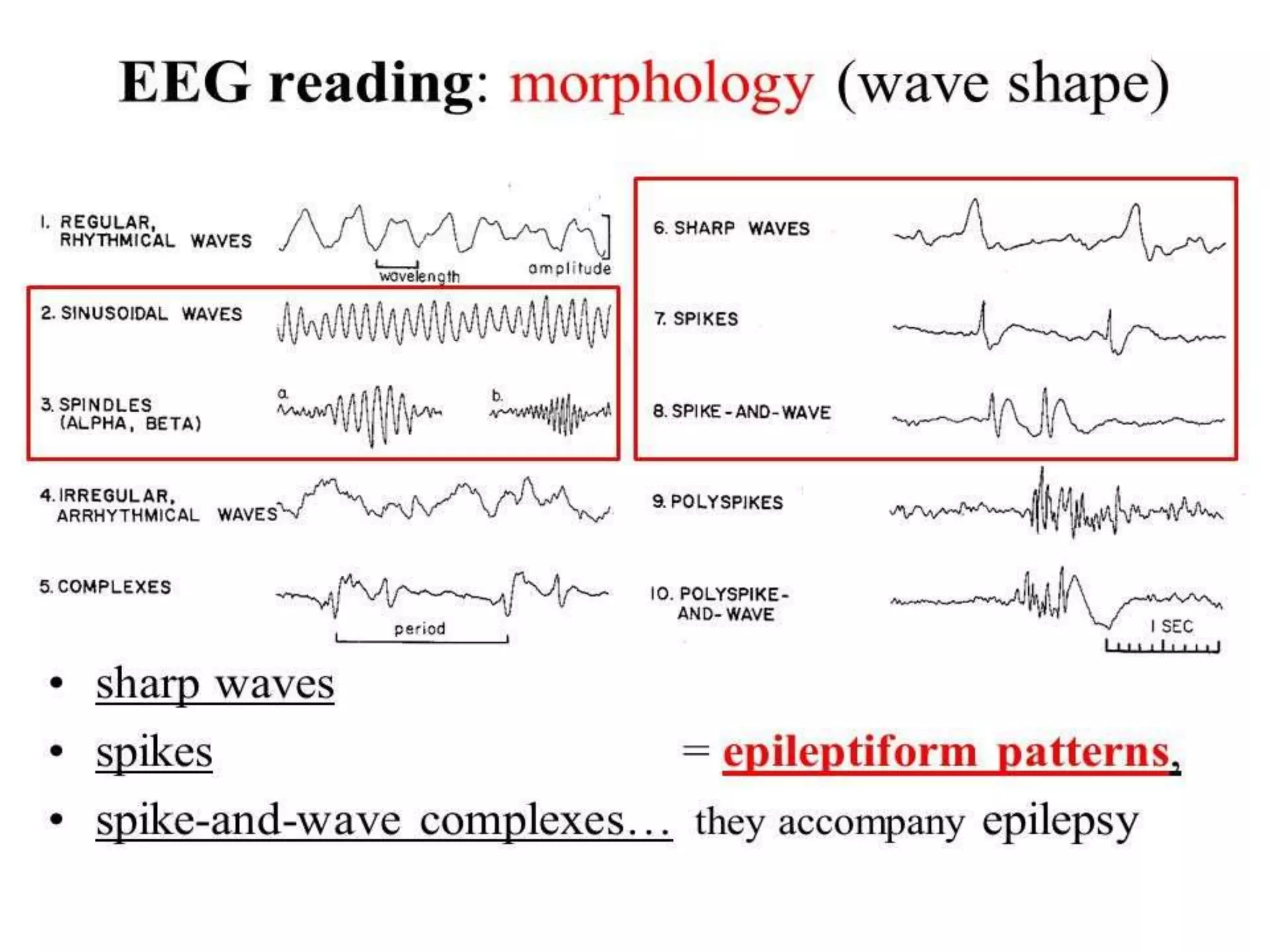
