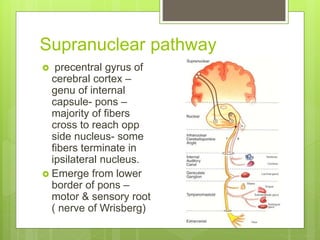
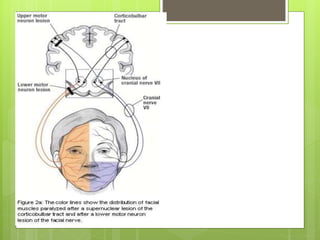
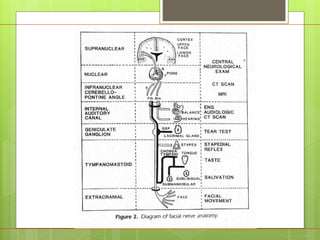
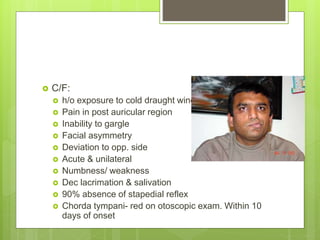
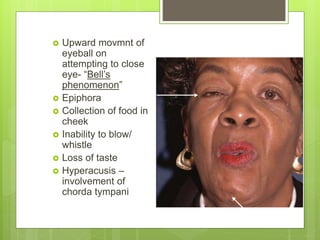
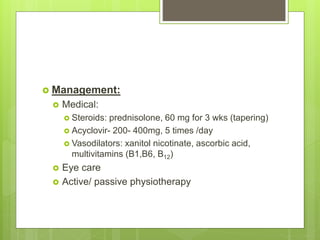
This document provides an overview of the facial nerve (cranial nerve VII), including its anatomy, branches, course, variations, testing, and causes of paralysis. Some key points:
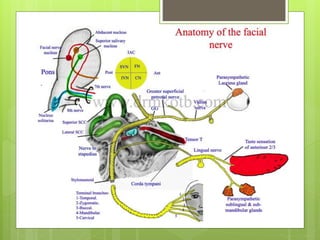
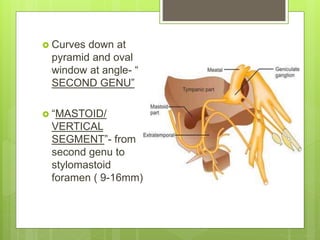
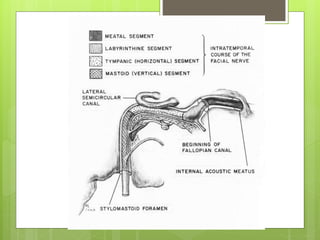
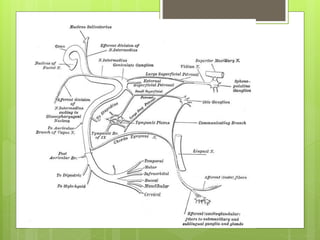
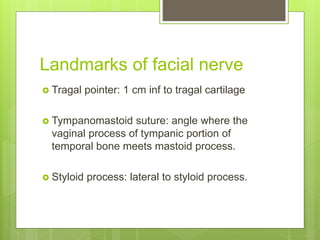
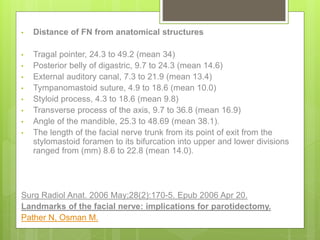
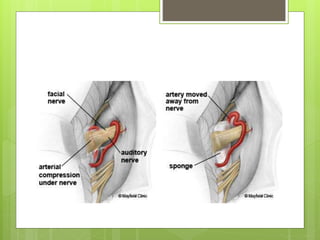
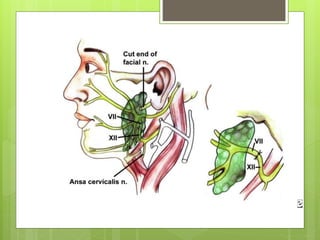
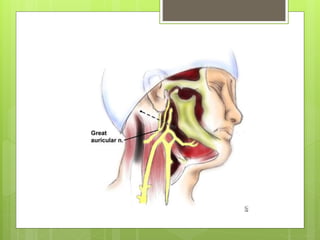
- The facial nerve has intracranial, intratemporal, and extratemporal segments as it passes through the skull and exits at the stylomastoid foramen.
