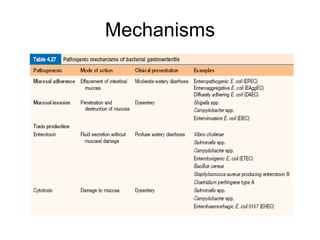
The most common causes of bacterial gastroenteritis worldwide include Salmonella, Campylobacter, Shigella, EHEC, Vibrio, Yersinia, Staph aureus, and Bacillus cereus. Vibrio cholerae causes cholera, which results in a massive secretion of fluid into the intestinal lumen through the release of toxins. Clostridium difficile infection is a common cause of antibiotic-associated diarrhea.