This document provides an overview of cardiac physiology, including:
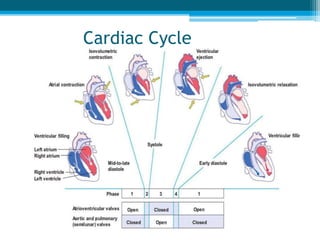
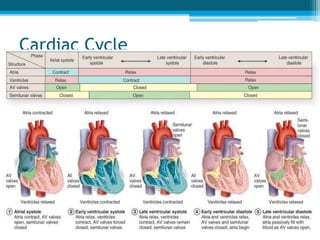
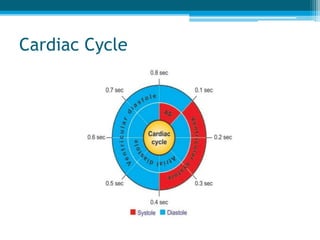
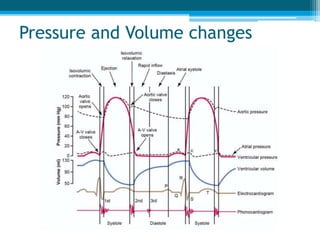
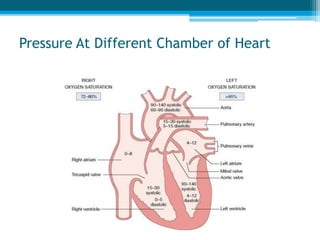
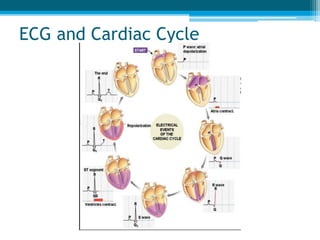
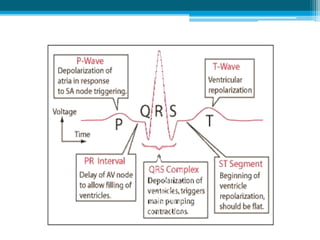
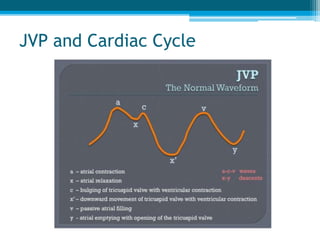
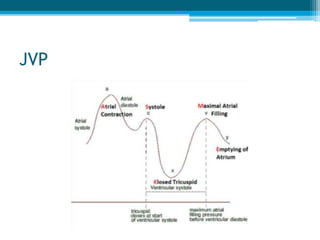
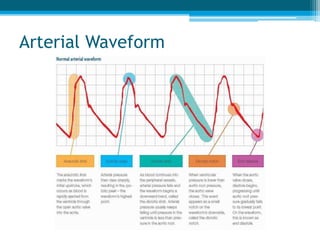
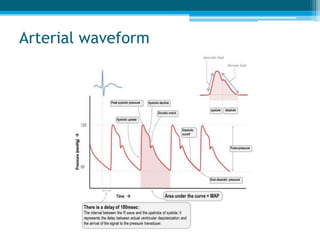
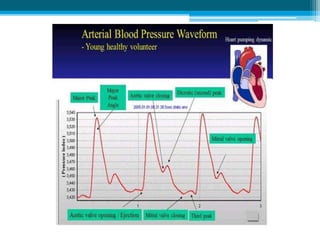
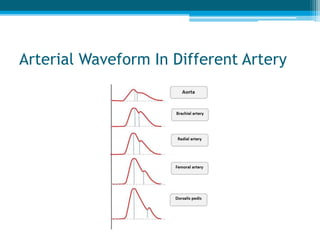
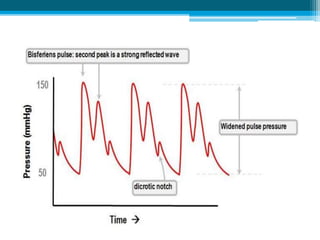
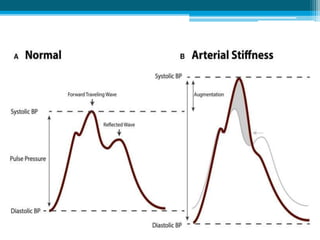
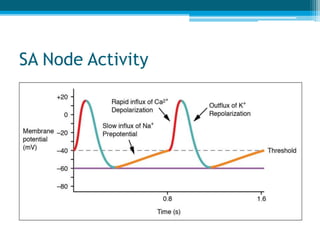
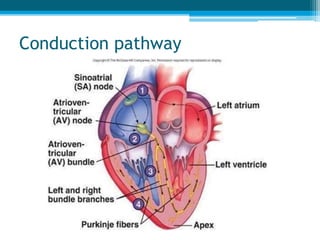
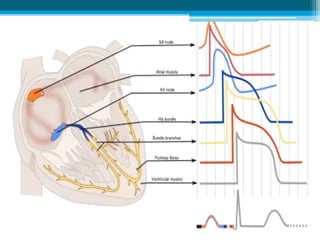
