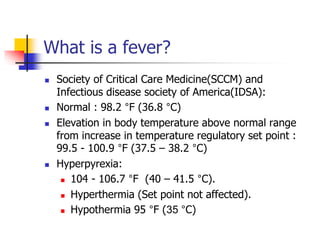
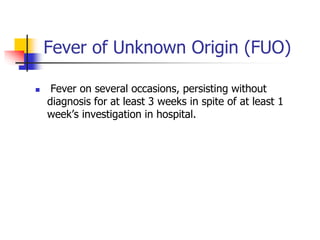
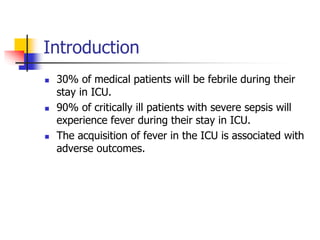
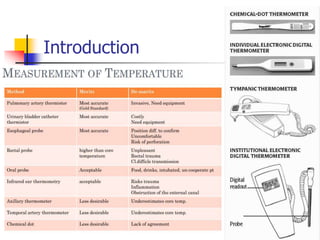
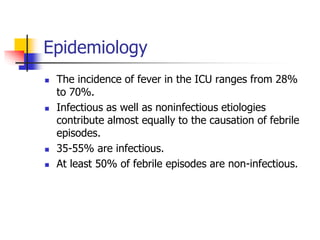
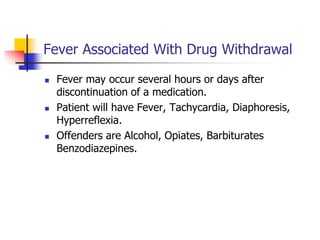
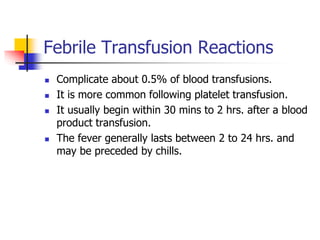
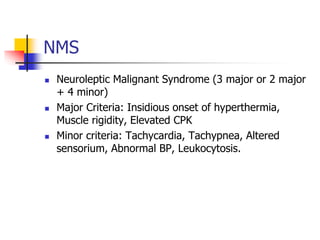
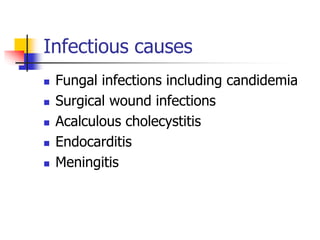
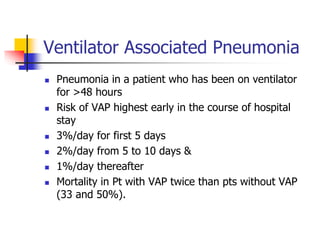
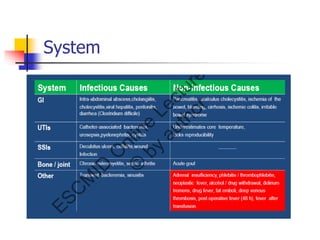
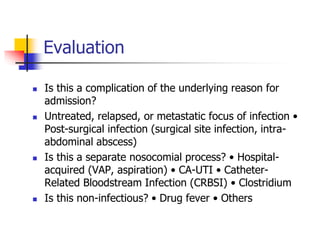
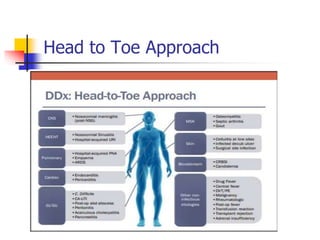
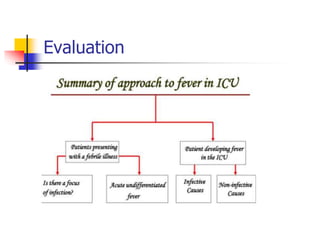
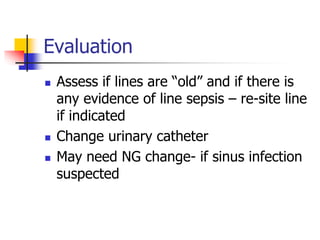
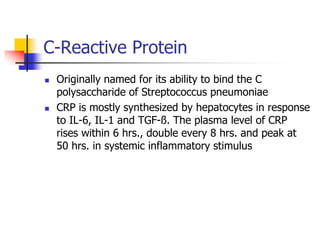
Fever is a common problem in the ICU, occurring in 30-70% of patients. It can be caused by infections, non-infectious factors, or a combination. A thorough evaluation including blood tests, imaging, and cultures is important to determine the cause. Common infectious causes include ventilator-associated pneumonia, catheter-related bloodstream infections, and urinary tract infections. Non-infectious causes include drug reactions, transfusions, and environmental factors. Prompt treatment of the underlying cause is key to avoiding adverse outcomes in critically ill ICU patients experiencing fever.