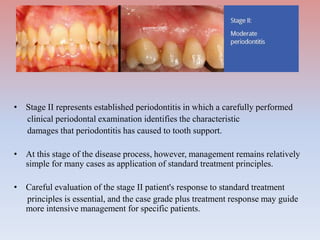
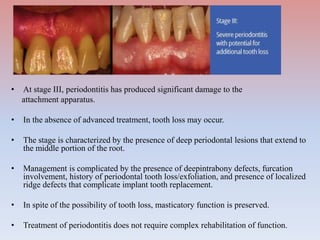
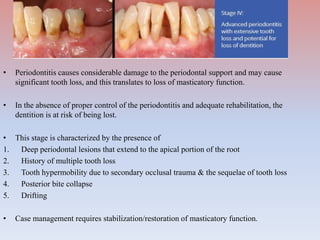
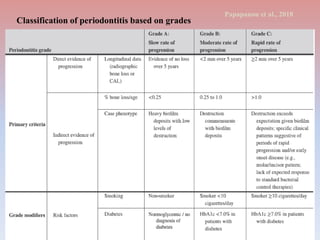
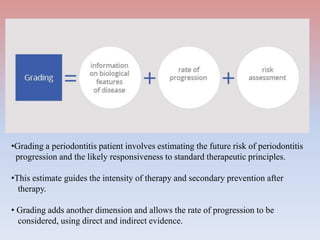
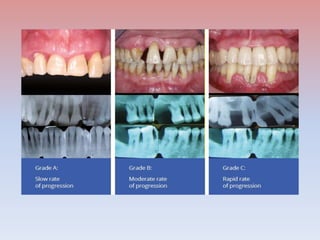
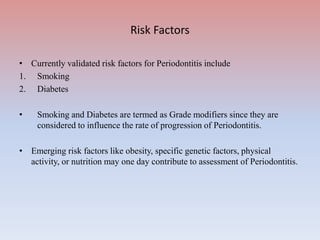
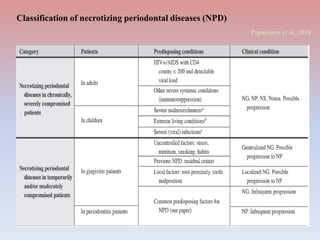
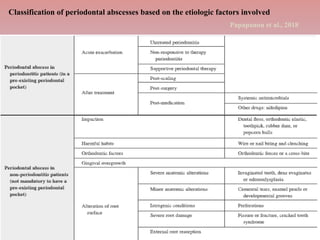
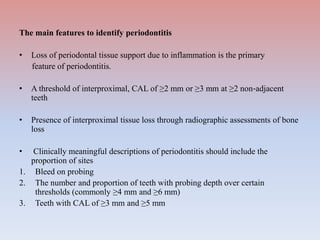
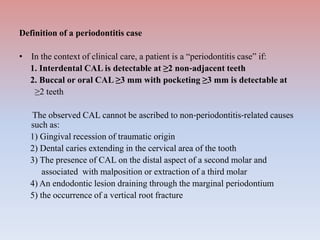
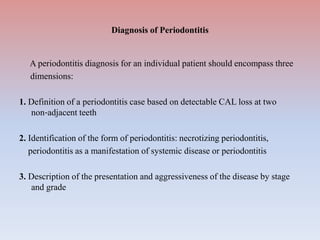
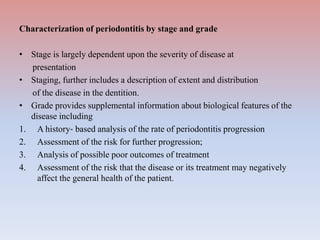
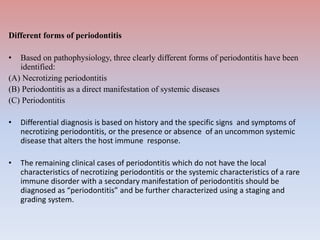
The document provides a comprehensive overview of periodontitis, defining it as a chronic inflammatory disease marked by the destruction of the tooth-supporting apparatus due to dysbiotic plaque biofilms. It presents various classifications of periodontitis, including chronic and aggressive types, diagnosis criteria based on clinical attachment loss, and the latest updates to classification systems based on severity and grade. Key features for diagnosis and management of periodontitis are detailed, alongside risk factors and distinctions between different forms of periodontal diseases.