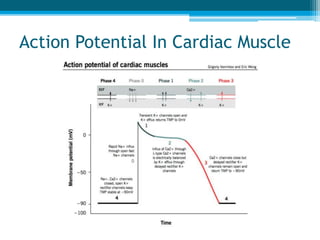
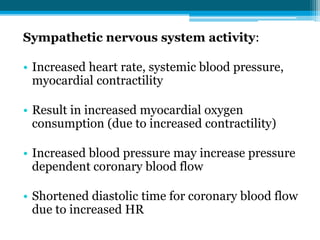
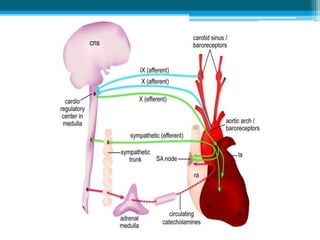
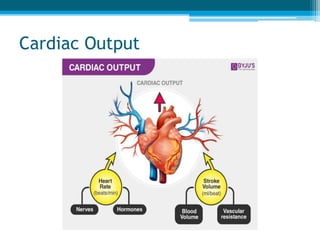
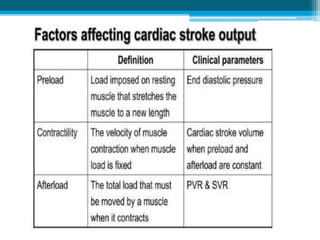
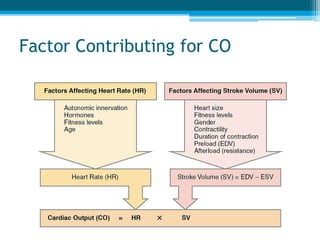
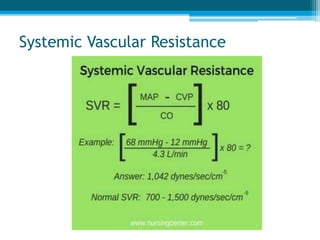
1) It discusses the cardiac cycle, electrical activity of the heart, arterial waveforms, and factors that influence cardiac output and blood pressure regulation.
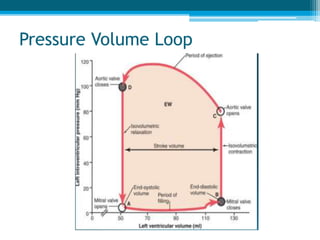
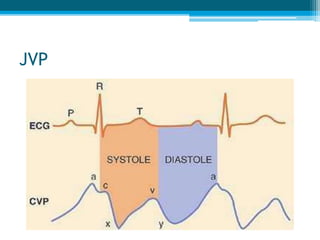
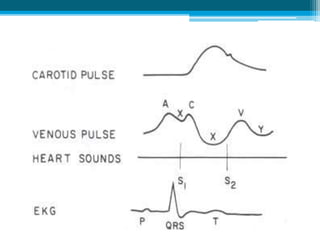
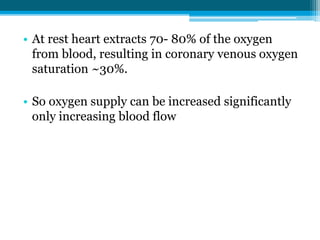
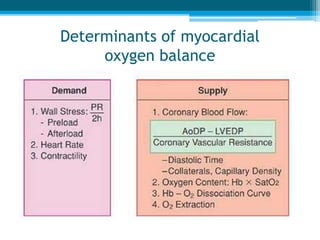
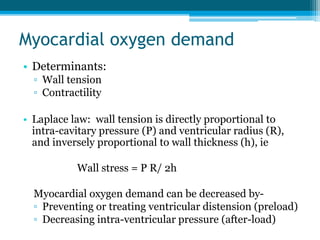
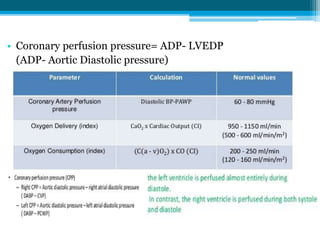
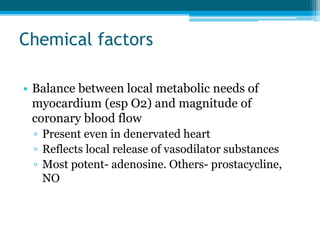
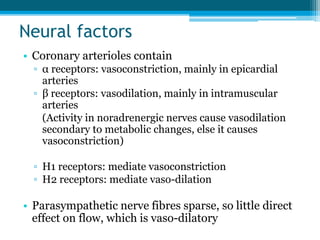
