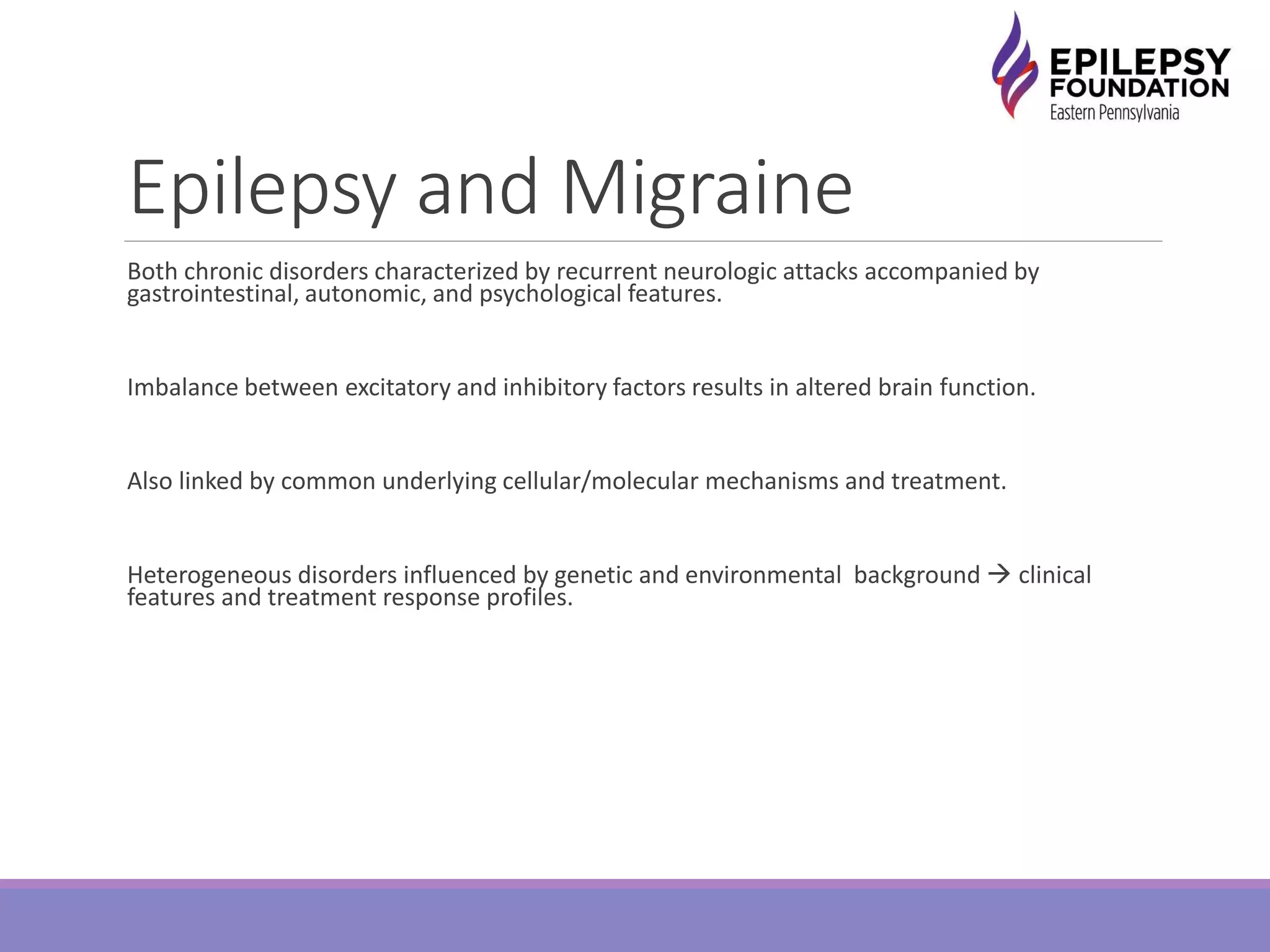
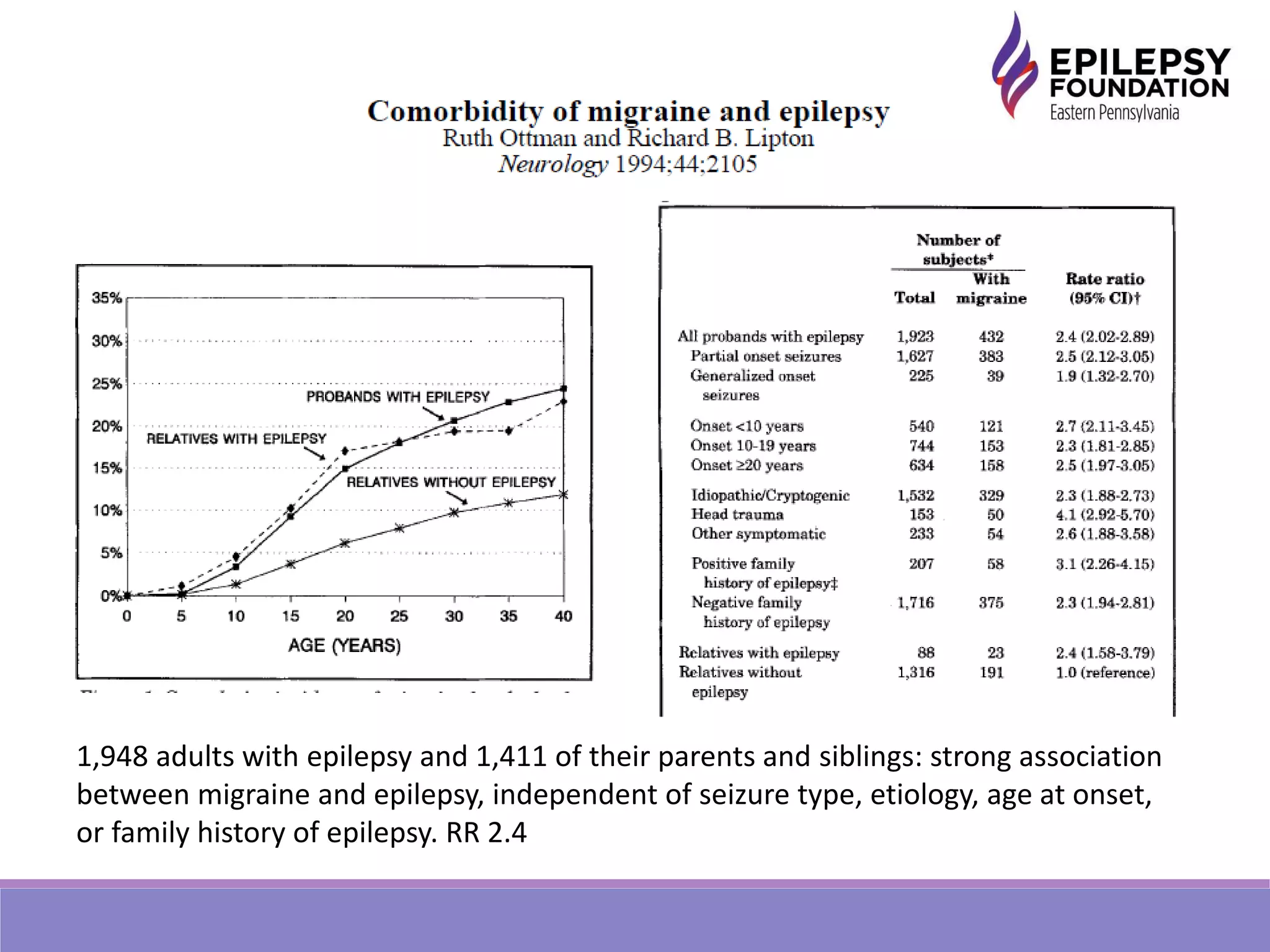
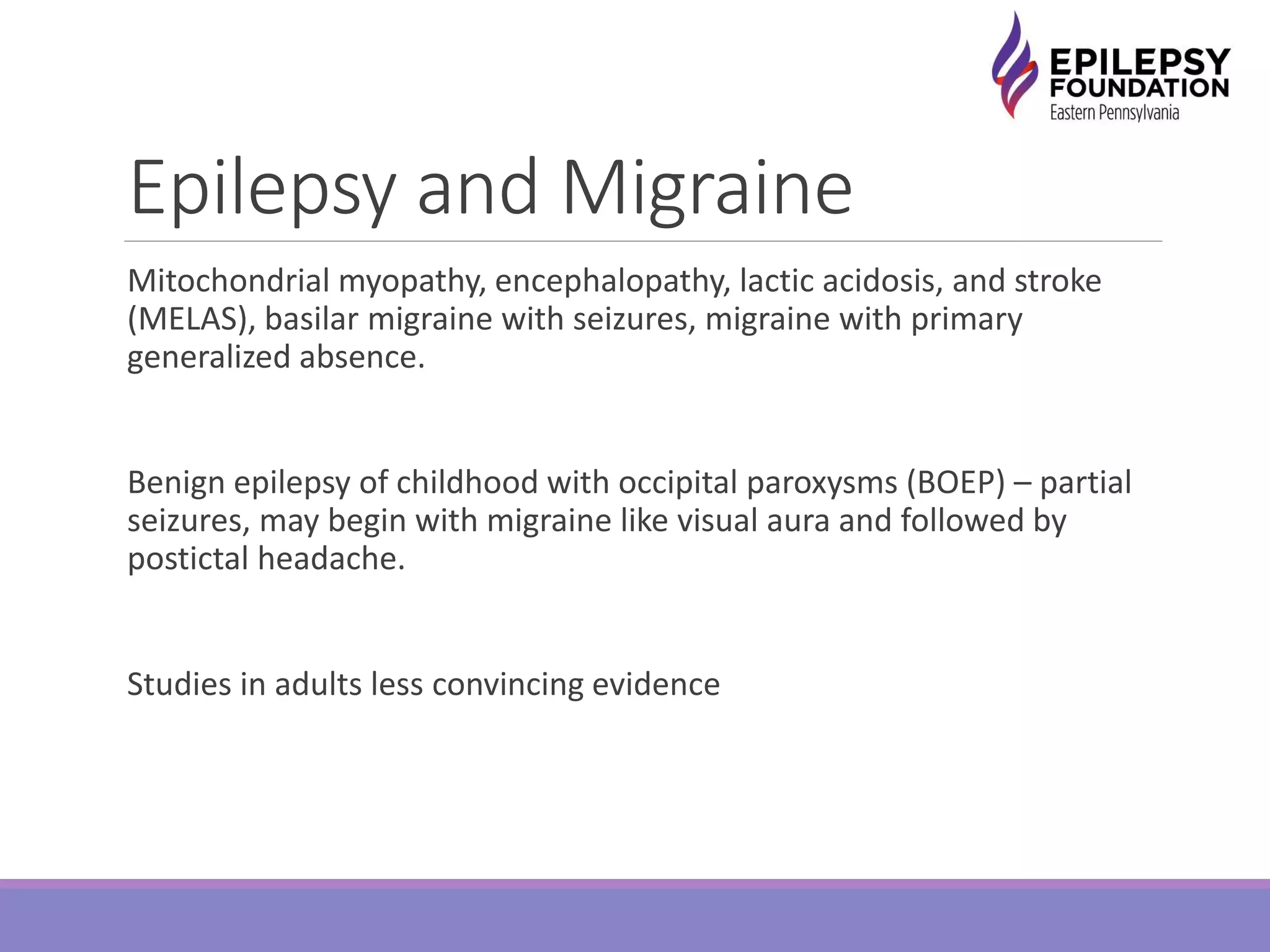
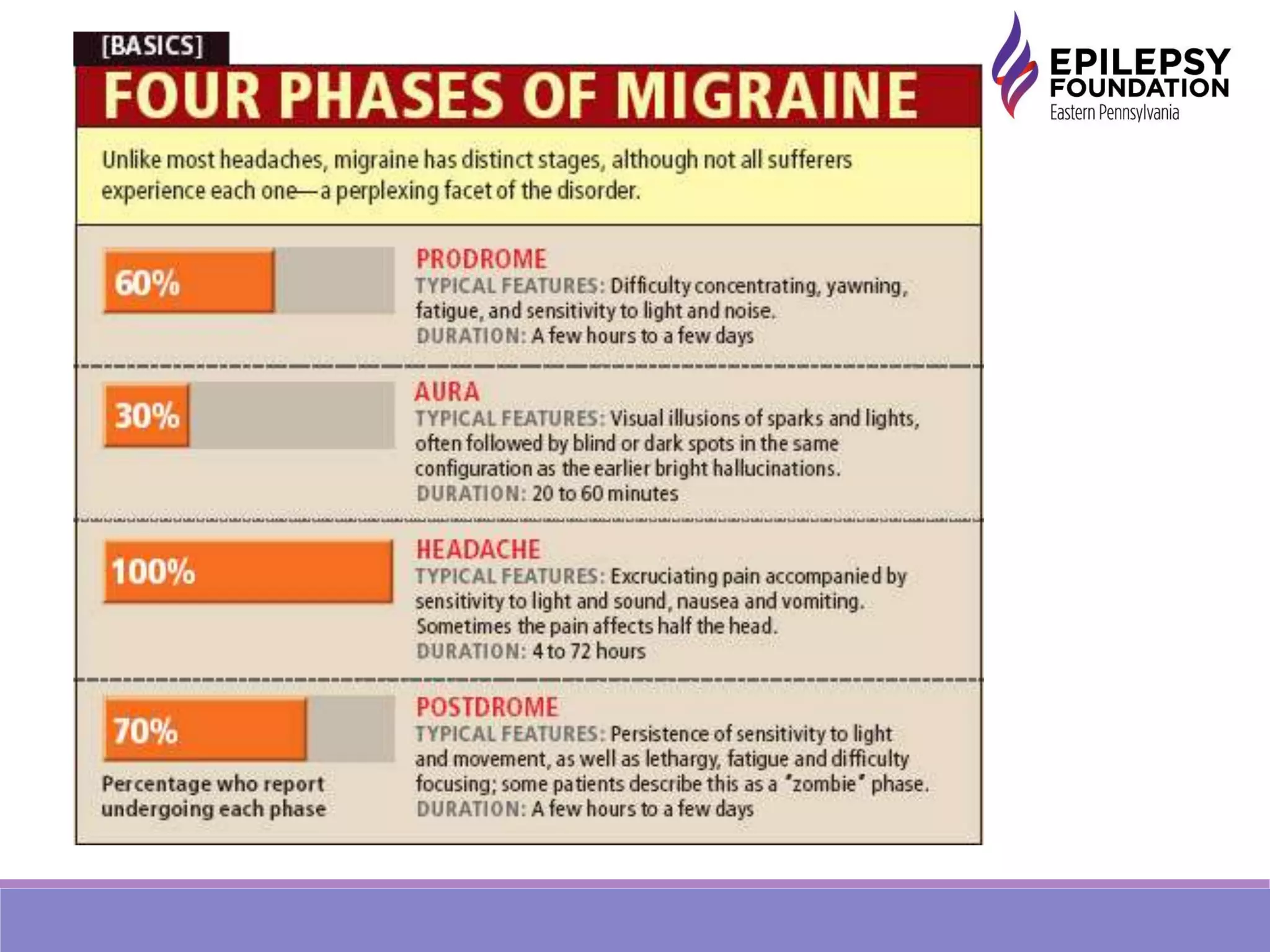
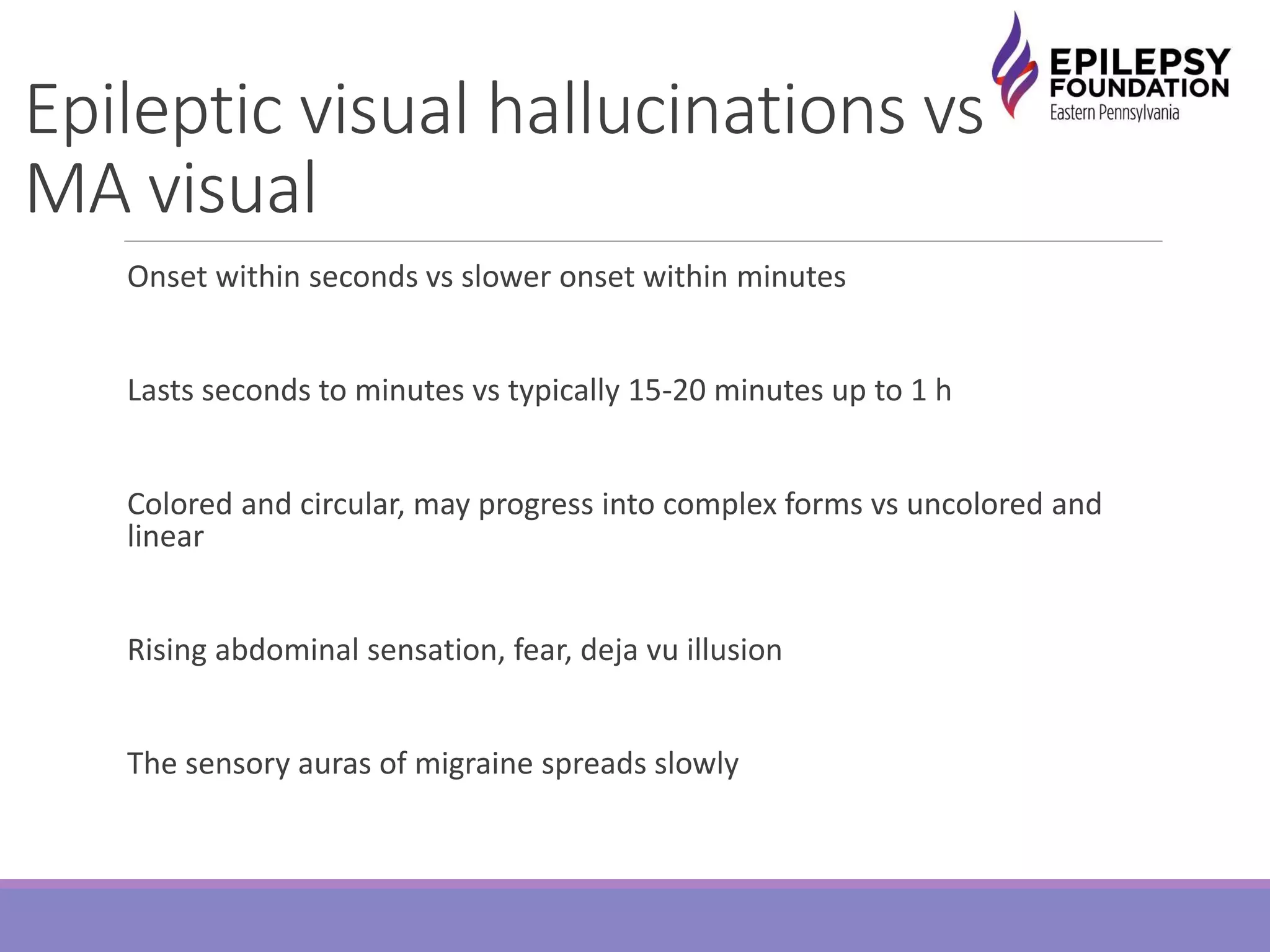
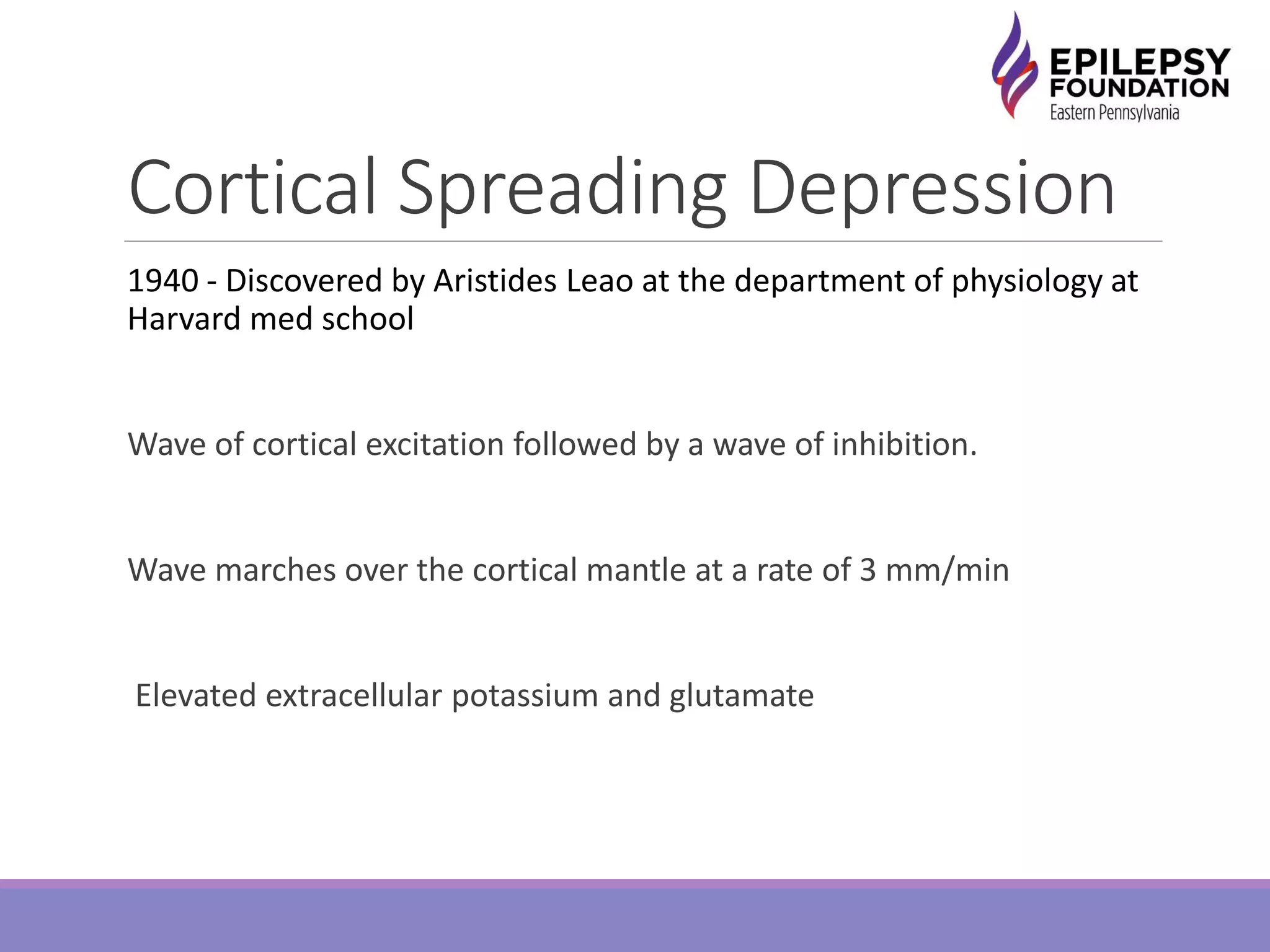
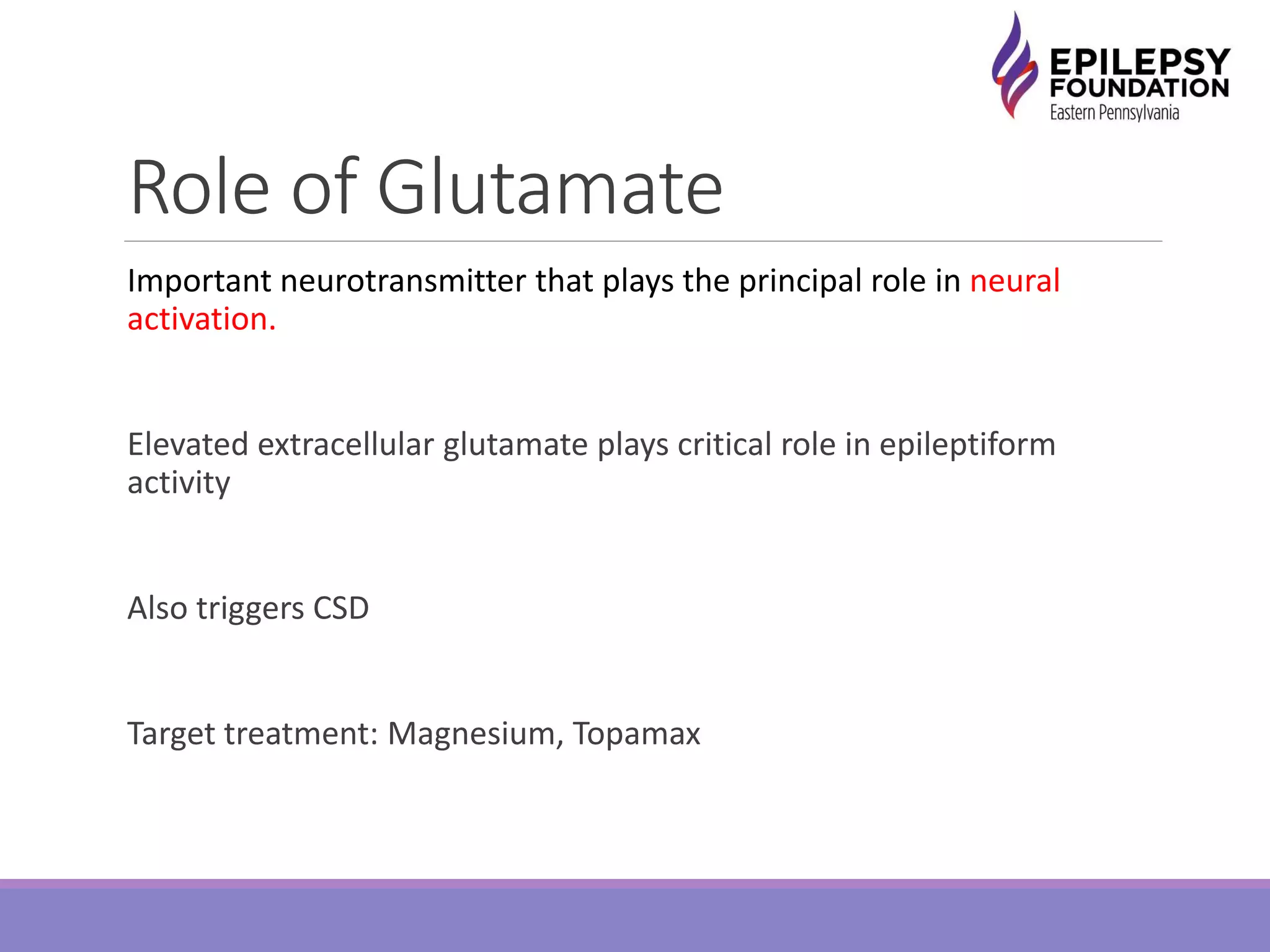
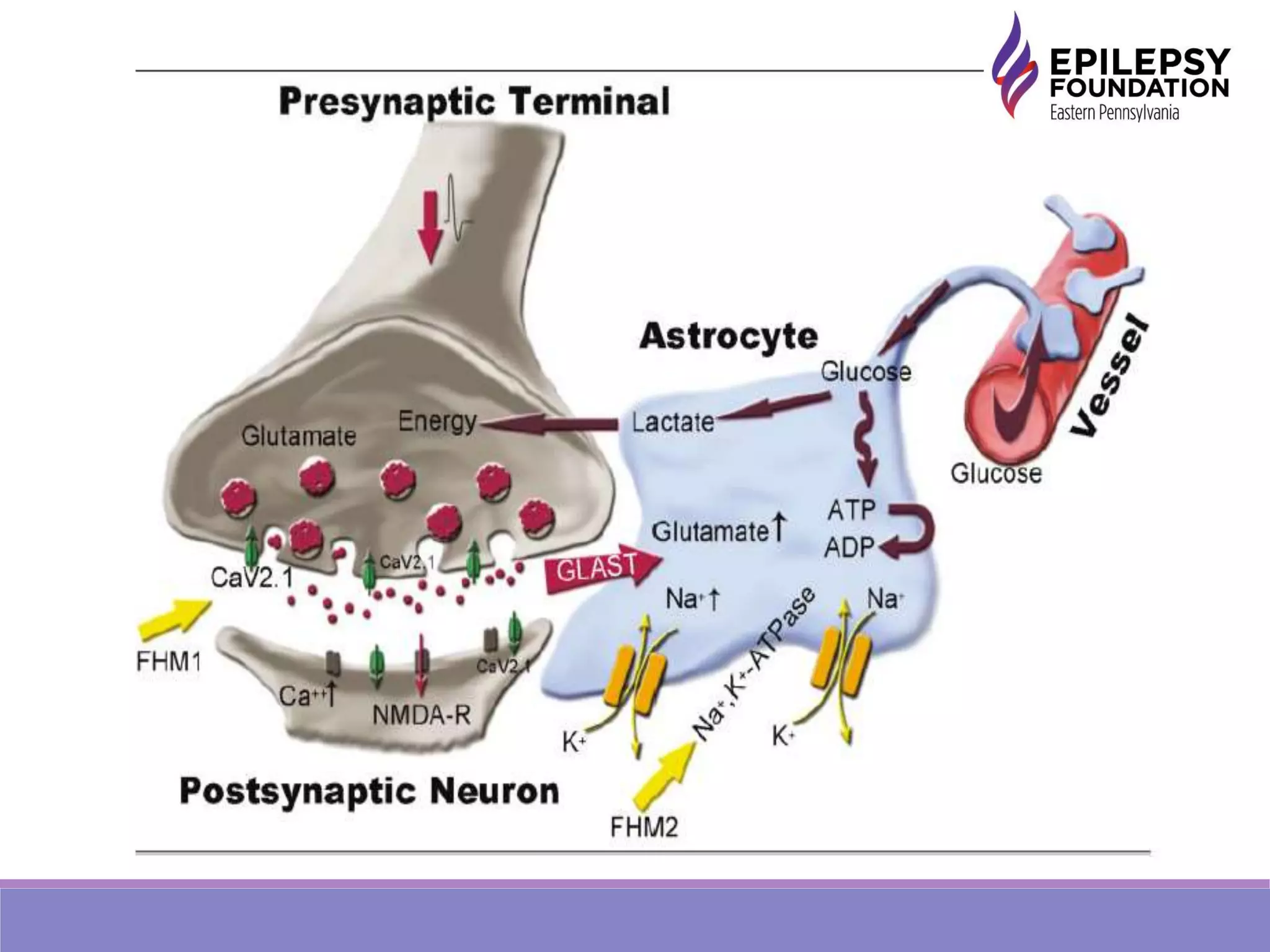
Headache and epilepsy are commonly comorbid conditions that share underlying pathophysiological mechanisms. About 5-10% of those with migraine