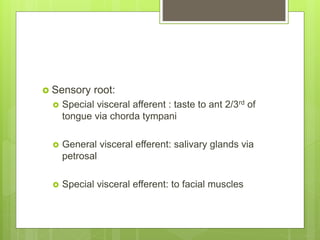
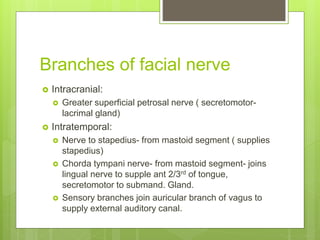
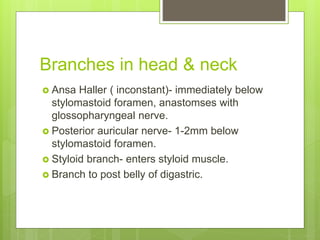
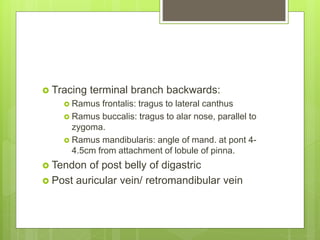
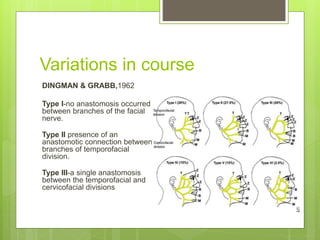
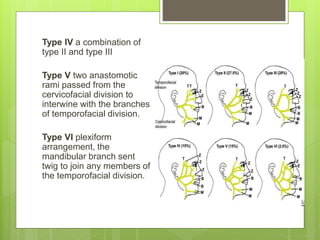
- It gives off numerous branches including the chorda tympani, nerve to stapedius, and branches in the parotid plexus.
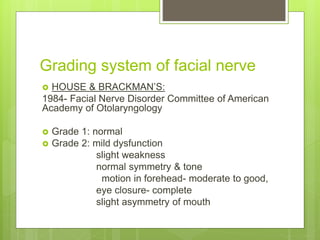
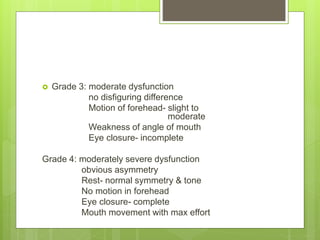
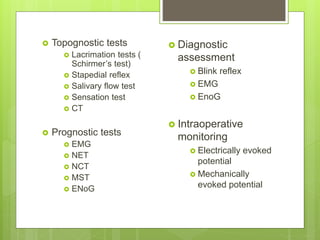
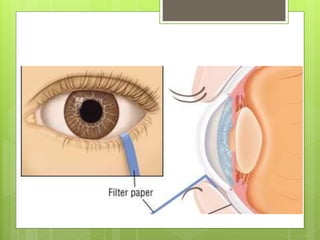
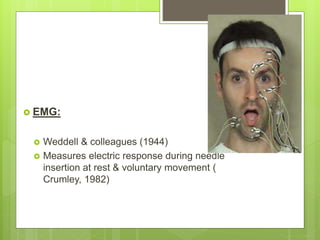
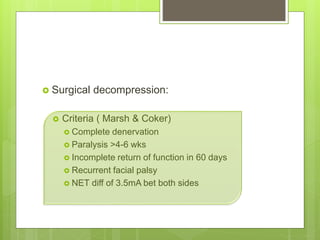
- Testing includes topognostic tests like lacrimation and salivary flow, as well as electrodiagnostic tools like EMG, NCT, and MST to evaluate