This document provides information on epistaxis (nosebleed) including:
- The anatomy of the nasal blood supply from both internal and external carotid arteries. The majority of anterior nosebleeds occur from Kiesselbach's plexus.
- Types of epistaxis including anterior (85-90% of cases) and posterior (10-15% involving those over 50).
- Causes can be local like trauma or tumors, or systemic like infections, blood disorders, or vascular problems.
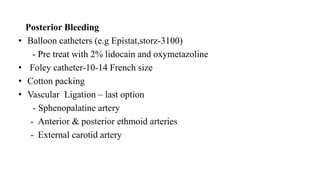
- Treatment depends on location but may include cauterization, nasal packing, balloon catheters, or ligation of arteries in severe cases. Hospitalization is needed for posterior bleeds or those