have epilepsy, and 8-15% of those with epilepsy experience migraine. Both involve neuronal hyperexcitability that can trigger cortical spreading depression or seizures. Genetic channelopathies like FHM types 1-3 alter neuronal calcium and sodium channel function, lowering seizure and migraine thresholds. Antiepileptic drugs like levetiracetam and zonisamide can treat both conditions. Careful history is needed to identify pre-ictal headaches in those with epilepsy and evaluate for epilepsy in migraine patients due to medication interactions.
![Epilepsy and Headache
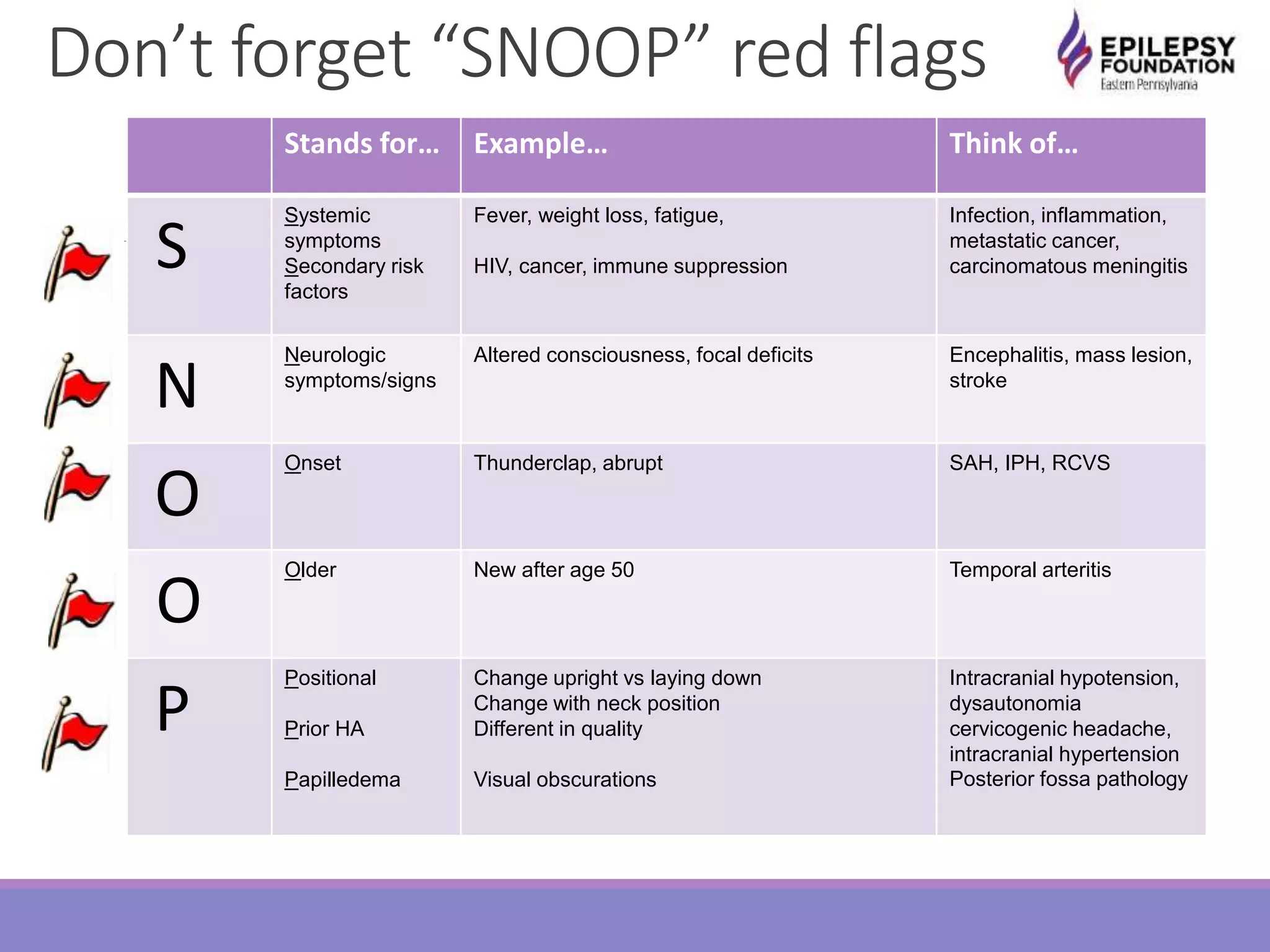
In the general population, the life time prevalence of headache is about
46 % [1] and that of migraine 10-22 % [2].
Bi-directional relationship one disorder increases the likelihood that
the other is also present.
1 to 17% (median of 5.9%) with migraine have epilepsy