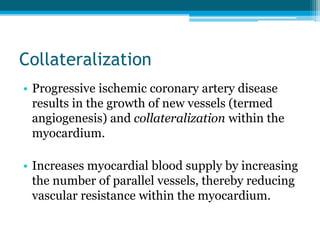
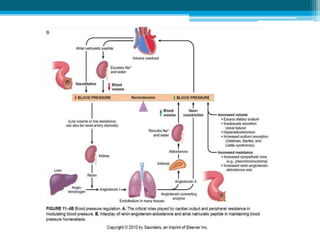
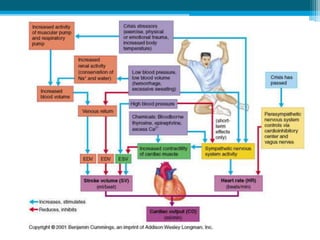
2) It covers topics like the pressure-volume loop, ECG, JVP, coronary circulation, oxygen demand and supply, and mechanisms that control blood pressure both short and long term.
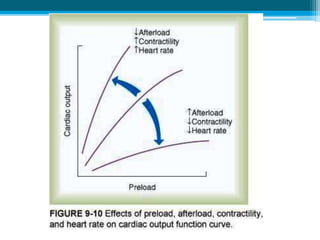
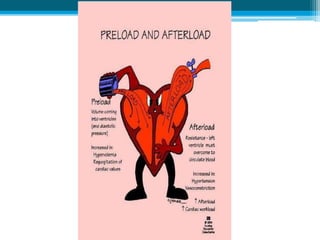
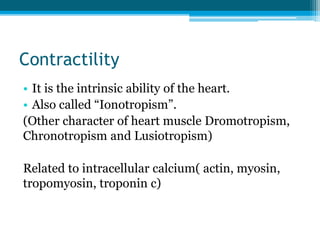
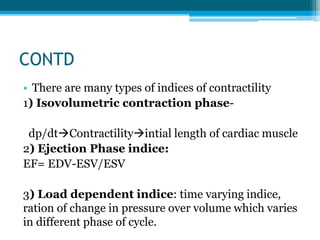
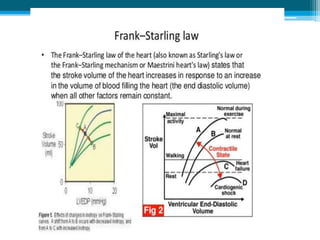
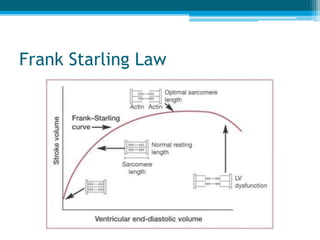
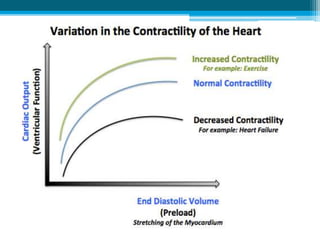
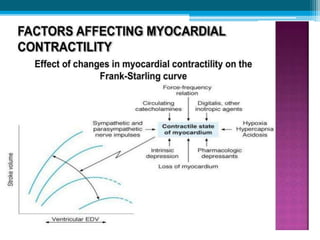
3) It addresses cardiac contractility, factors that influence cardiac output, and the relationship between cardiac output, blood pressure, and systemic vascular resistance as dictated by the Frank-Starling Law.