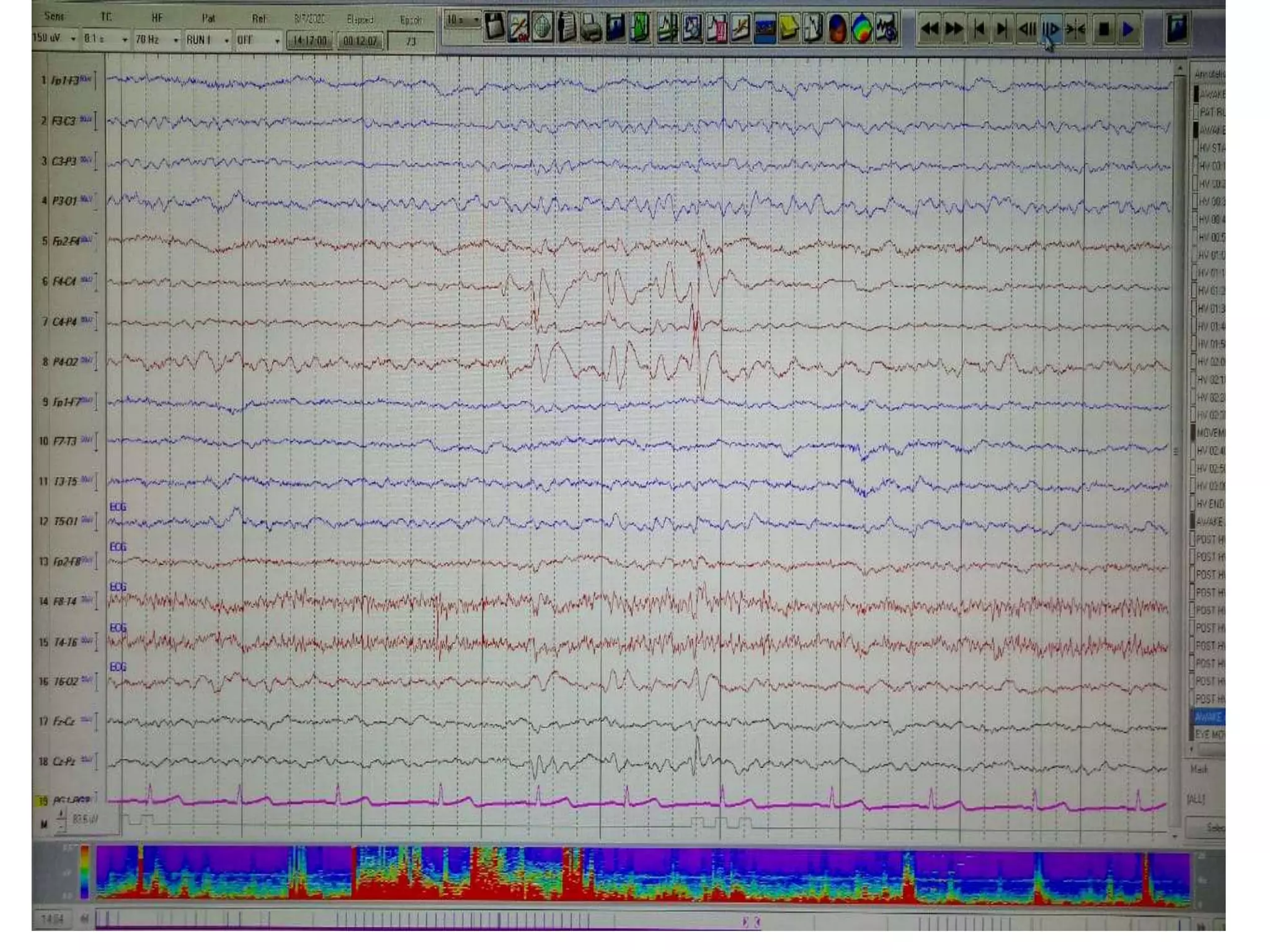
