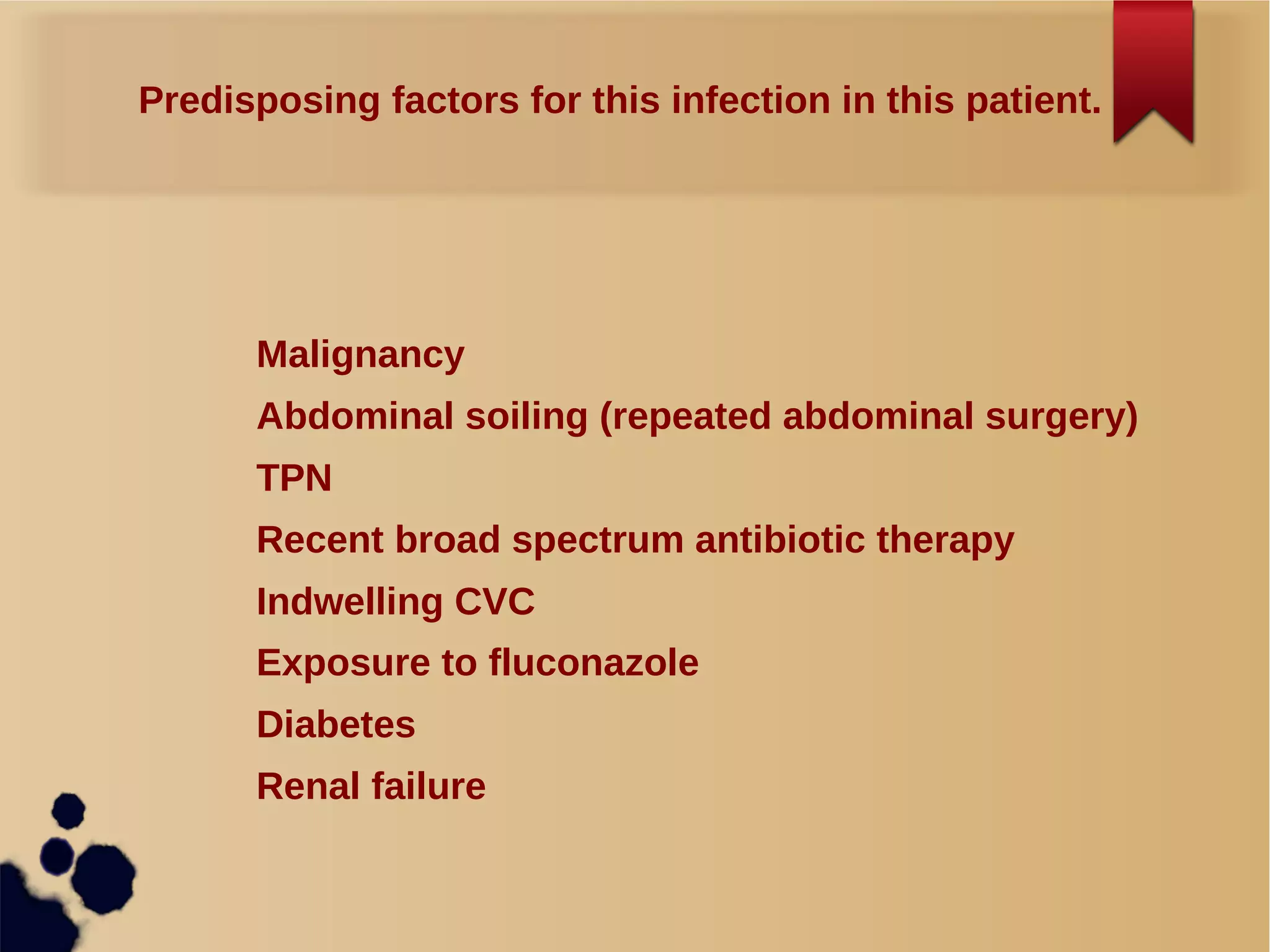
A 50-year-old man with perforated colon cancer and sepsis underwent surgery but remained febrile and leukocytic despite antibiotics. Blood cultures grew Candida glabrata, which may be resistant to fluconazole. The patient is at risk of fungal infection due to recent surgery, antibiotics, TPN, and exposure to fluconazole. Voriconazole, amphotericin B or caspofungin would be started while awaiting sensitivities as C. glabrata may not respond to fluconazole. An echocardiogram is recommended to check for vegetations which could influence antifungal treatment duration and prognosis.