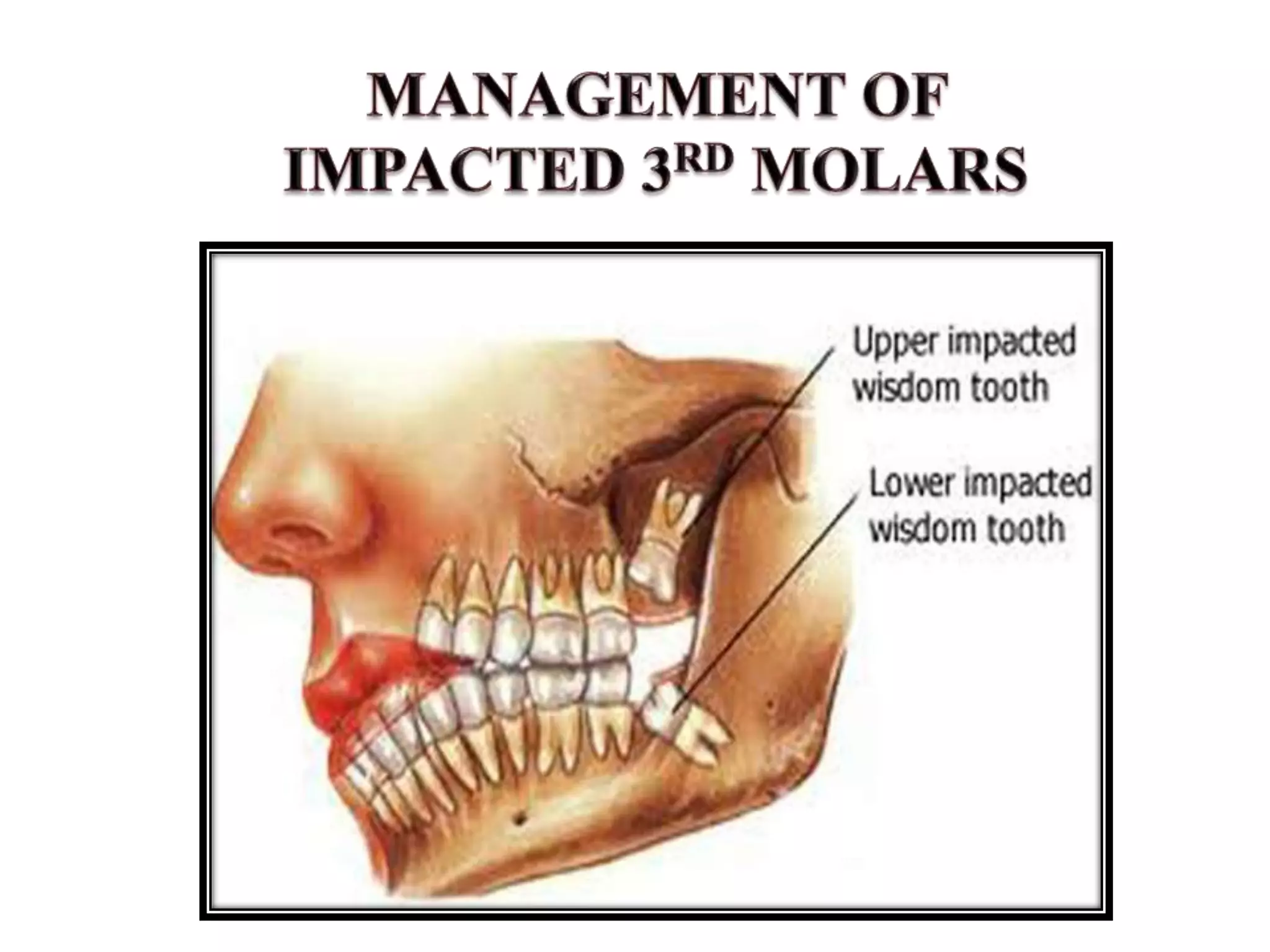
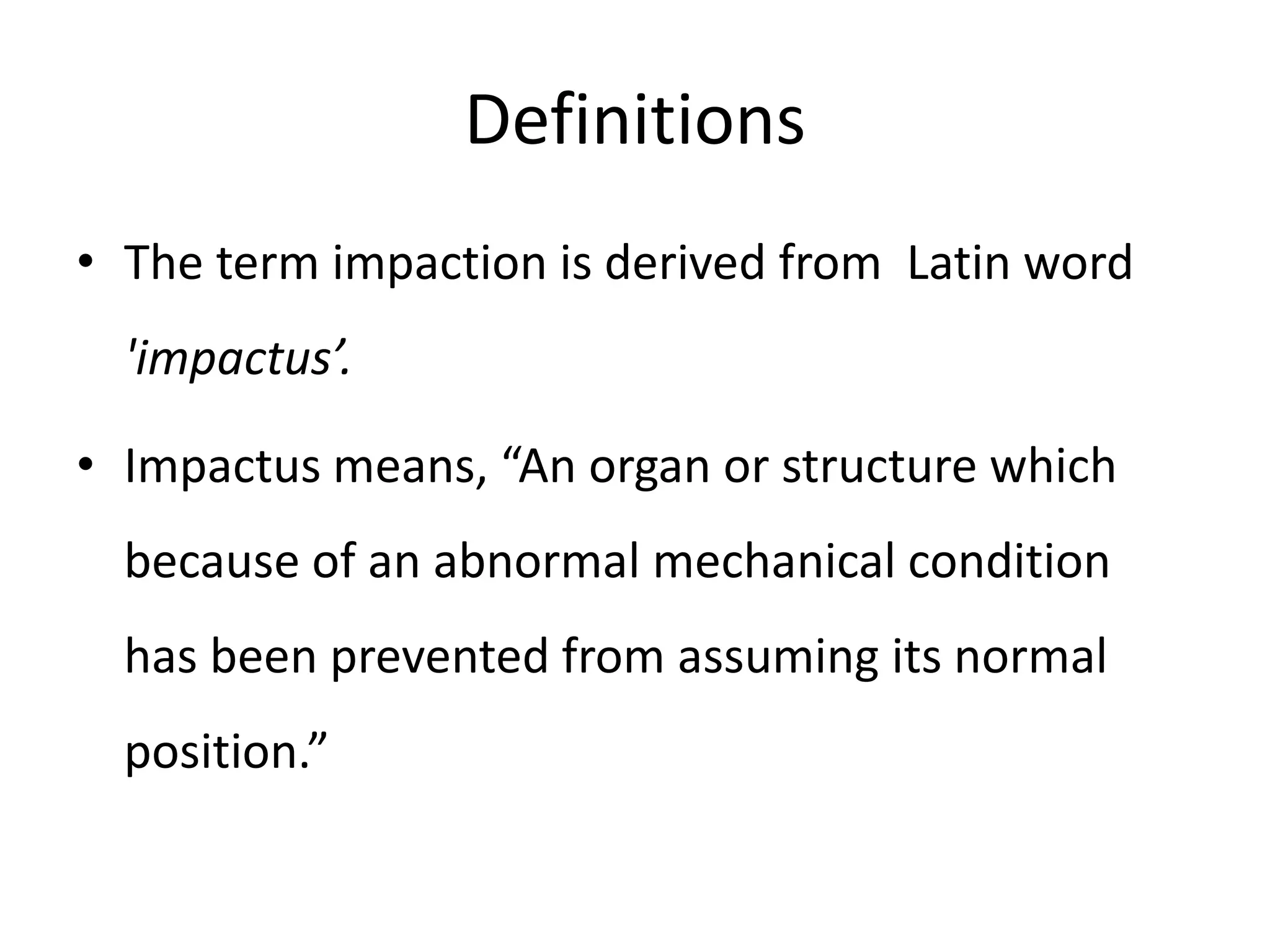
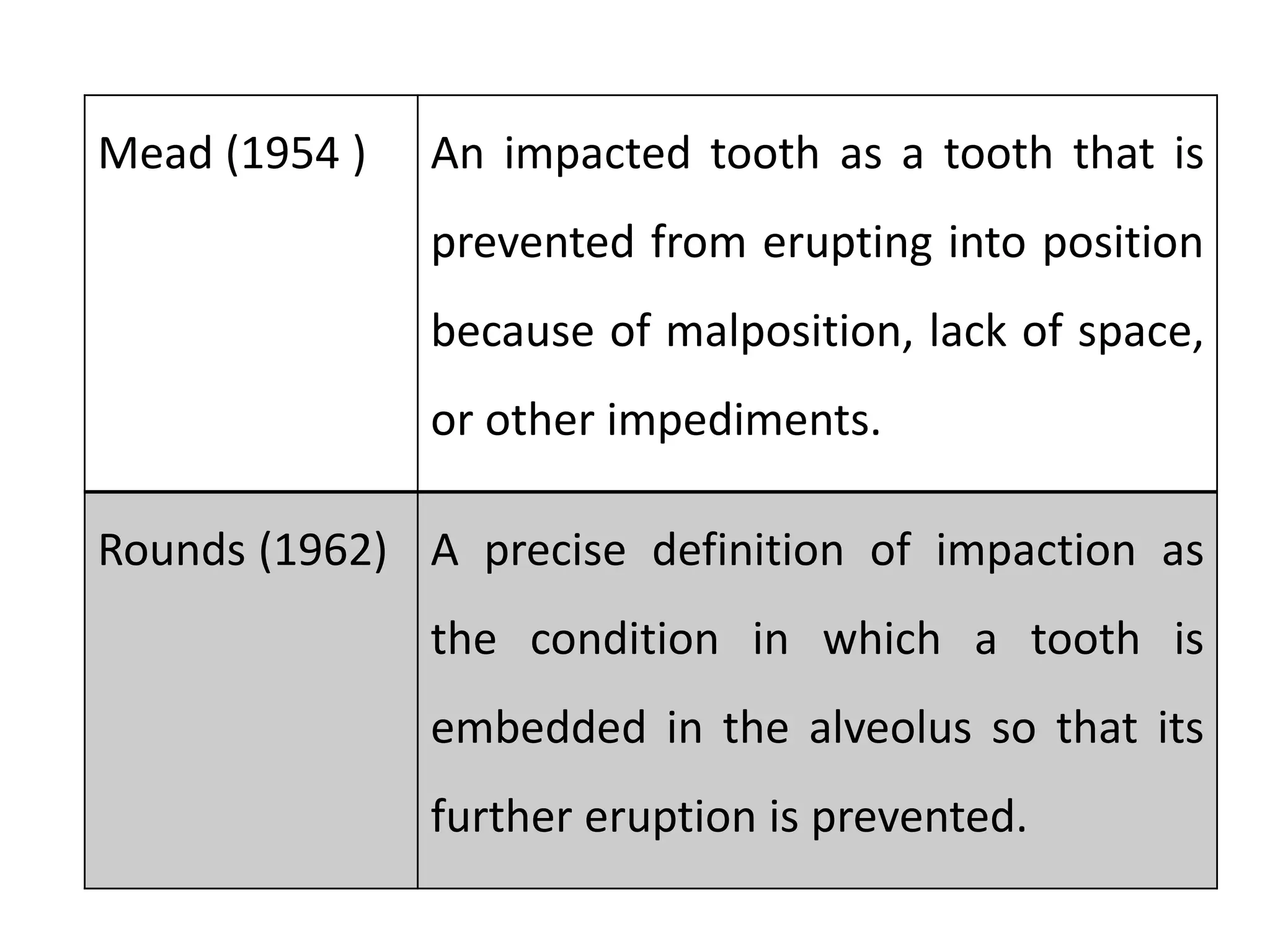
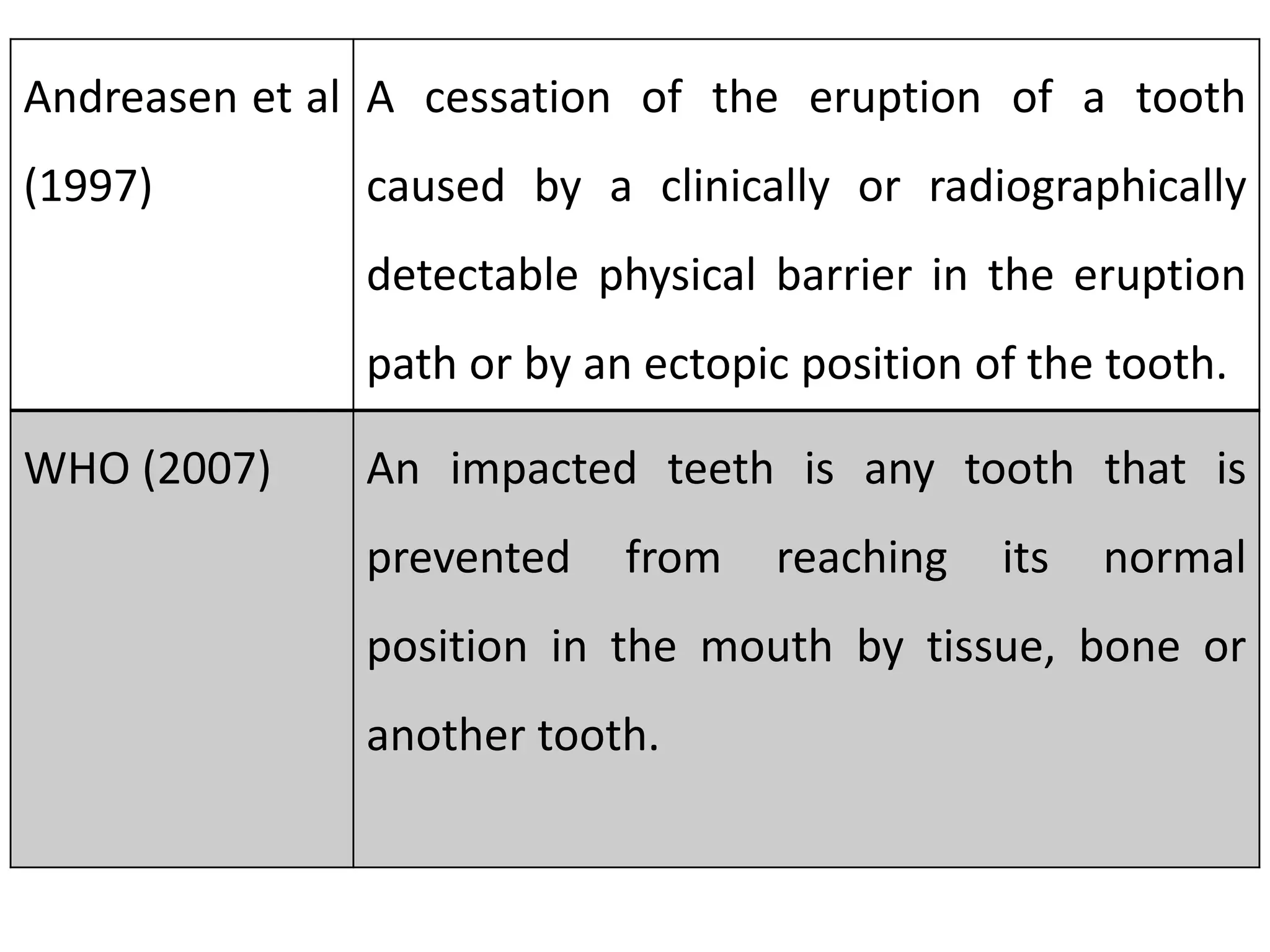