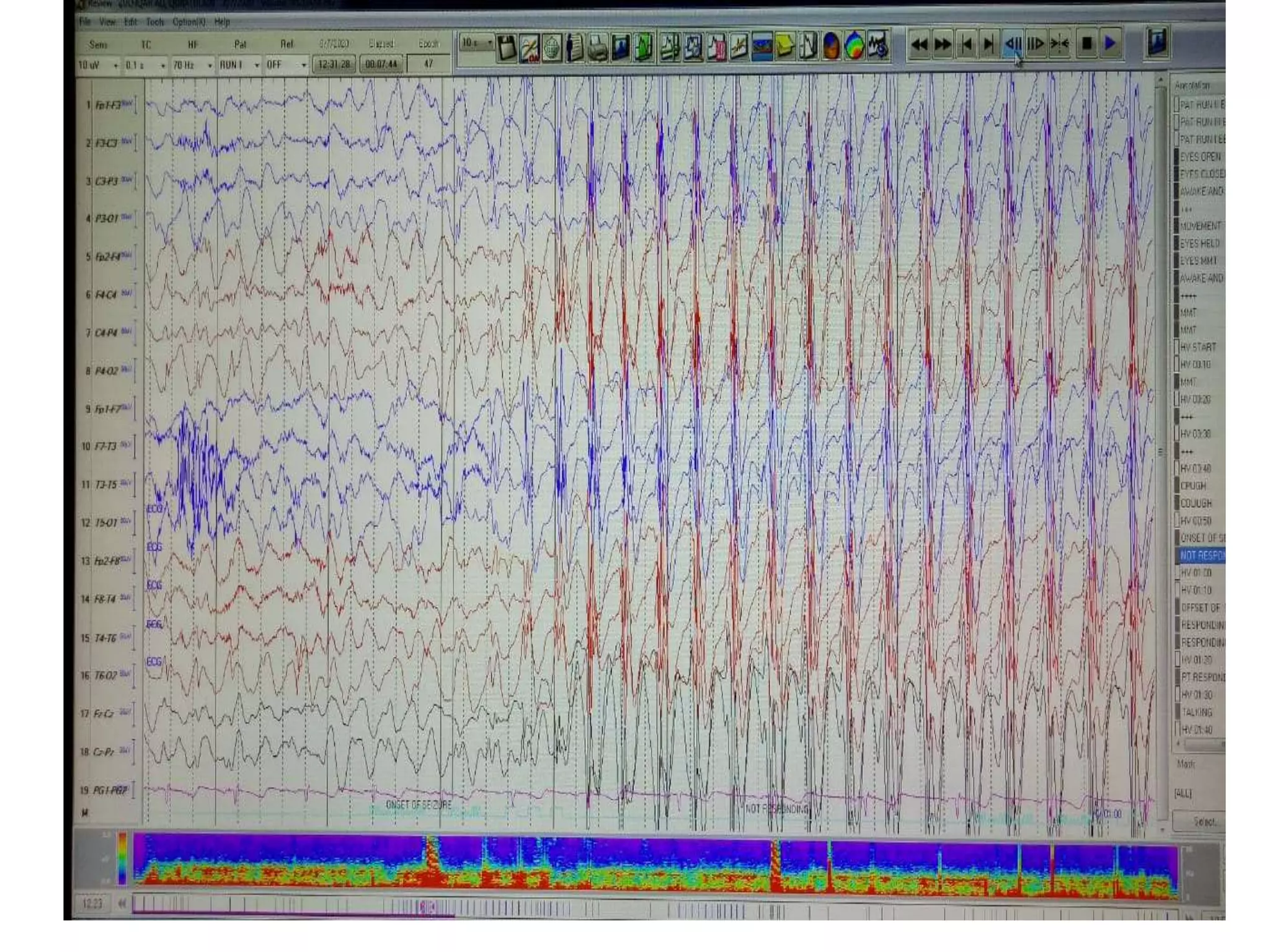
