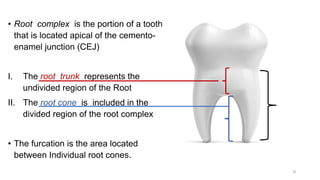
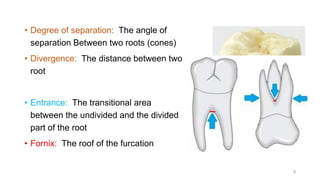
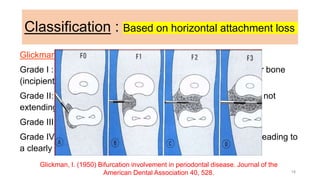
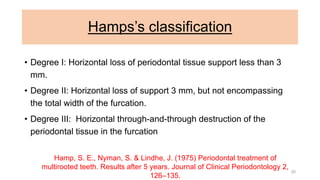
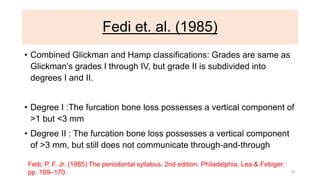
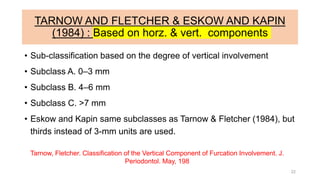
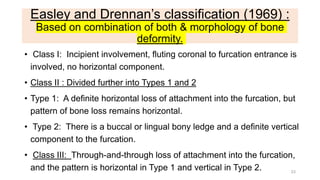
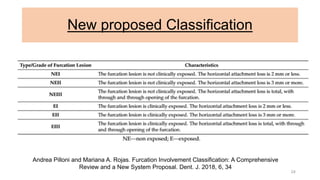
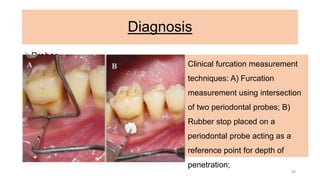
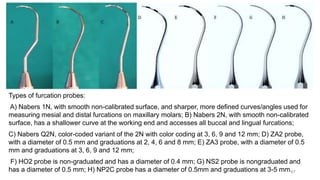
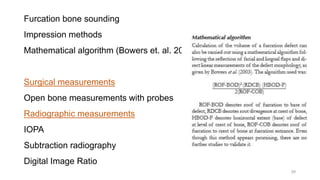
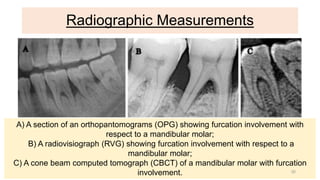
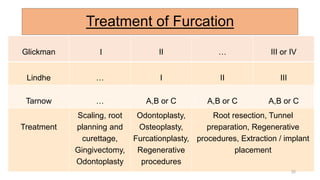
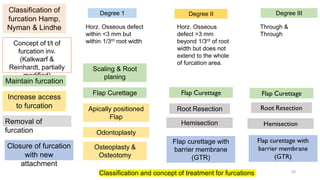
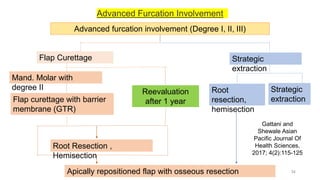
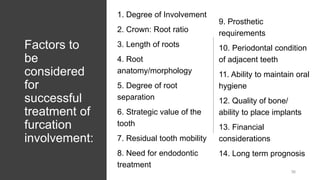
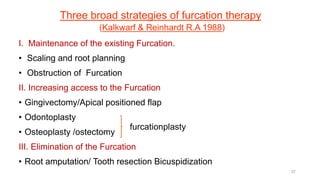
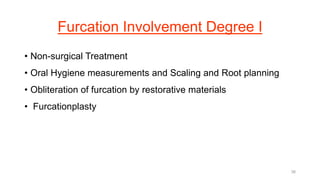
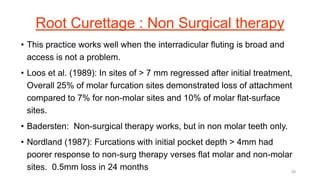
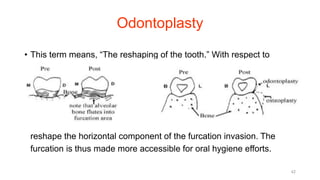
The document discusses furcation involvement, which refers to periodontal disease that affects the connection between roots in multi-rooted teeth. It defines furcation, presents various classification systems for grading the severity of furcation involvement, and outlines methods for diagnosing and treating furcation lesions. The management of furcation involvement depends on the grade or class and involves non-surgical and surgical approaches ranging from scaling and root planing to regenerative procedures and tooth extraction.