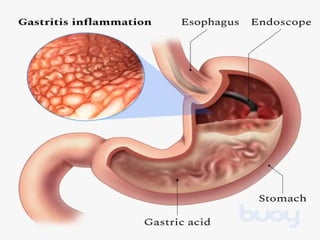
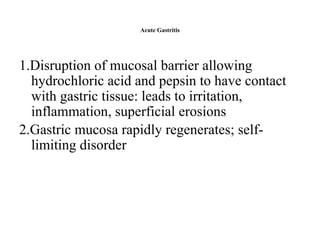
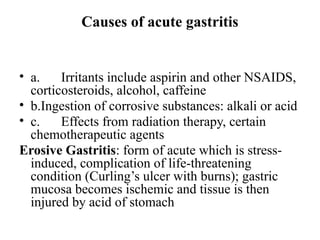
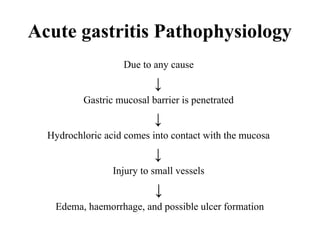
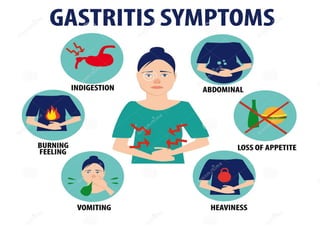
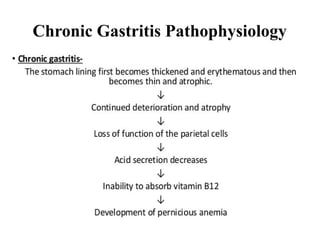
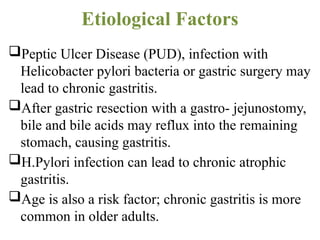
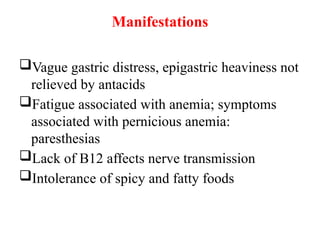
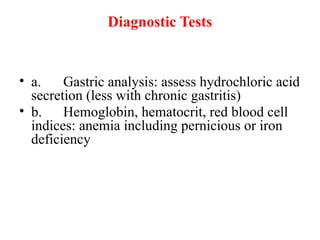
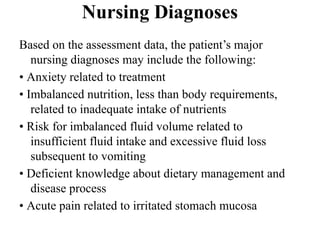
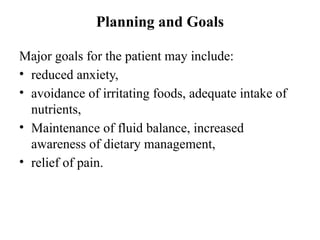
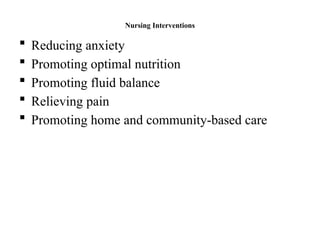
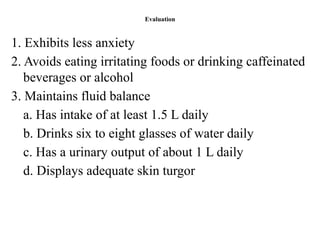
The document provides an in-depth examination of gastritis, covering its causes, pathophysiology, symptoms, diagnostics, and treatment strategies, including nursing management. It differentiates between acute and chronic gastritis, detailing the roles of irritants, infections like Helicobacter pylori, and the significance of dietary management. The nursing process emphasizes assessment, planning, intervention, and evaluation to ensure patient care and education.