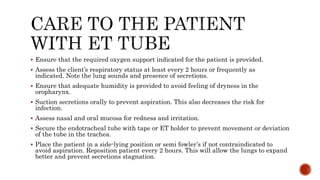
Endotracheal intubation involves the placement of a flexible tube through the mouth into the trachea to assist patients who cannot breathe independently. The procedure is often used in emergencies and requires careful management to prevent complications such as tube obstruction, dislodgment, and injury. Continuous monitoring and supportive care are essential, including proper positioning, suctioning, and ensuring adequate oxygenation and nutrition.