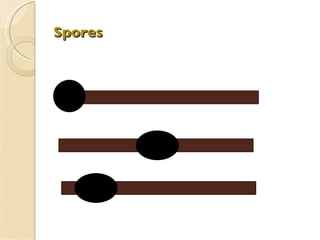
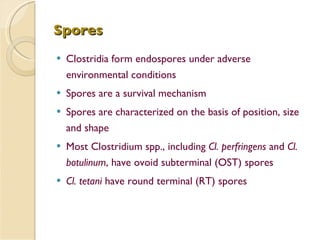
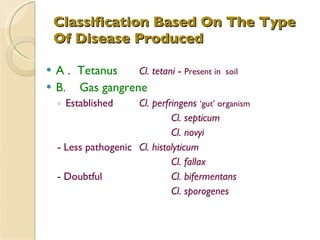
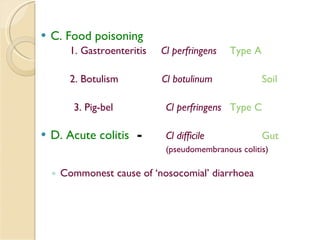
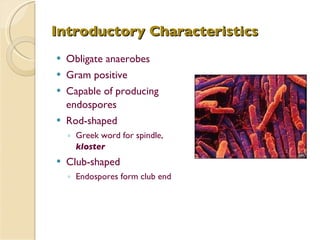
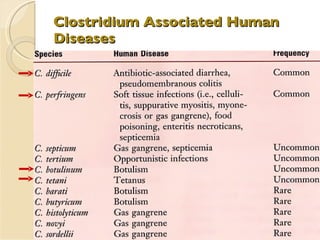
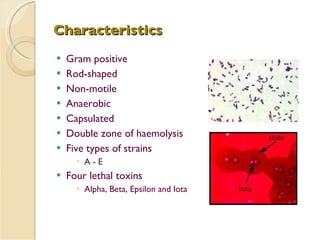
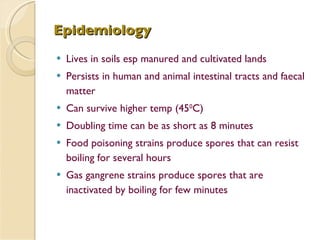
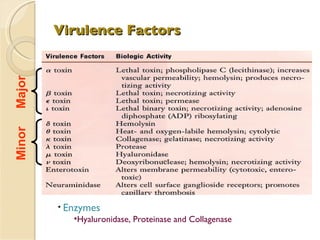
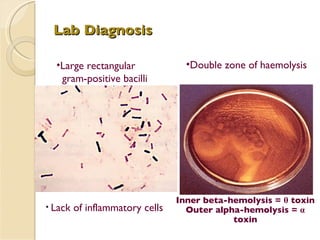
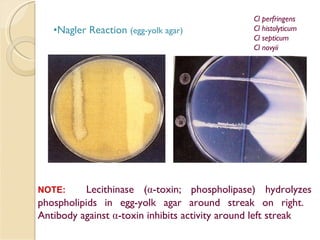
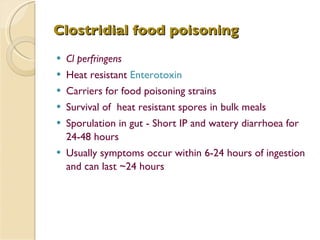
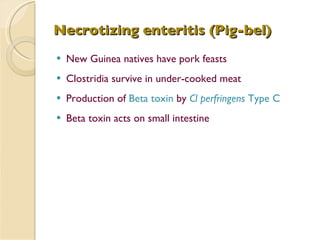
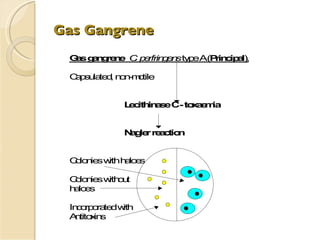
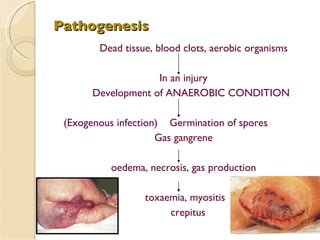
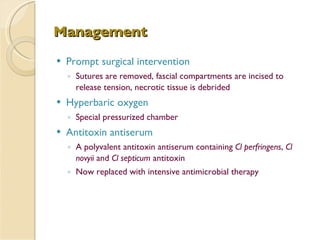
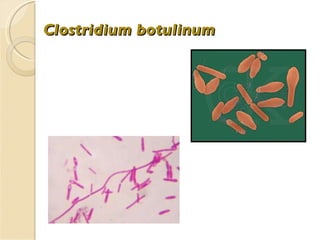
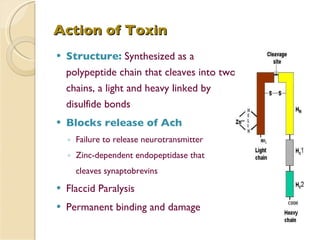
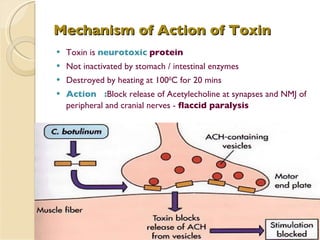
