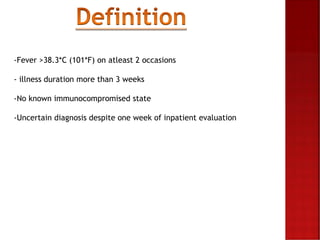
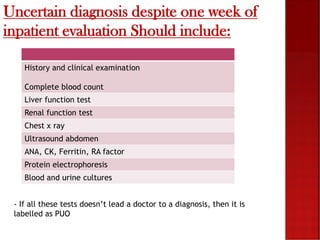
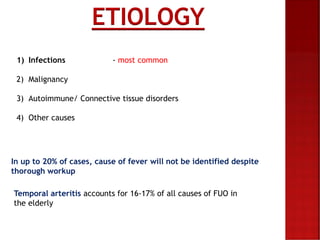
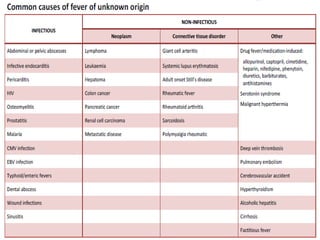
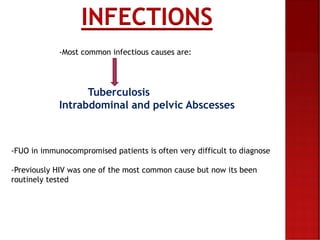
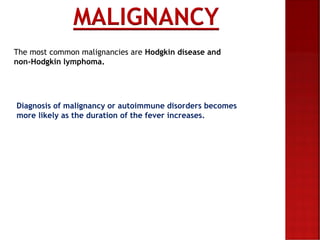
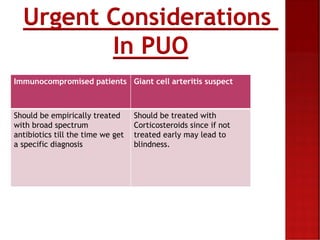
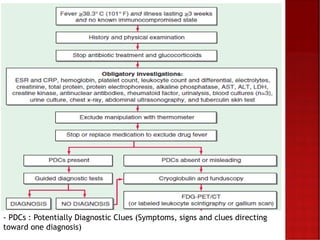
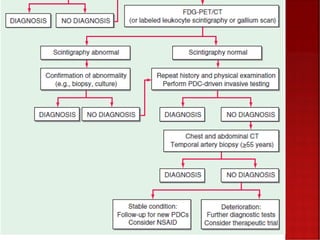
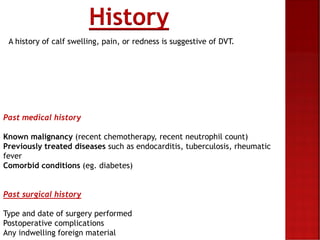
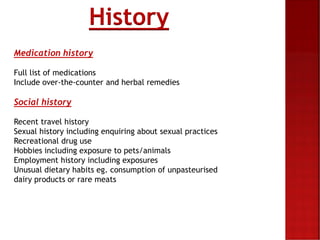
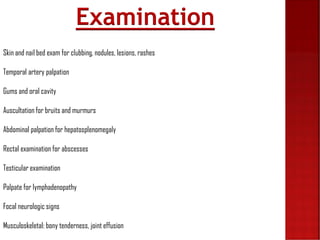
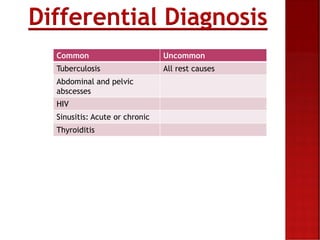
The document discusses pyrexia of unknown origin (PUO), defined as fever over 38.3°C on at least two occasions with an illness duration exceeding three weeks, and outlines the diagnostic workup including various tests and examinations. Common causes include infections, malignancies, and autoimmune disorders, with specific attention to the diagnostic approach in immunocompromised patients. Urgent considerations for conditions like temporal arteritis and giant cell arteritis are highlighted, emphasizing the need for empirical antibiotic treatment and corticosteroids to prevent serious complications.