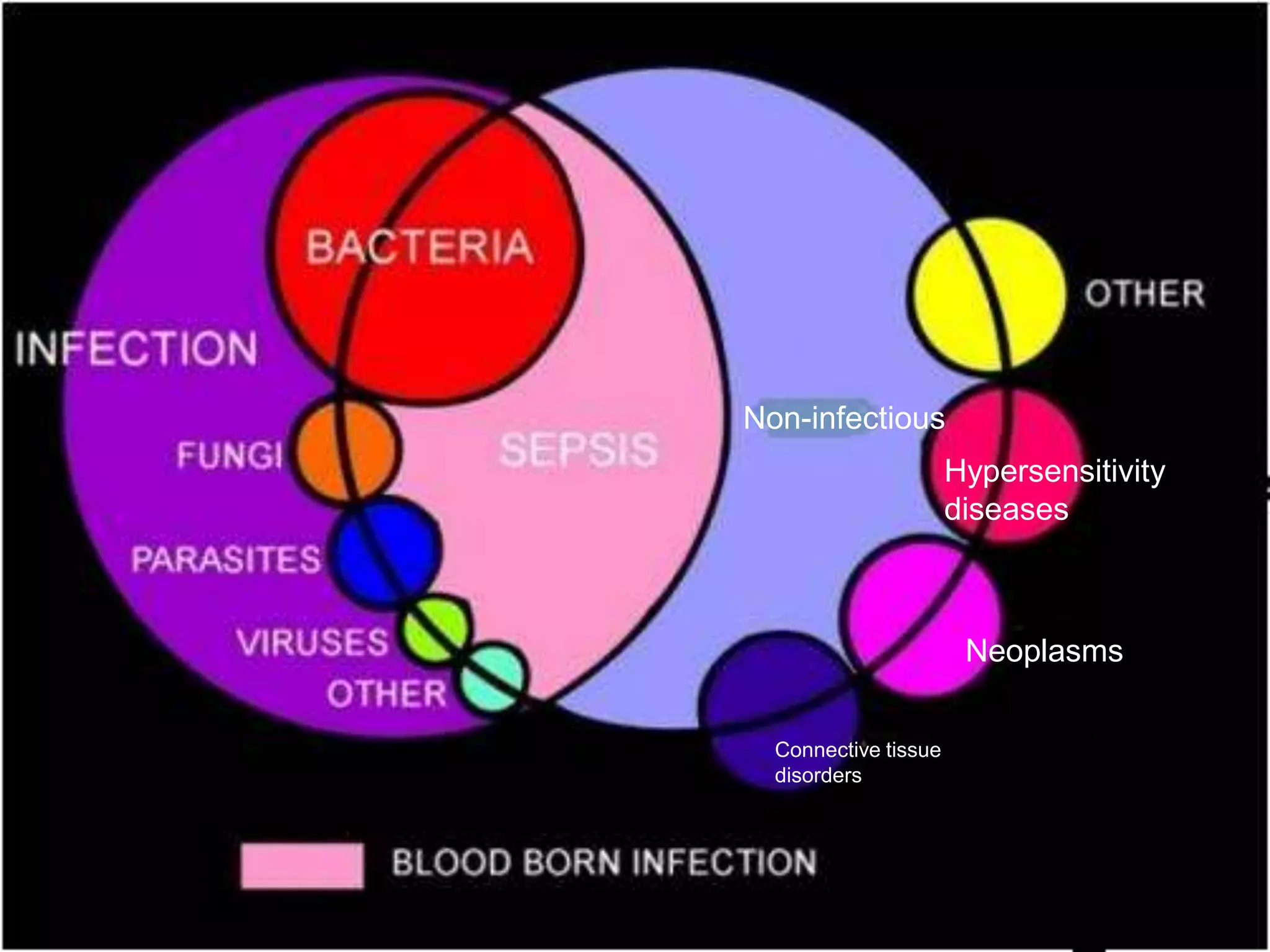
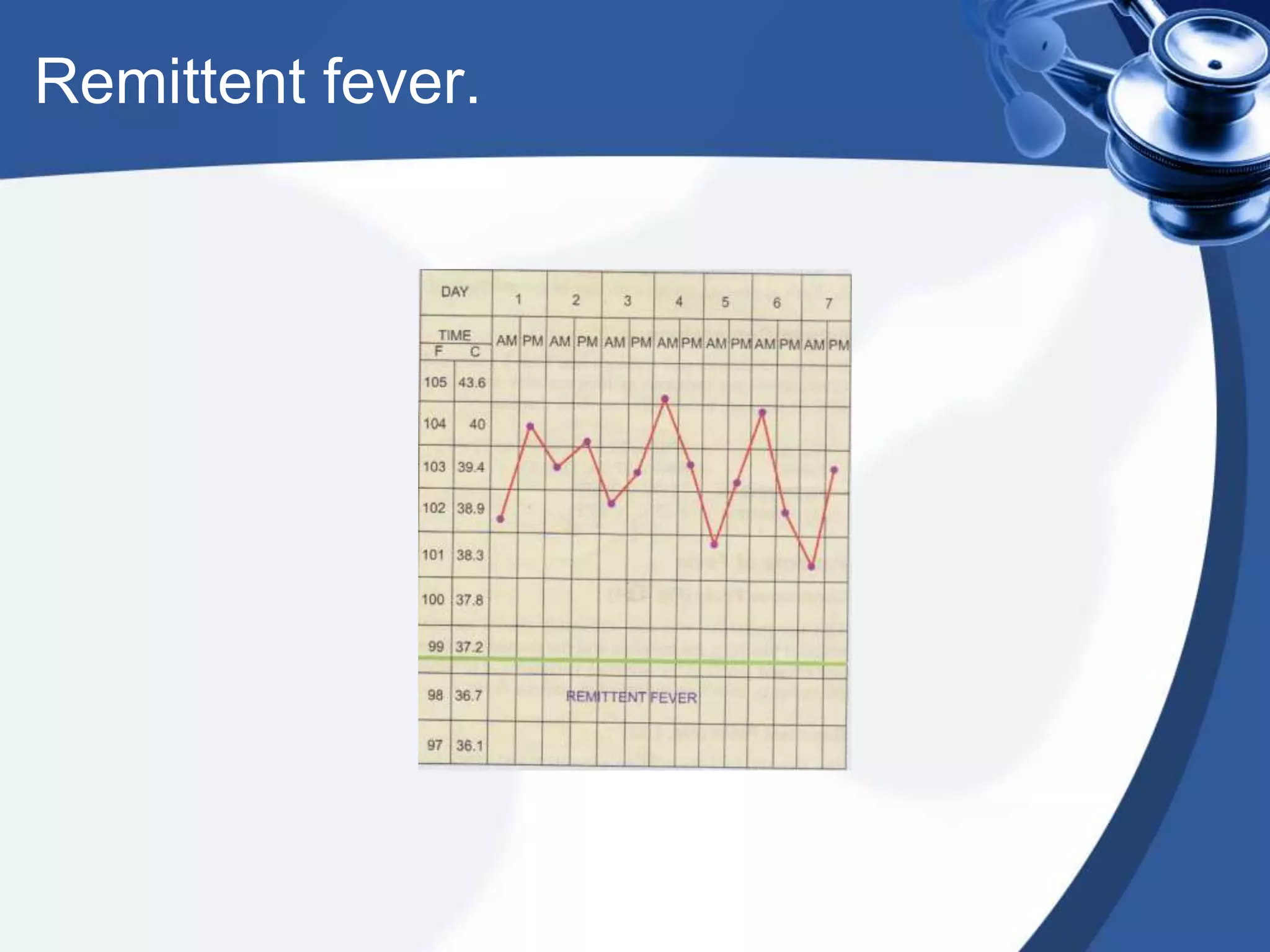
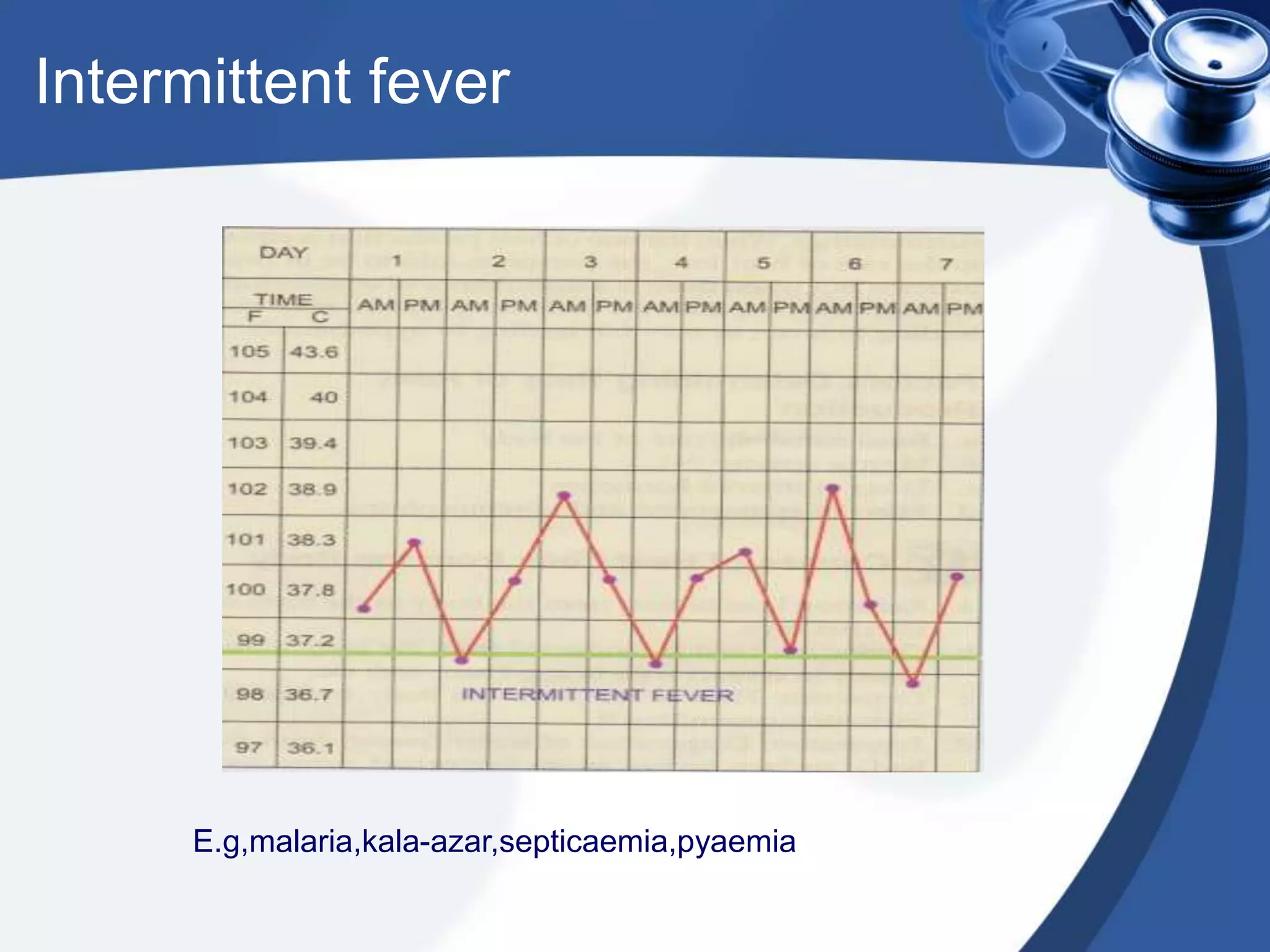
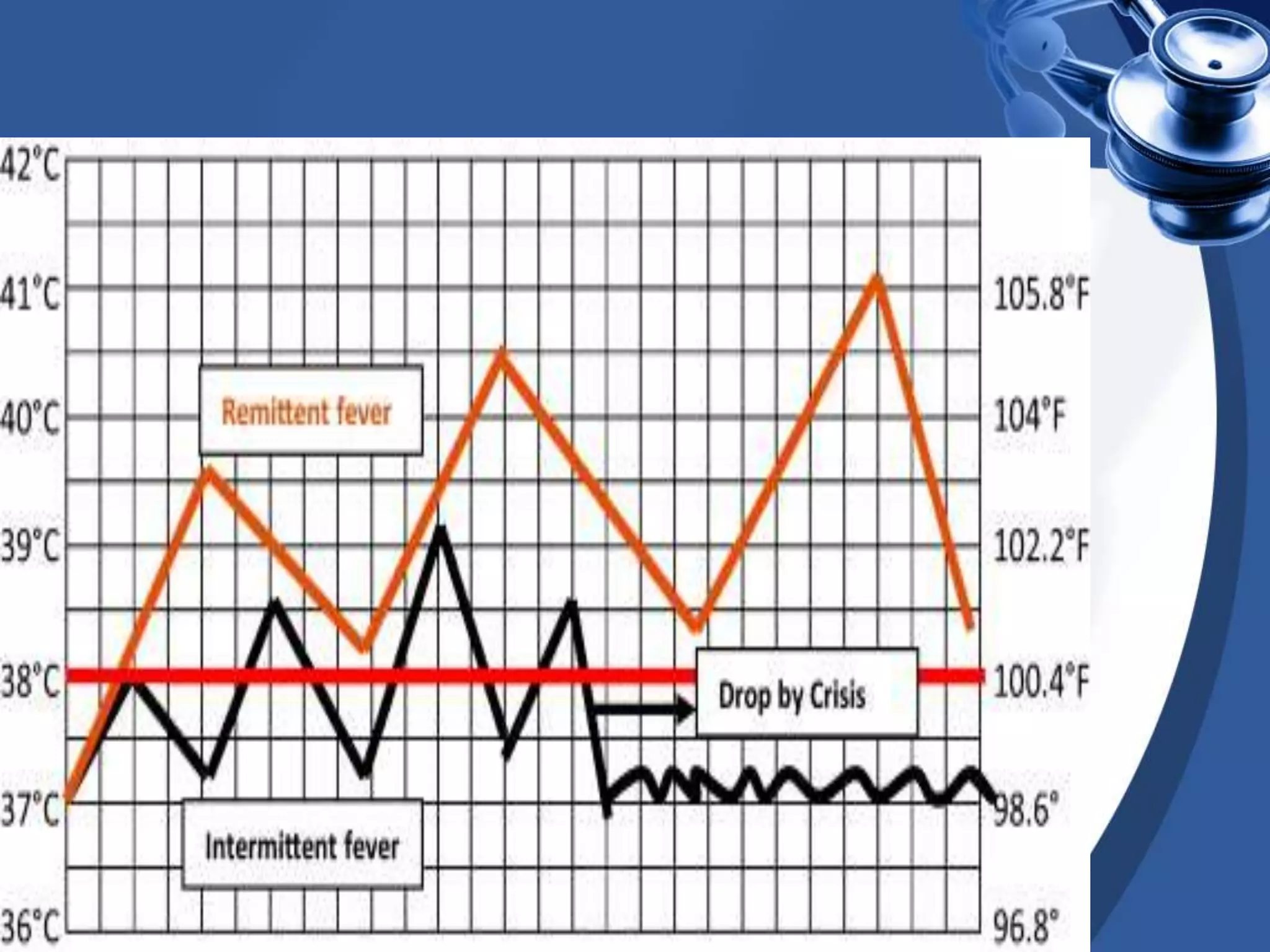
