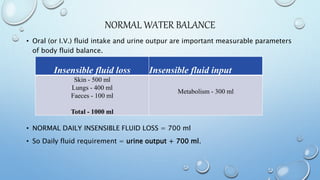
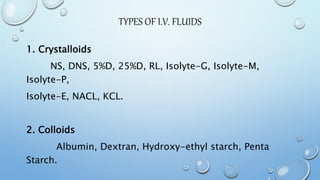
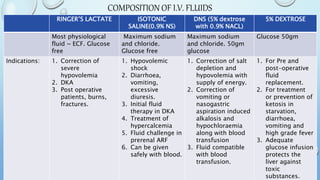
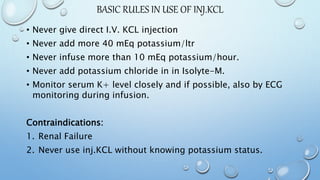
This document discusses fluid therapy and intravenous fluid administration. It begins by explaining normal water balance and insensible fluid loss. The basic principles of IV fluid therapy are then outlined, including advantages like accurate administration and rapid response, as well as indications like dehydration and shock. Contraindications and complications are also reviewed. The document then describes the types of IV fluids, including crystalloids like saline and lactated Ringer's, as well as colloids like albumin. Special fluids like sodium bicarbonate and potassium chloride are also covered. Guidelines for fluid administration and monitoring are provided.