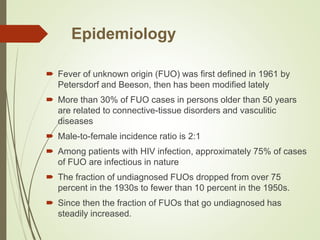
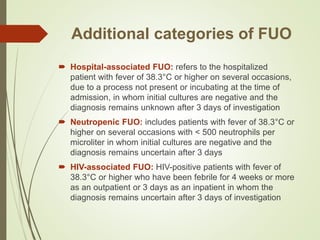
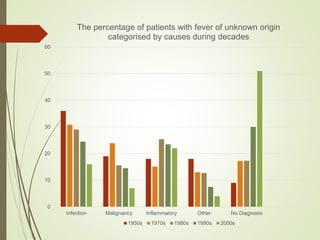
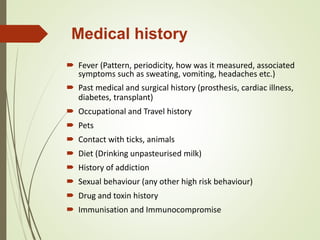
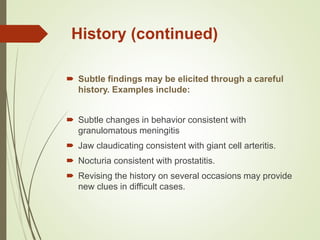
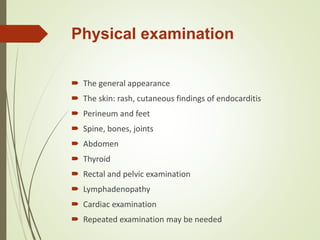
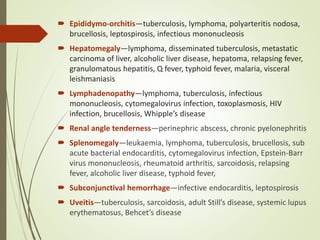
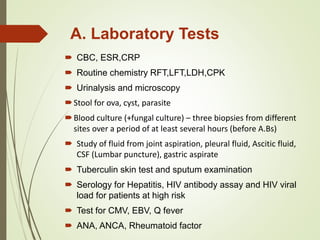
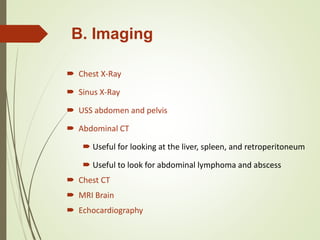
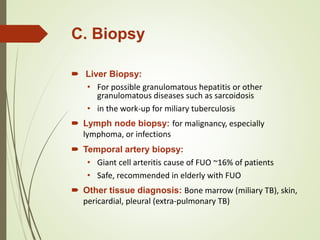
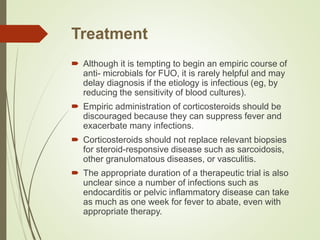
This document provides information on fever of unknown origin (FUO). It defines FUO as a fever over 38.3°C for at least 3 weeks without a confirmed diagnosis after tests and visits. Common causes include infections, cancers, and autoimmune disorders. The evaluation involves medical history, exam, lab tests, imaging and biopsies to identify infectious, inflammatory or malignant sources. Treatment focuses on the underlying cause rather than empiric antibiotics or steroids. Some cases remain undiagnosed, but most adult patients have a good prognosis in these situations.