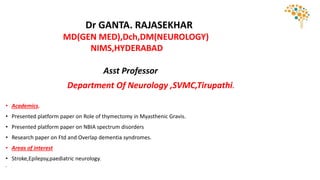
This document provides information on Dr. Ganta Rajasekhar's academic qualifications and areas of interest in neurology. It then discusses approaches to evaluating headache, classifications of primary and secondary headache disorders, migraine pathogenesis and management, tension-type headache, and trigeminal autonomic cephalalgias. Evaluation and treatment strategies for acute migraine, preventive migraine therapy, medication overuse headache, and special headache conditions are covered. Common questions in headache management are also addressed.