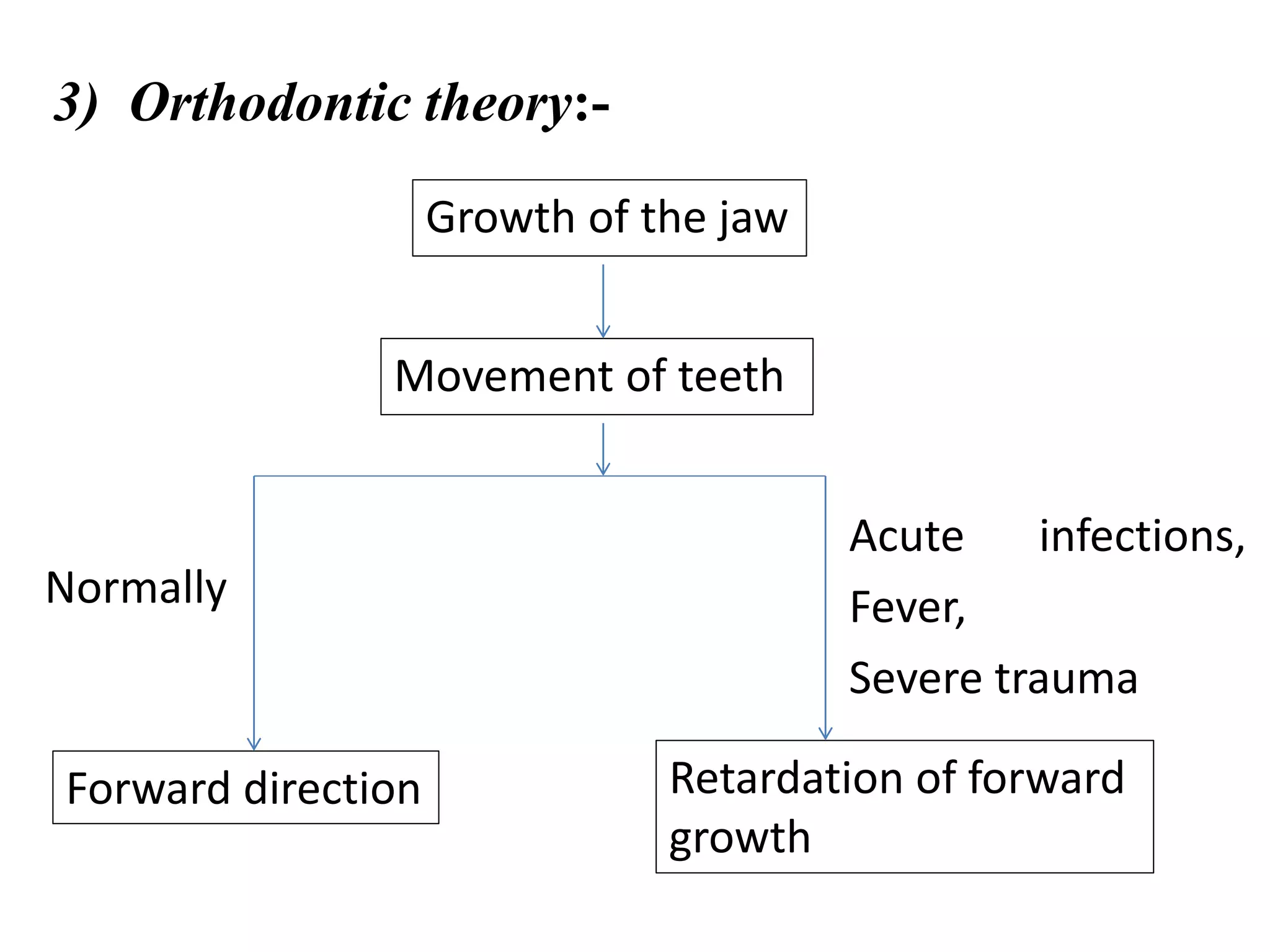
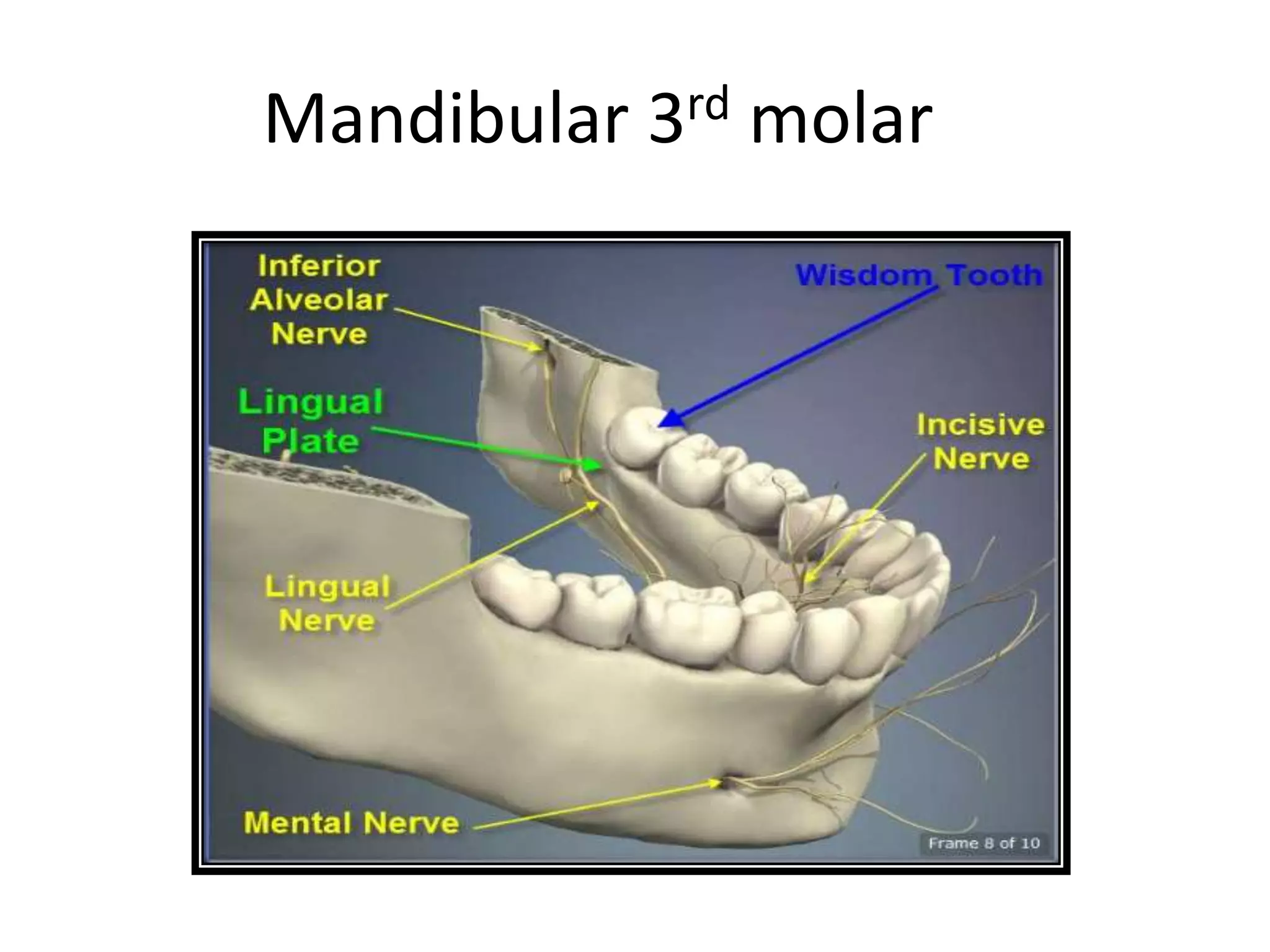
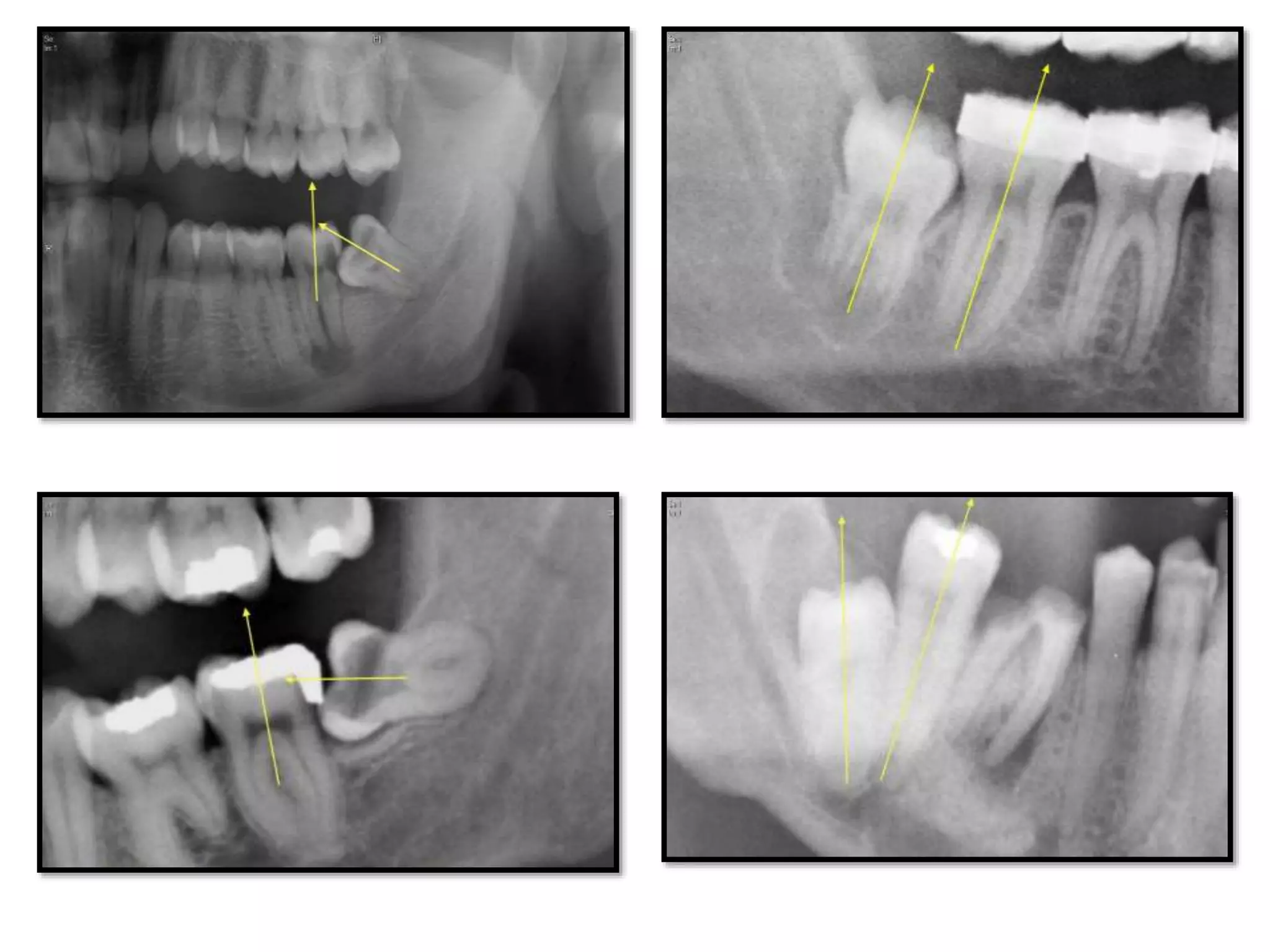
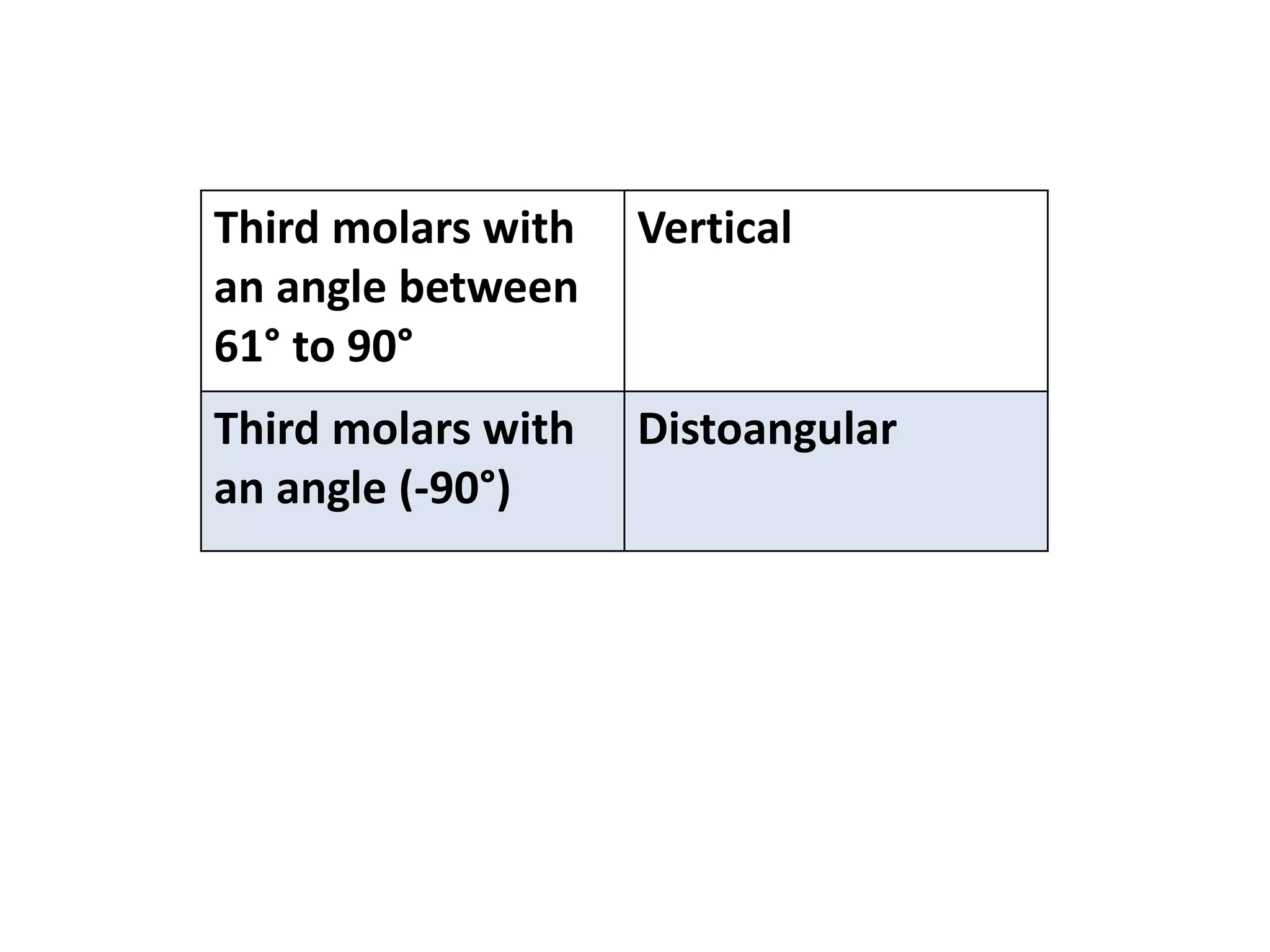
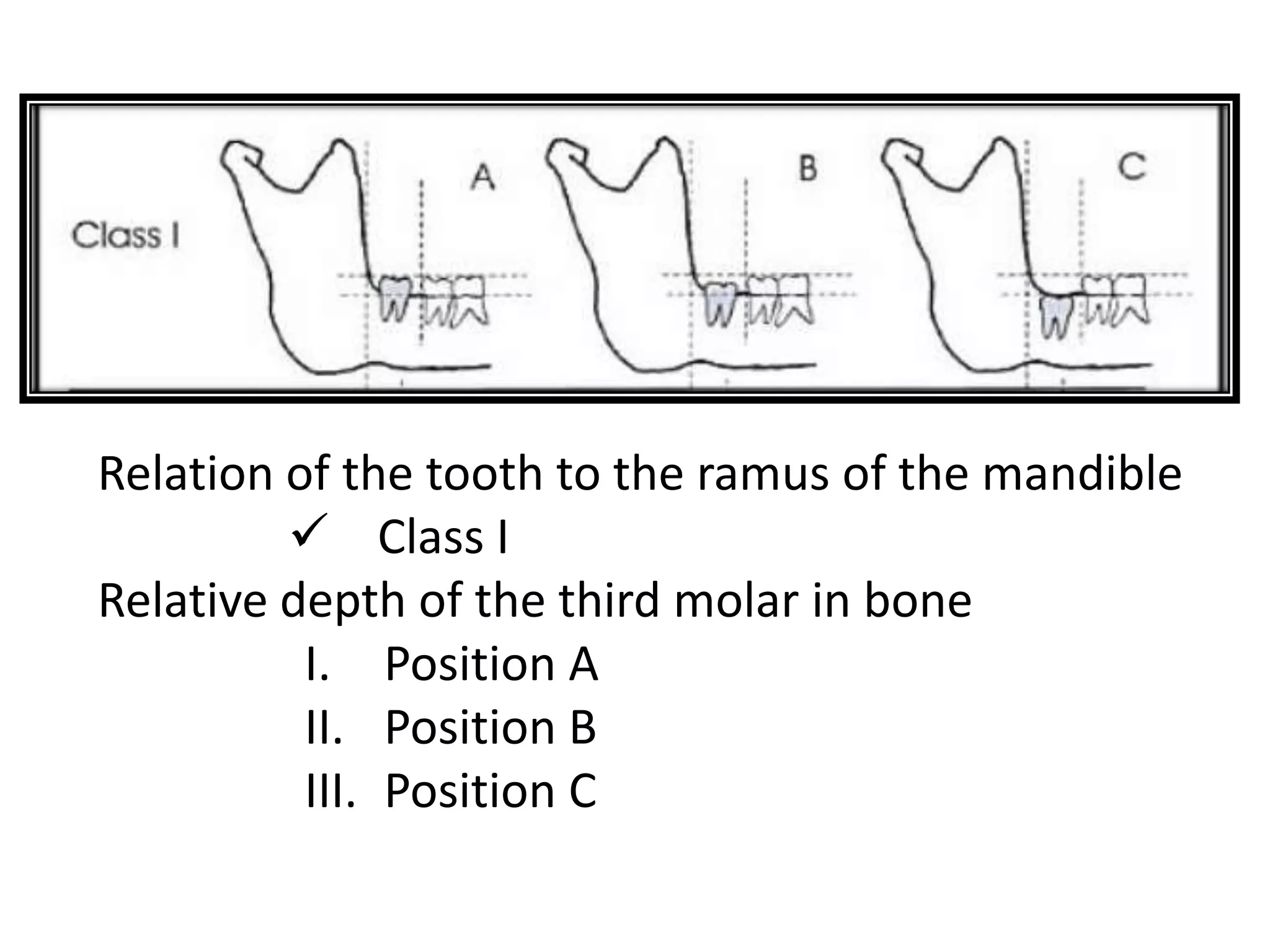