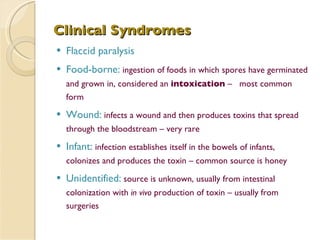
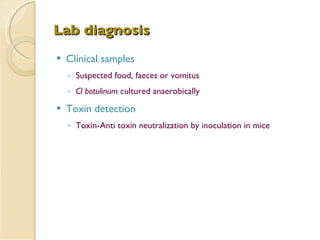
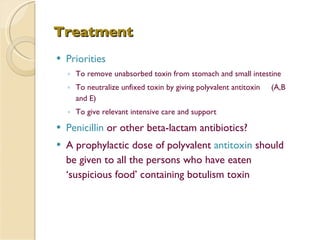
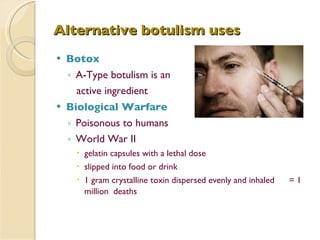
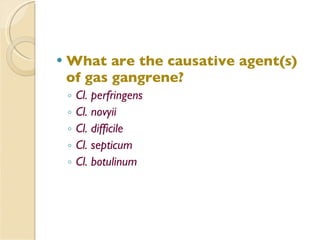
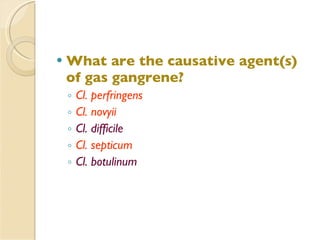
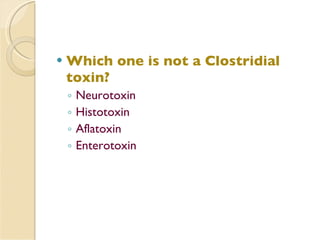
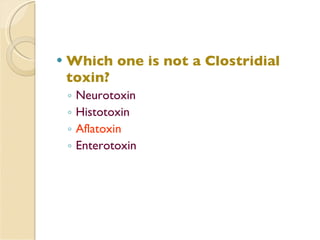
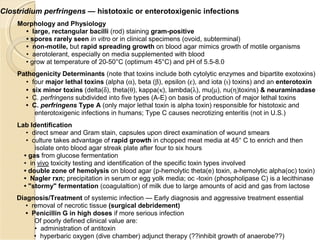
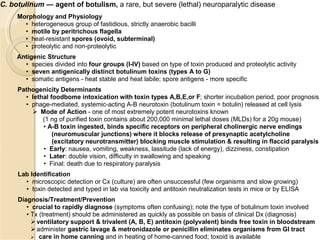
The document discusses several Clostridium species including C. perfringens, C. botulinum, C. tetani. It covers their characteristics, virulence factors, diseases caused like gas gangrene, food poisoning, botulism. Management includes prompt surgery, antitoxins, antibiotics for C. perfringens. C. botulinum toxin blocks acetylcholine release causing flaccid paralysis. Its toxin is neutralized by antitoxin.