This document discusses epistaxis (nosebleeds), including:
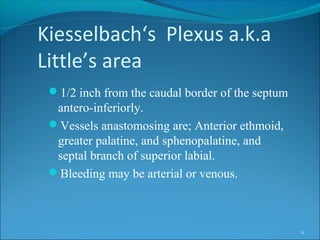
- The nasal vasculature and common bleeding sites like Kiesselbach's plexus make the nose prone to bleeding.
- Common causes of epistaxis include local irritation, medications, trauma, and underlying medical conditions.
- Initial treatment involves locating the bleeding site, applying pressure, and nasal packing. More severe cases may require cauterization, surgery, or angiographic embolization to stop the bleeding.