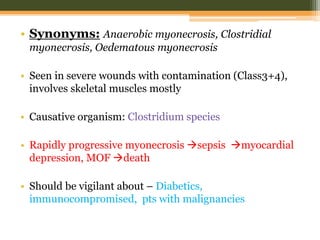
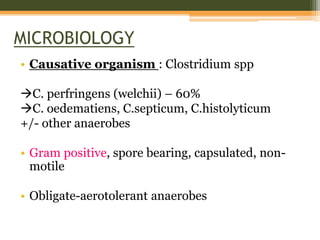
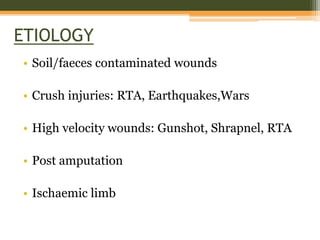
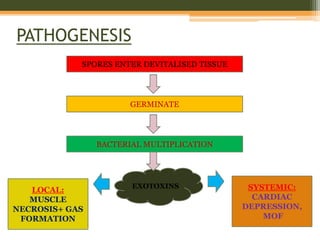
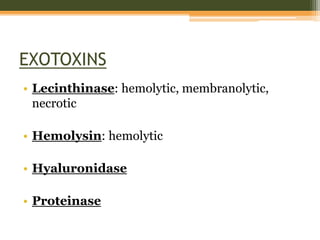
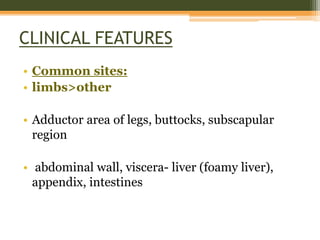
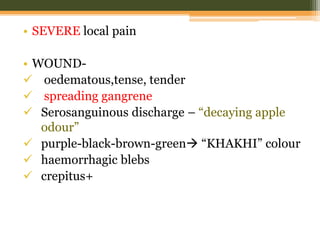
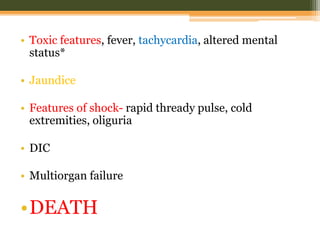
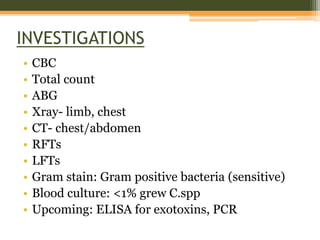
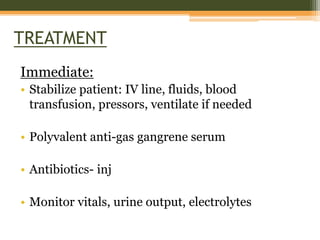
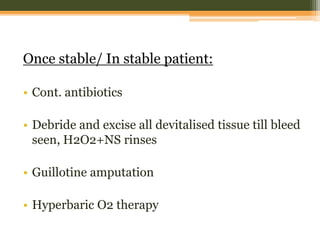
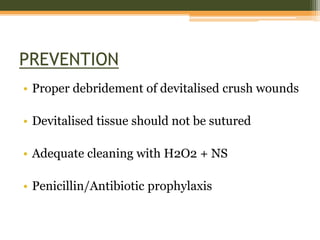
Gas gangrene is caused by Clostridium bacteria entering wounds contaminated with soil or feces. It results in rapid muscle necrosis and toxin production. Clinical features include severe local pain, wound edema and gangrene spreading from the original site. Systemic effects can include shock, organ failure and death. Treatment requires antibiotics, debridement of devitalized tissue, and sometimes amputation. Prevention focuses on thorough wound cleaning and debridement to remove contaminants and devitalized tissue.