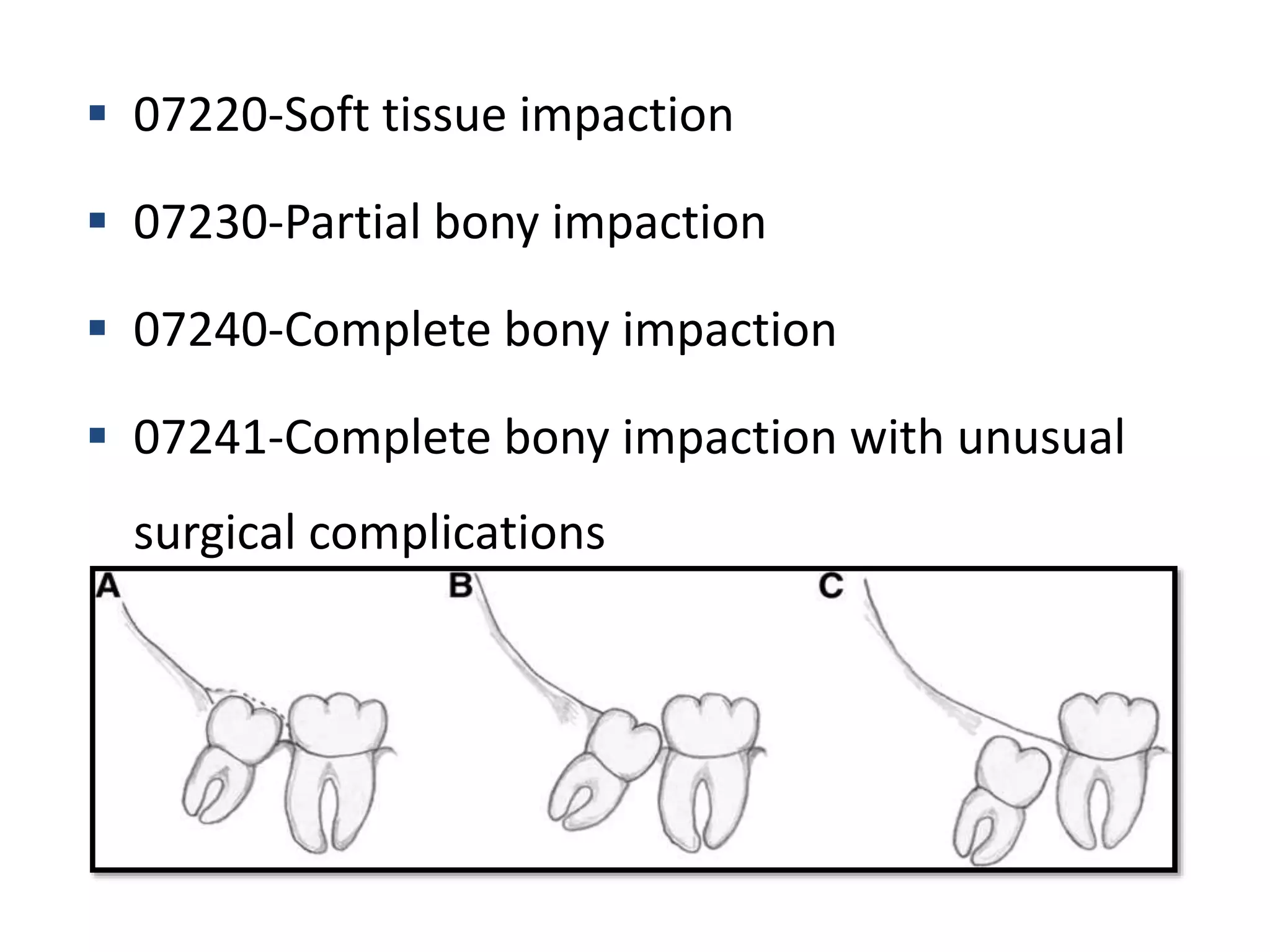
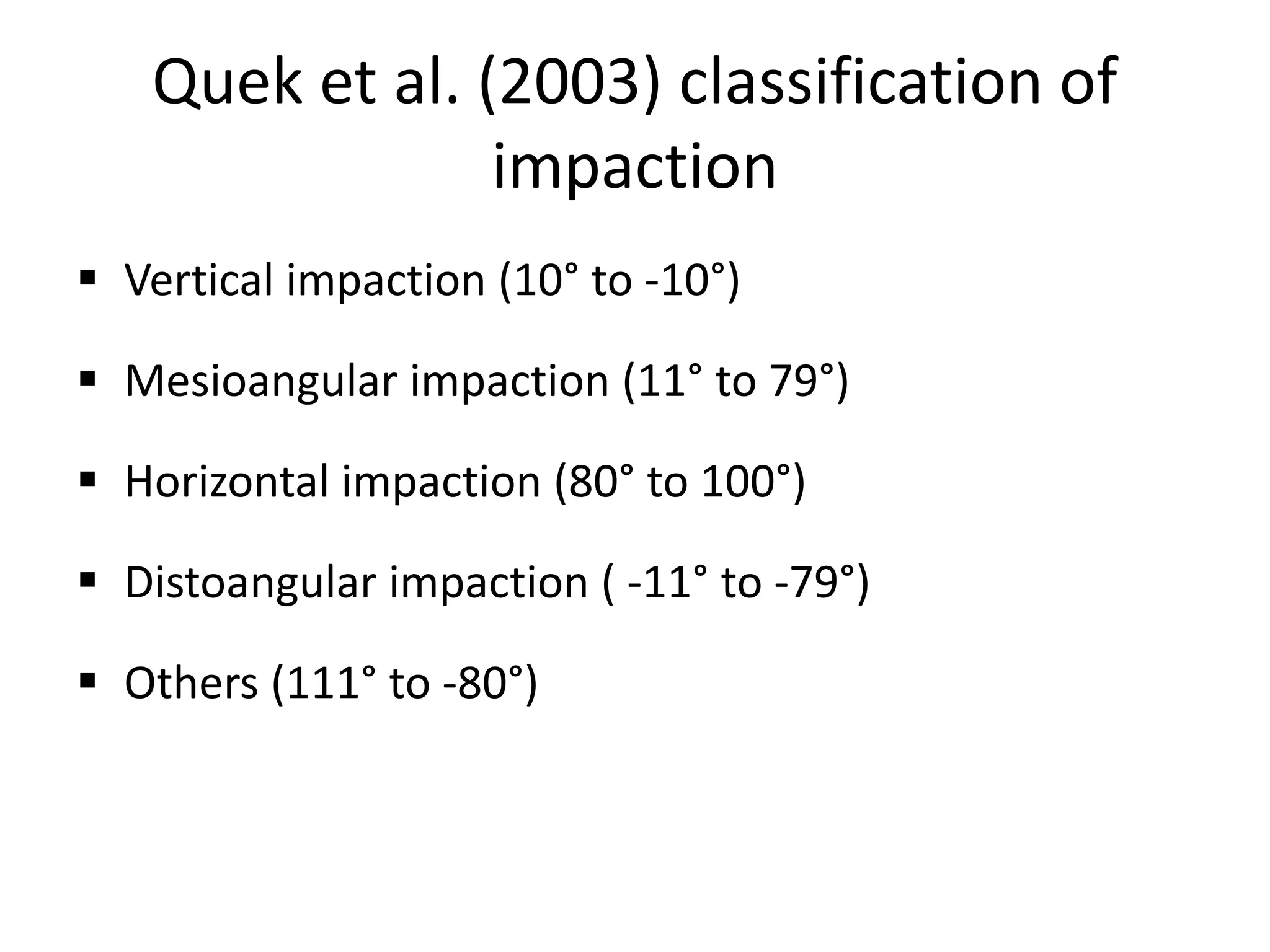
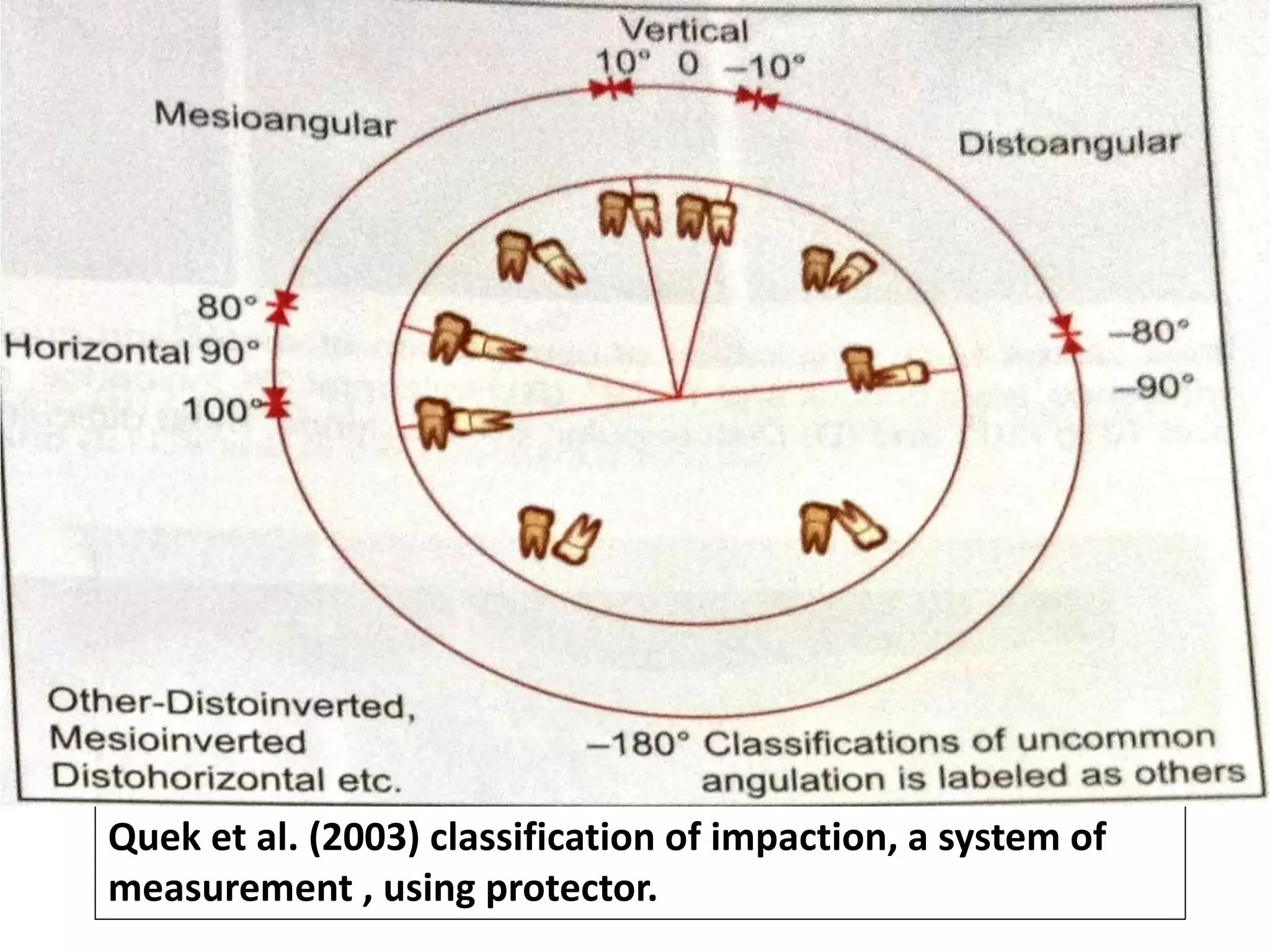
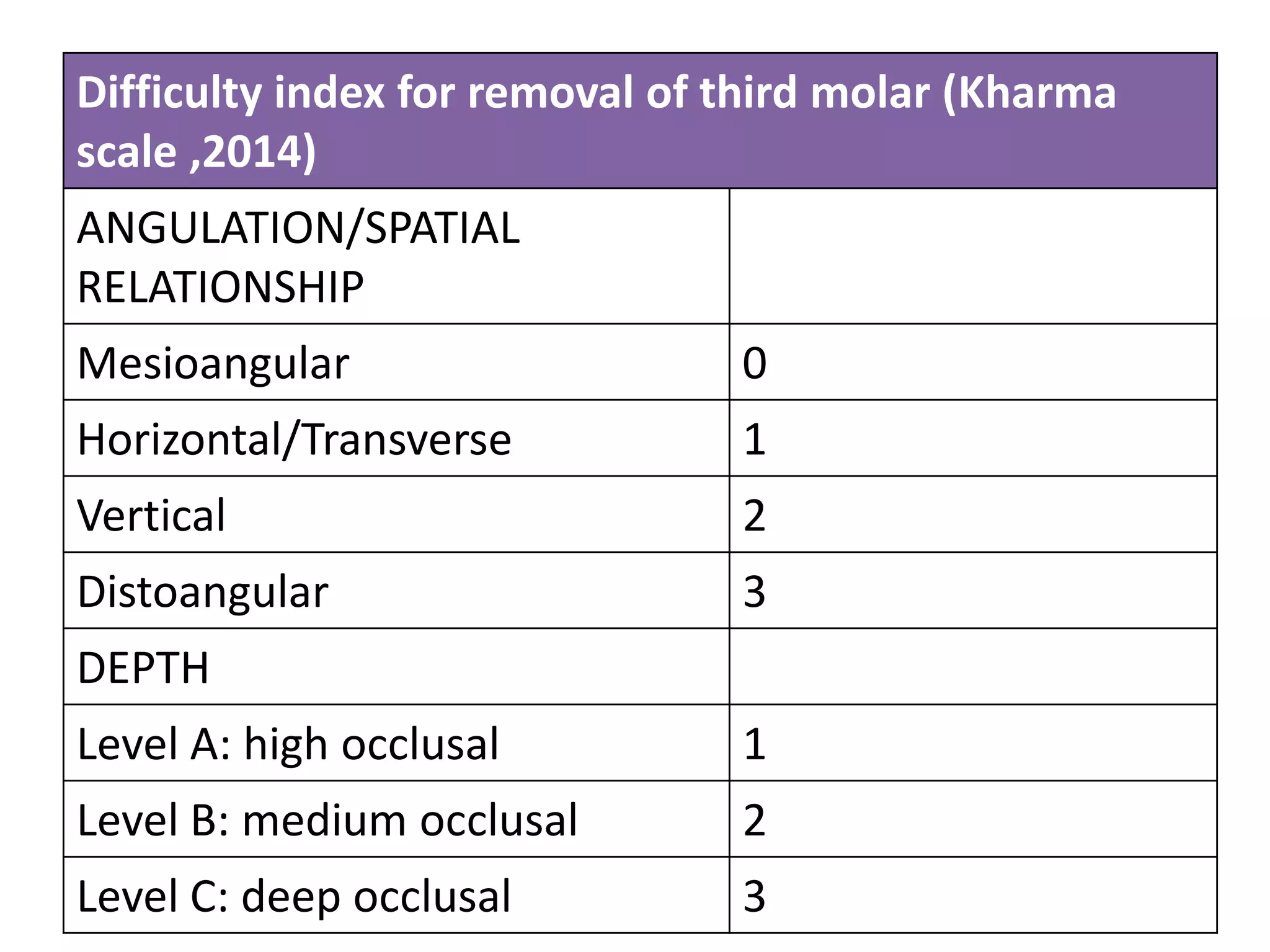
