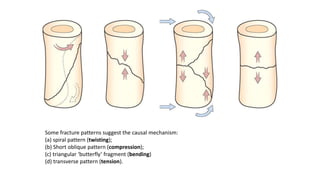
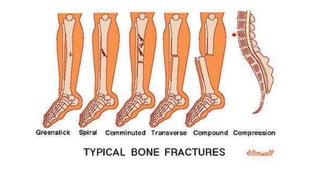
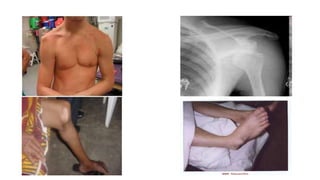
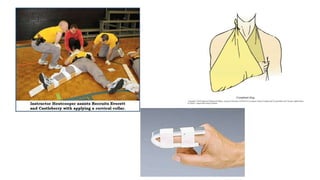
A fracture is a break in the bone caused by direct or indirect force. There are different types of fractures including complete, incomplete, transverse, oblique, and comminuted. Fractures can be displaced by forces of injury, gravity, muscles, or patient age. Symptoms include pain, swelling, deformity, and loss of movement. Treatment depends on the fracture and may include splinting, casting, traction, or surgery. A dislocation occurs when bones at a joint are no longer in proper contact, most commonly in the shoulder, elbow, thumb, or knee. Signs include deformity, pain, swelling, and loss of function. Treatment focuses on RICE (rest, ice, compression, elevation