8 to 15% with epilepsy have migraine](https://image.slidesharecdn.com/haepilepsywrobelgoldberg2014updated2015-150707203711-lva1-app6892/75/Epilepsy-and-Headaches-7-2048.jpg)





![References
[1] Stovner L, Hagen K, Jensen R, et al. The global burden of headache: a documentation of
headache prevalence and disability worldwide. Cephalalgia. 2007;27(3):193–210.
[2] Smitherman TA, Burch R, Sheikh H, Loder E. The prevalence, impact, and treatment of
migraine and severe headaches in the United States: a review of statistics from national
surveillance studies. Headache. 2013
[3] MacDonald BK, Cockerell OC, Sander JW, Shorvon SD. The incidence and lifetime
prevalence of neurological disorders in a prospective community-based study in the UK.
Brain. 2000;123:665–76.
[4] Forsgren L, Beghi E, Oun A, Sillanpää M. The epidemiology of epilepsy in Europe - a
systematic review. Eur J Neurol. 2005;12(4):245–53.
[5] Sander JW. The epidemiology of epilepsy revisited. Curr Opin
Neurol. 2003;16(2):165–70.
[6] Kelley SA, Hartman AL, Kossoff EH. Comorbidity of migraine in
children presenting with epilepsy to a tertiary care center. Neurology. 2012;79(5):468–73.](https://image.slidesharecdn.com/haepilepsywrobelgoldberg2014updated2015-150707203711-lva1-app6892/75/Epilepsy-and-Headaches-36-2048.jpg)
![References
[7] Winawer MR, Connors R. Evidence for a shared genetic susceptibility to migraine and
epilepsy. Epilepsia. 2013.
[8] Crepeau AZ. Migralepsy: a borderland of wavy lines. Curr Neurol Neurosci Rep. 2014
Feb;14(2):427
[9] Schon F, Blau JN. J Neurol Neurosurg Psychiatry. Post-epileptic headache and migraine.
1987 Sep;50(9):1148-52.
[10] Sethi NK, Ulloa CM, Solomon GE, Lopez L. Diagnostic utility of routine EEG study in
identifying seizure as the etiology of the index event in patients referred with a diagnosis of
migraine and not otherwise specified headache disorders. Clin EEG Neurosci. 2012
Oct;43(4):323-5.
[11] Marks DA, Ehrenberg BL. Migraine-related seizures in adults with epilepsy, with EEG
correlation. Neurology. 1993 Dec;43(12):2476-83.
[12] Bigal ME, Lipton RB, Cohen J, Silberstein SD. Epilepsy and migraine. Epilepsy Behav.
2003 Oct;4 Suppl 2:S13-24.
[13] Ottman R, Lipton RB Comorbidity of migraine and epilepsy. Neurology 1994
Nov;44(11):2105-10.](https://image.slidesharecdn.com/haepilepsywrobelgoldberg2014updated2015-150707203711-lva1-app6892/75/Epilepsy-and-Headaches-37-2048.jpg)