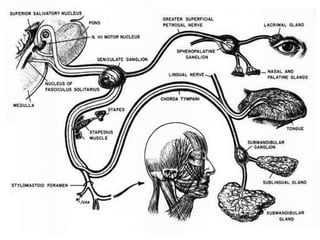
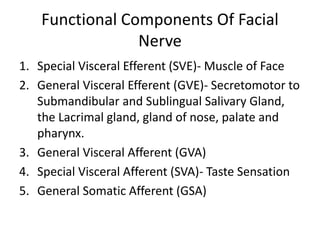
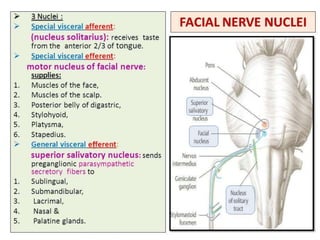
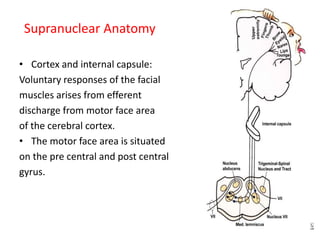
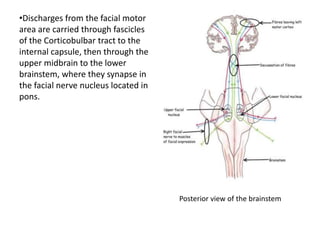
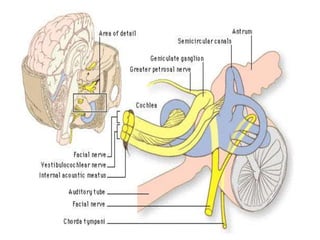
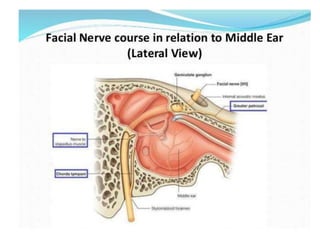
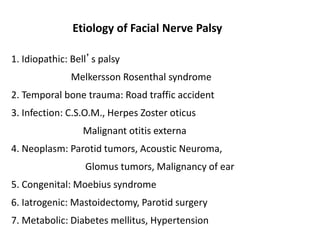
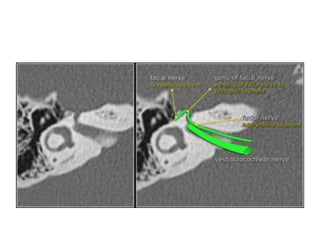
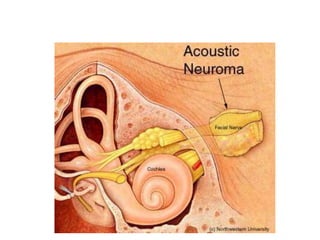
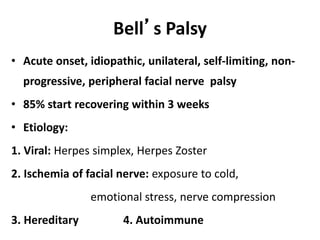
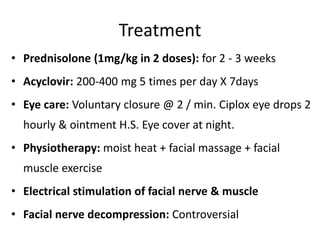
The facial nerve arises from nuclei in the brainstem and travels through the temporal bone, where it is vulnerable to injury. It innervates the muscles of facial expression and provides motor, sensory, and autonomic functions. Bell's palsy is an acute onset idiopathic peripheral facial nerve palsy that typically recovers within 3 weeks with treatment such as corticosteroids and antivirals.