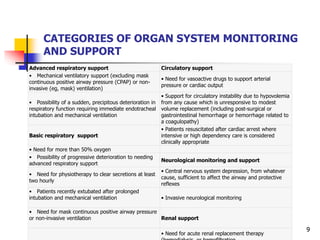
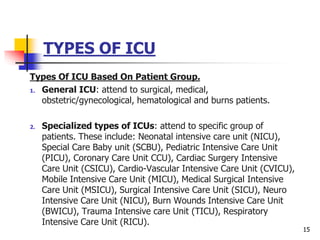
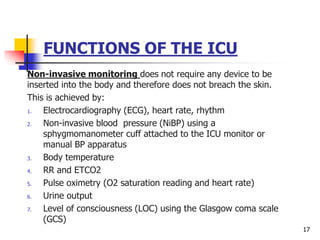
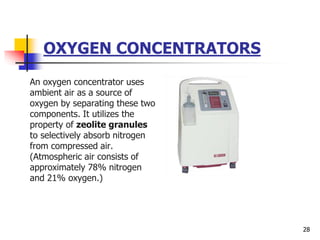
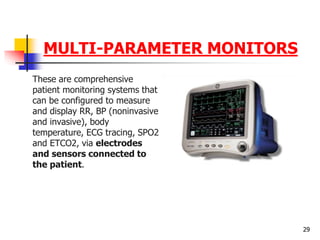
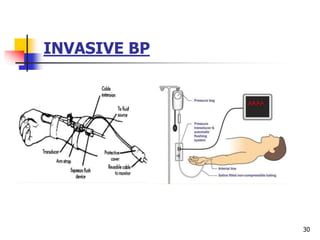
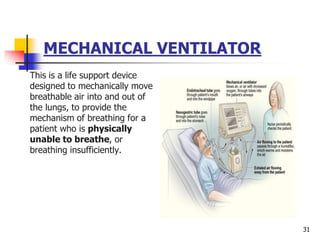
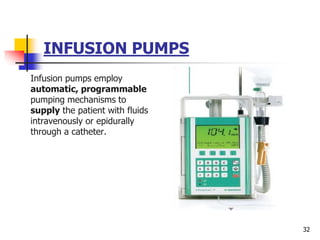
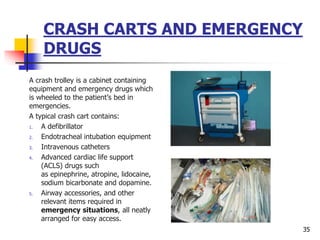
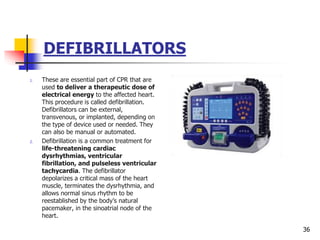
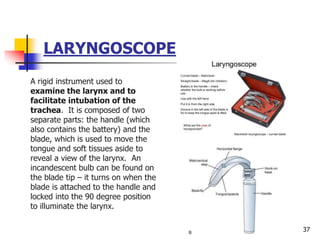
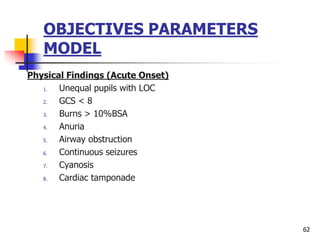
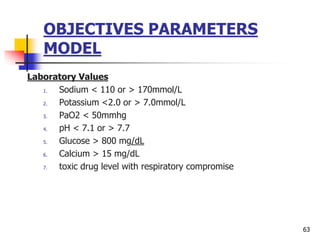
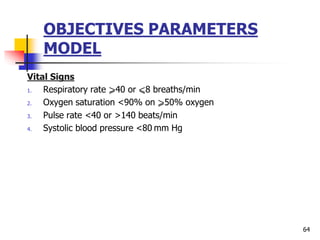
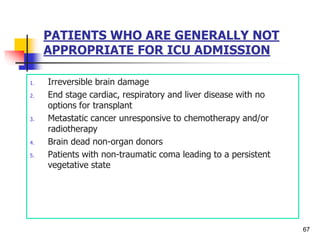
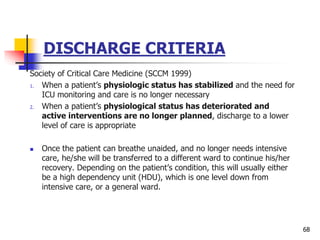
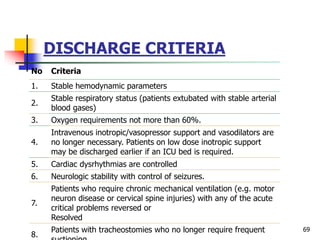
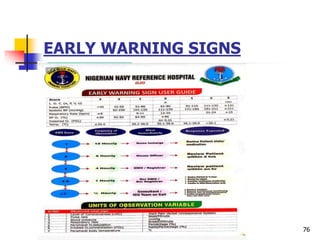
This document provides an overview of indications for admission to an intensive care unit (ICU). It discusses the types of ICUs, including open and closed units, and specialty units organized by patient type. The functions of the ICU are described, including invasive and non-invasive monitoring, hemodynamic support, ventilation, nutrition, and treatment of the underlying illness. Admission criteria include those needing advanced respiratory, circulatory, neurological, or renal support. Equipment used in ICUs is also reviewed.