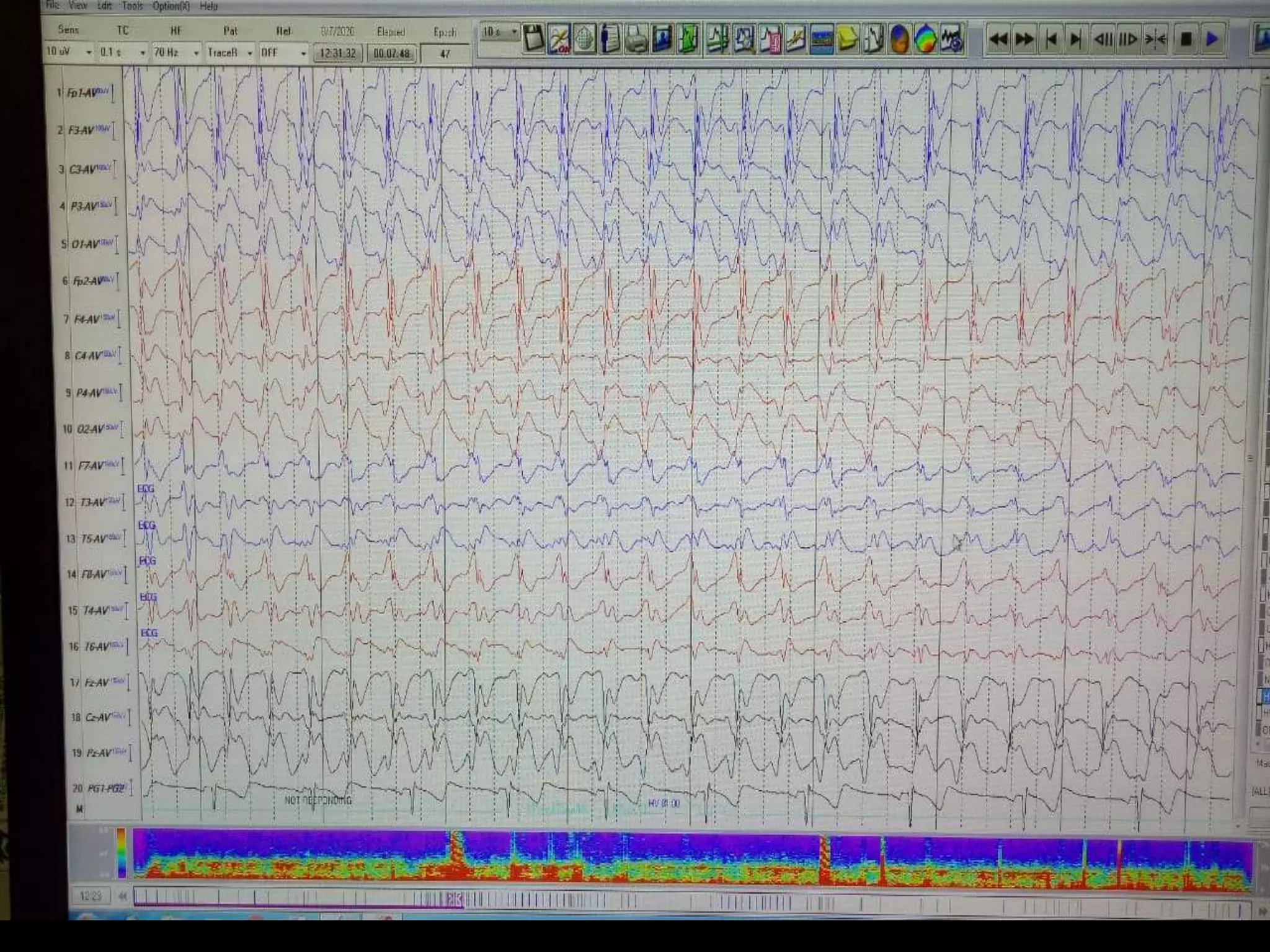