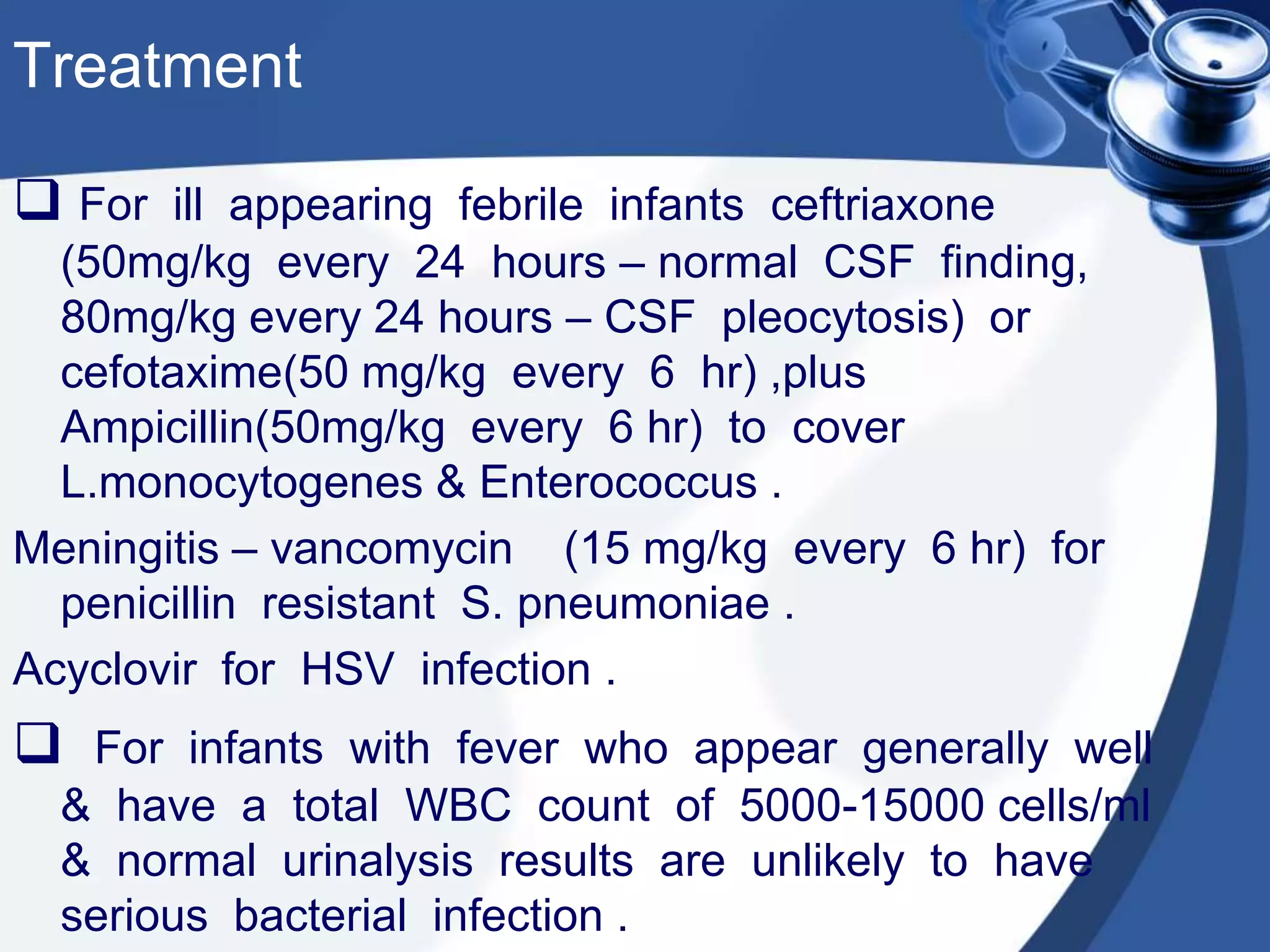
This document provides a tutorial on fever of unknown origin. It discusses normal body temperature regulation and the definition of fever. It describes the pathogenesis and causes of fever, which can be infectious such as bacterial, viral, parasitic, or non-infectious such as neoplasms, connective tissue disorders, and hypersensitivity diseases. It outlines various patterns of fever and provides classifications. It focuses on fever without a focus, distinguishing fever without localizing signs from fever of unknown origin. It provides guidelines for evaluating and managing febrile infants of different ages from neonates to 3 months.