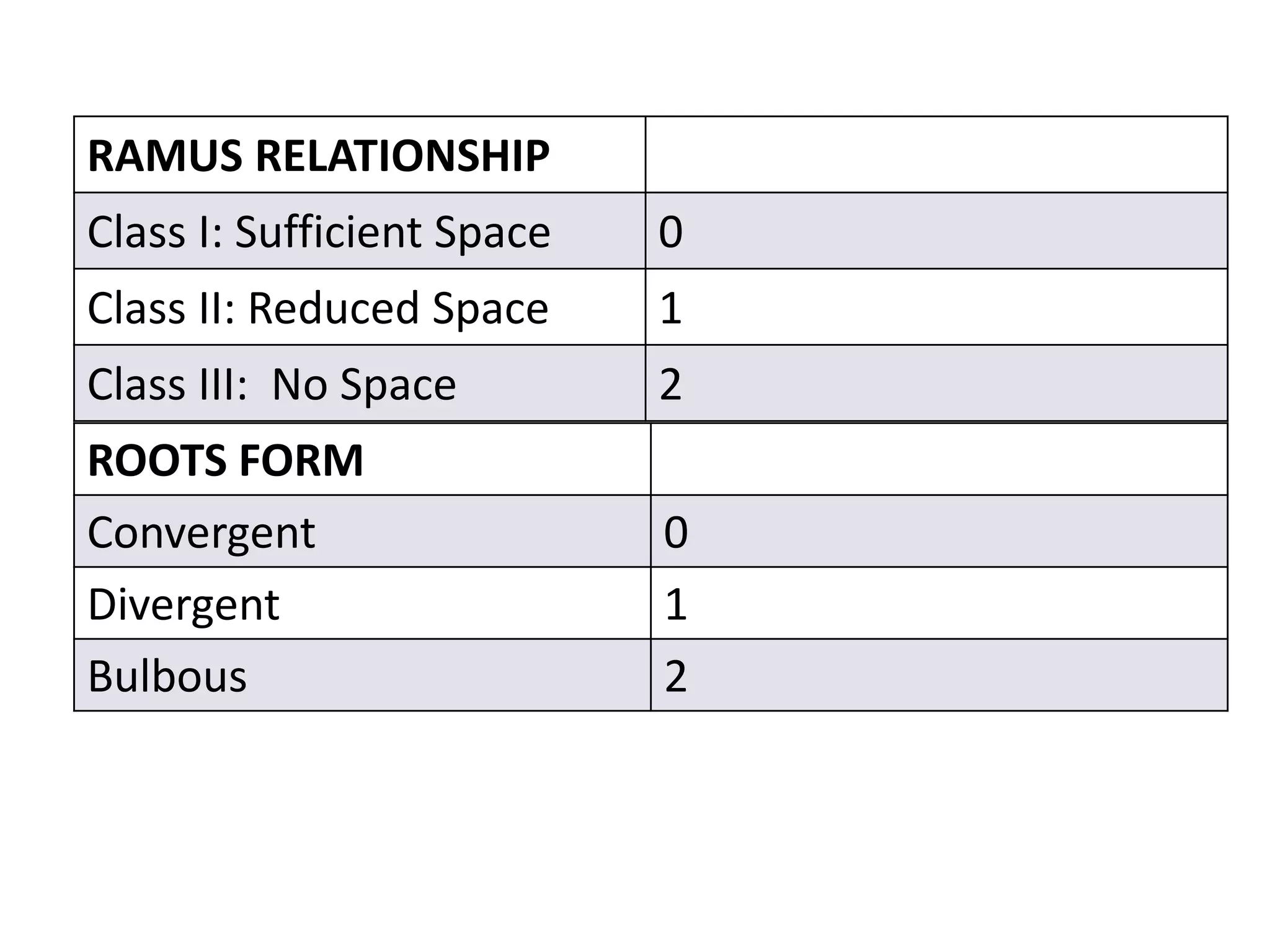
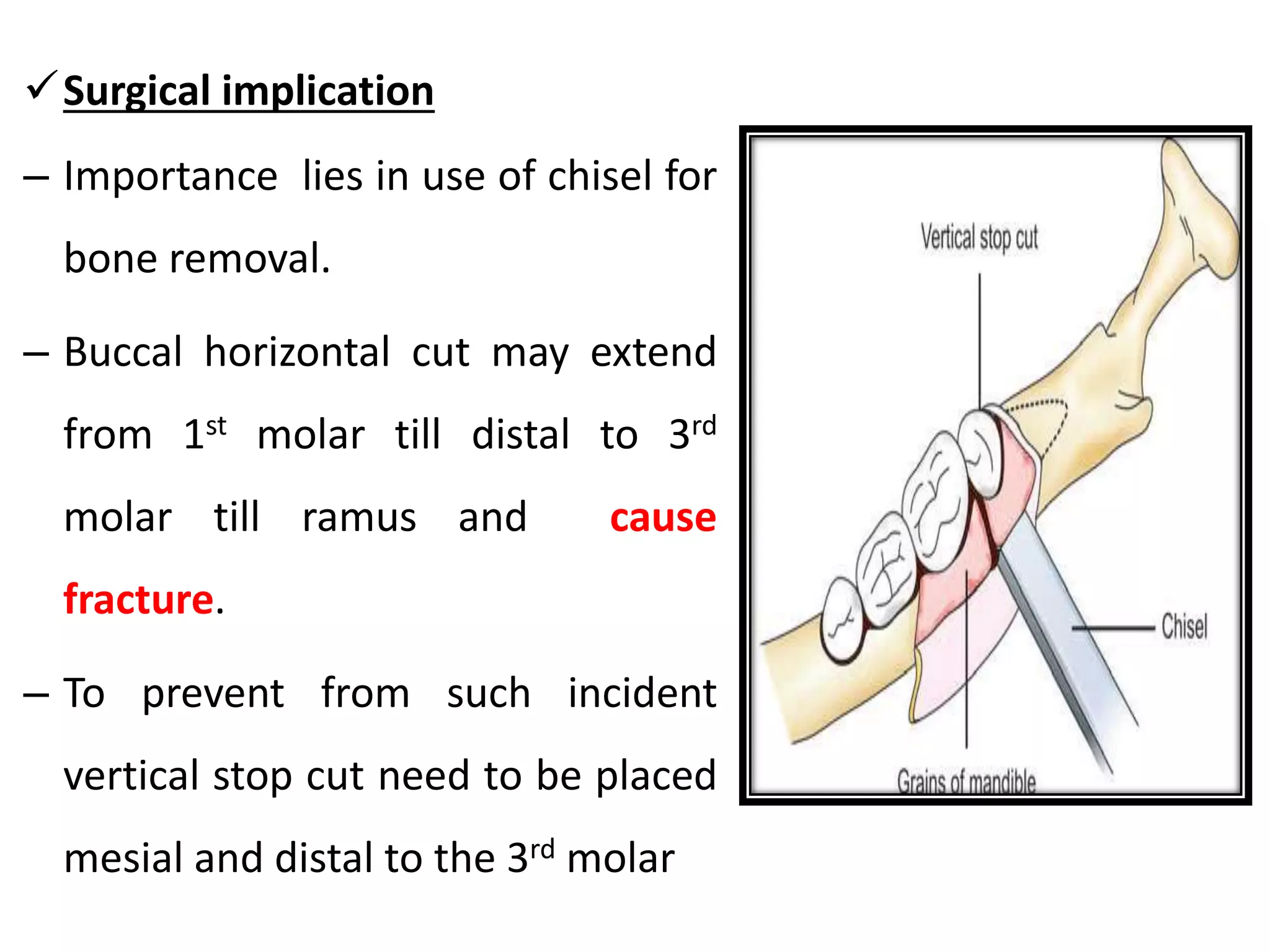
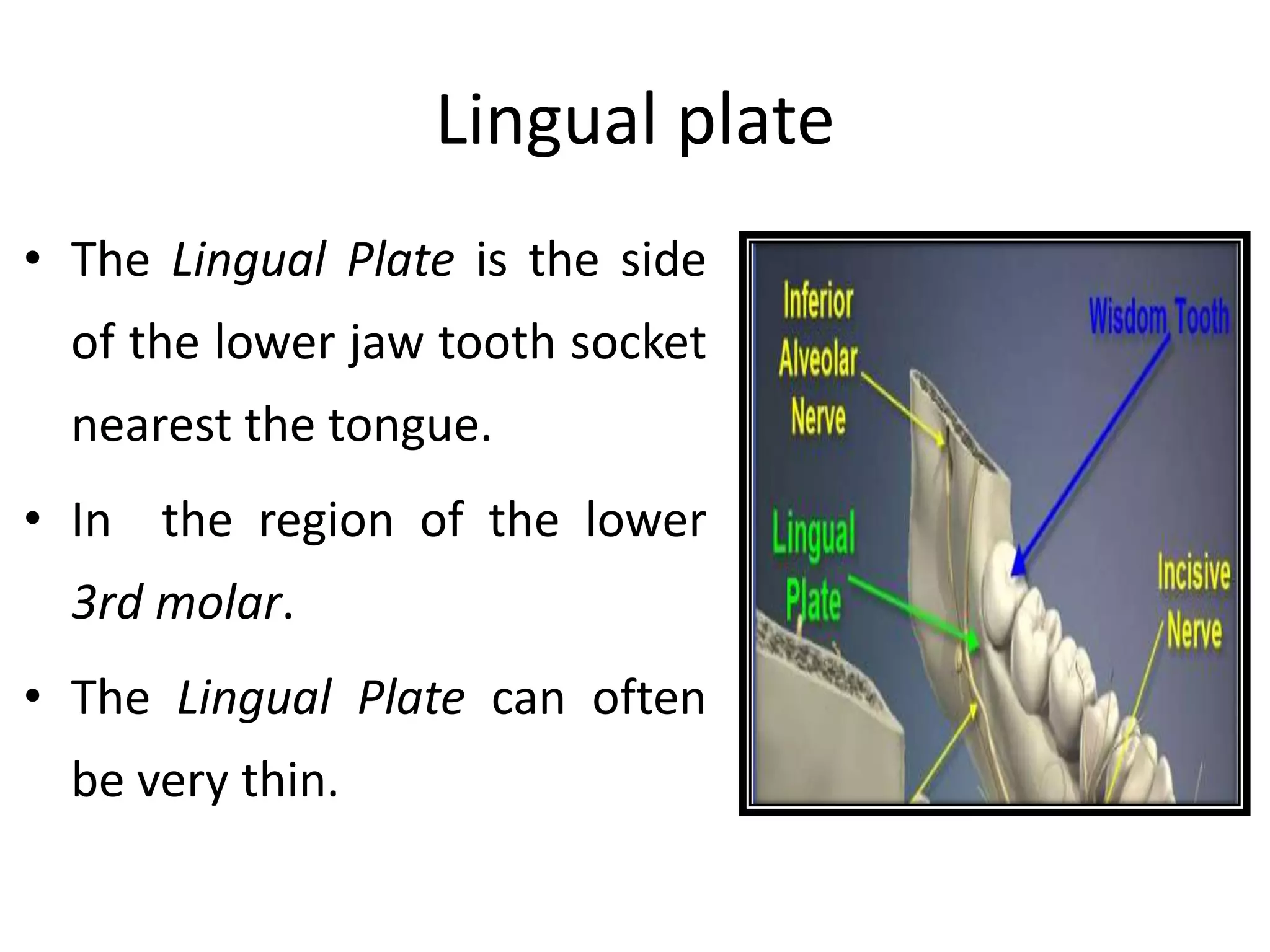
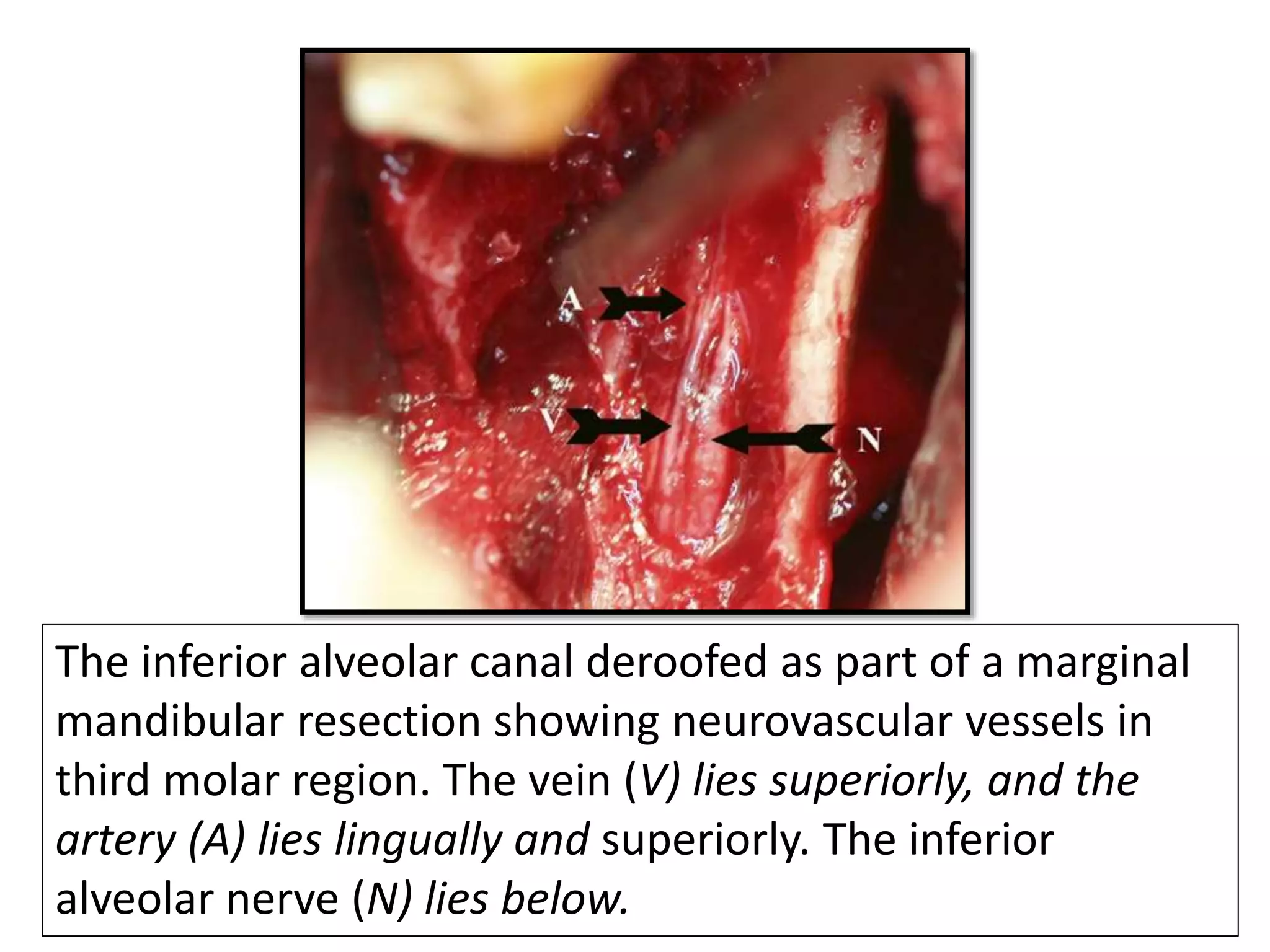
