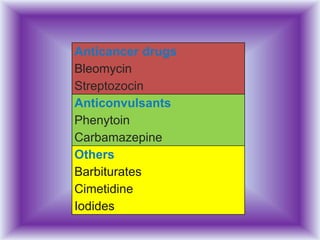
Fever is defined as a temperature of 38°C or higher in infants and 38.3°C or higher in adults. Immunocompromised patients may not develop a high enough fever. Low grade fevers in these patients should be addressed cautiously. Rectal temperatures are most accurate for measuring core body temperature. A fever is caused by elevation of the hypothalamic temperature set point while hyperthermia is elevated temperature without a changed set point. Antipyretics like acetaminophen and ibuprofen are used to reduce fever for patient comfort but fever itself is not generally harmful. Infection is the most common cause of fever but other potential causes include medications, malignancies, and inflammatory conditions.




















![Causes of fever
•Central nervous system lesions
(e.g., stroke, intracranial bleed, or trauma)
•Illicit drug use
(cocaine, ecstasy [MDMA], or methamphetamines)
•Withdrawal syndromes
•(delirium tremens or benzodiazepine withdrawal)
•Factitious fever
•Medications](https://image.slidesharecdn.com/feverinicu-150326105914-conversion-gate01/85/Fever-in-icu-22-320.jpg)