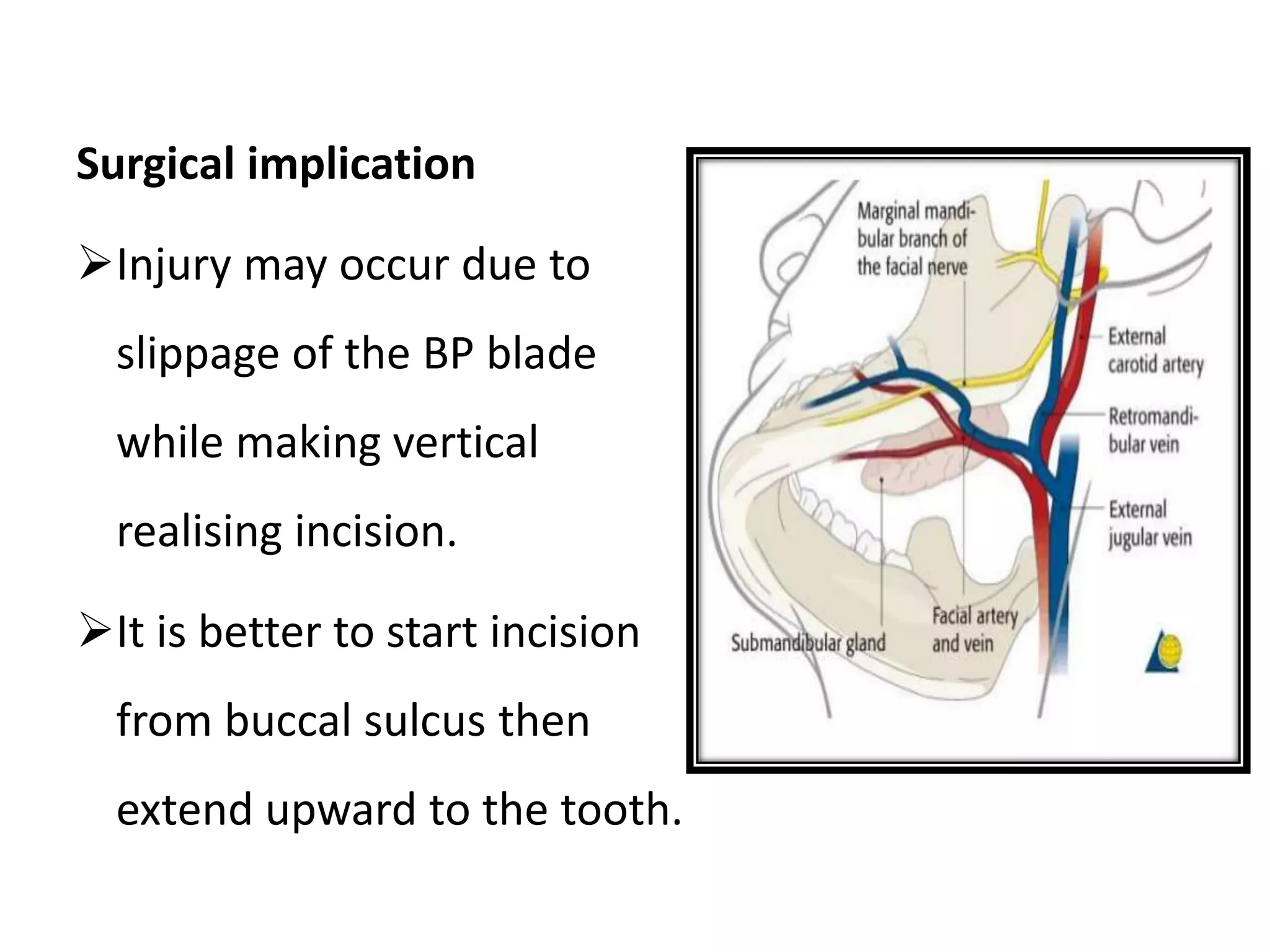
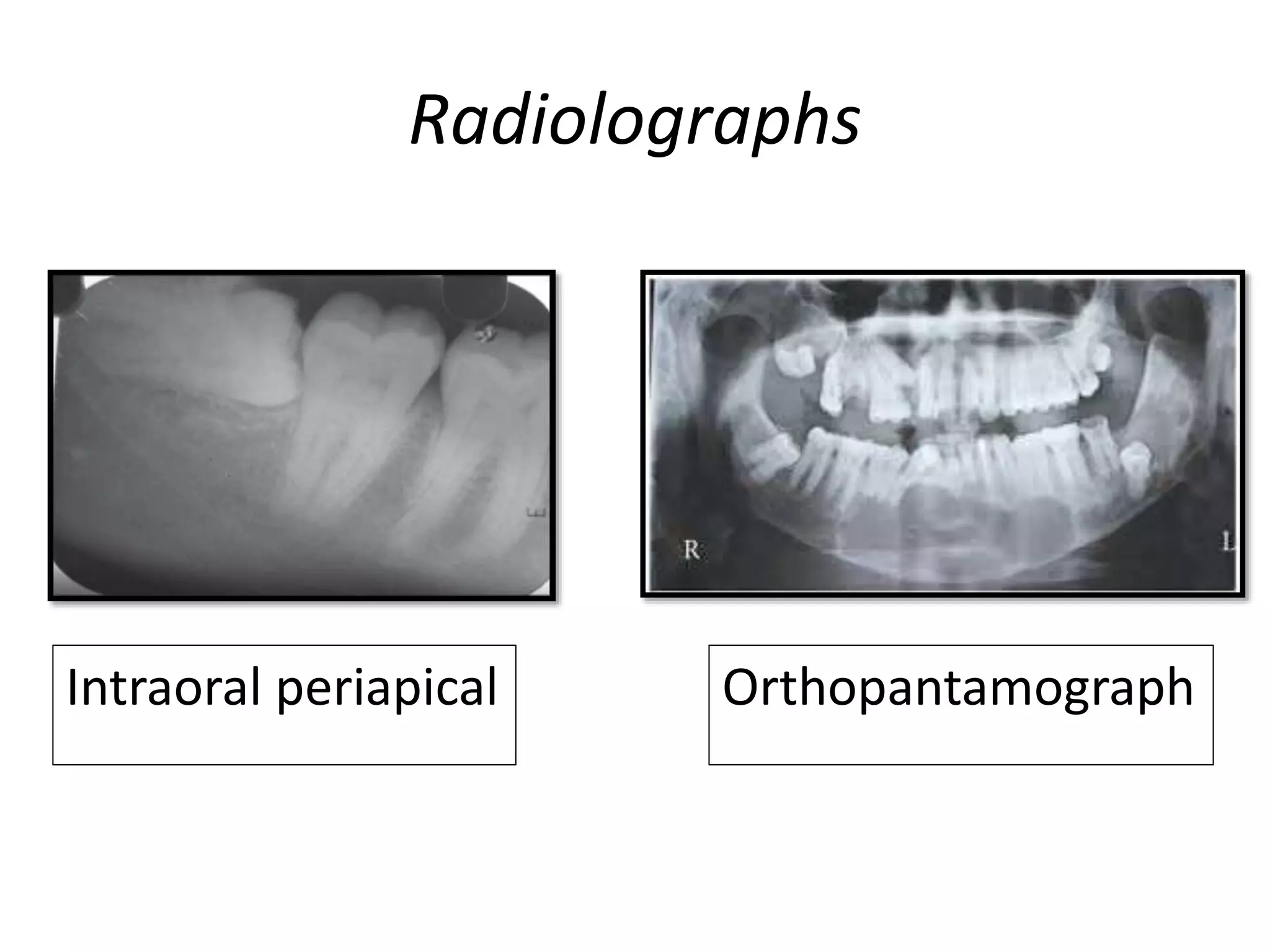
This document provides an overview of impacted third molars and their surgical removal. It discusses terminology, classifications, development, indications, contraindications and complications. Common classifications described include Winter's classification based on angulation and Pell & Gregory's classification analyzing anatomical relationships. Key points are that third molars are the last to erupt, between ages 18-25, and may become impacted due to insufficient jaw size or other impediments, leading to surgical removal which is one of the most common procedures in oral surgery. Careful planning is required due to potential complications.