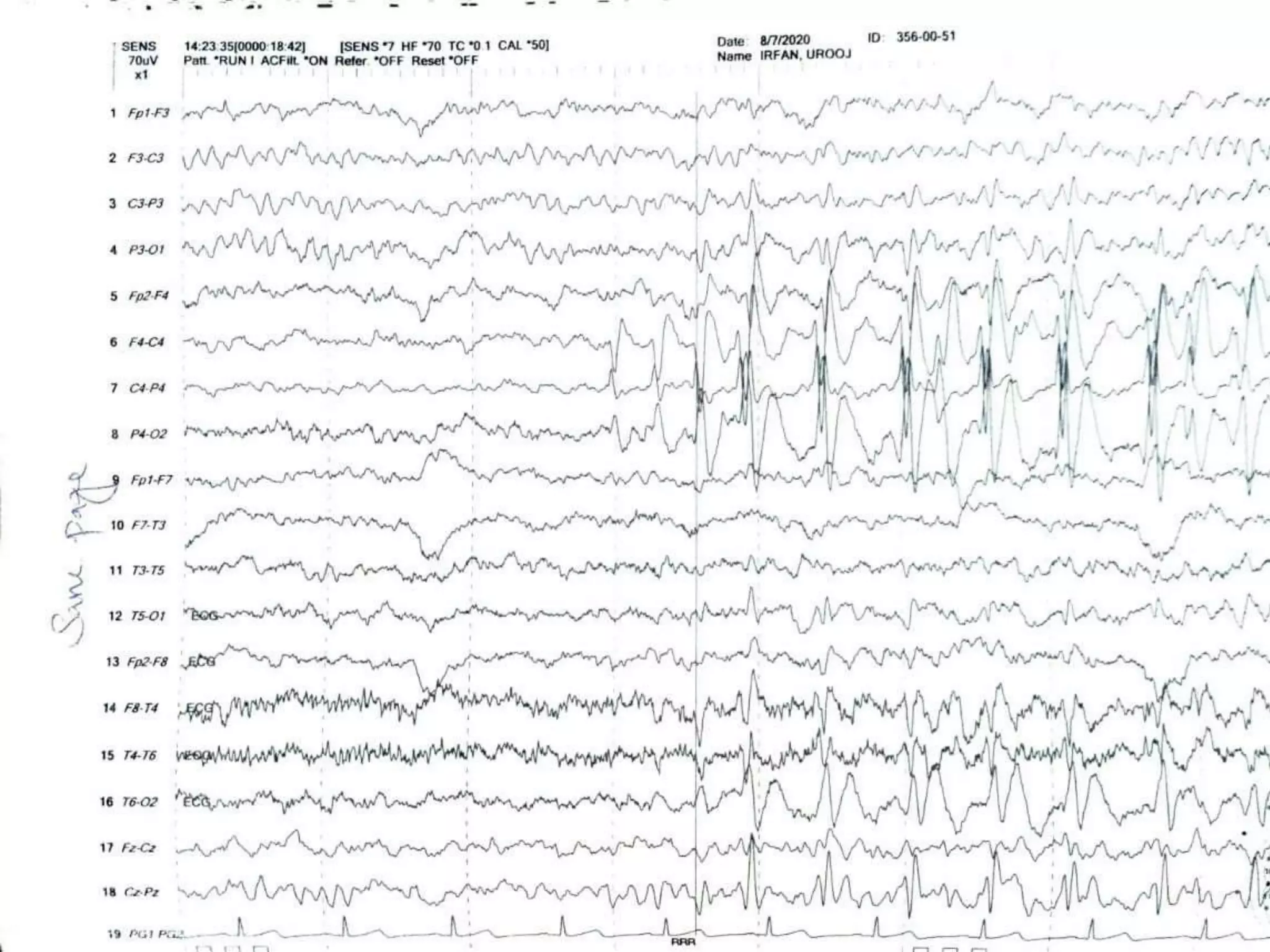
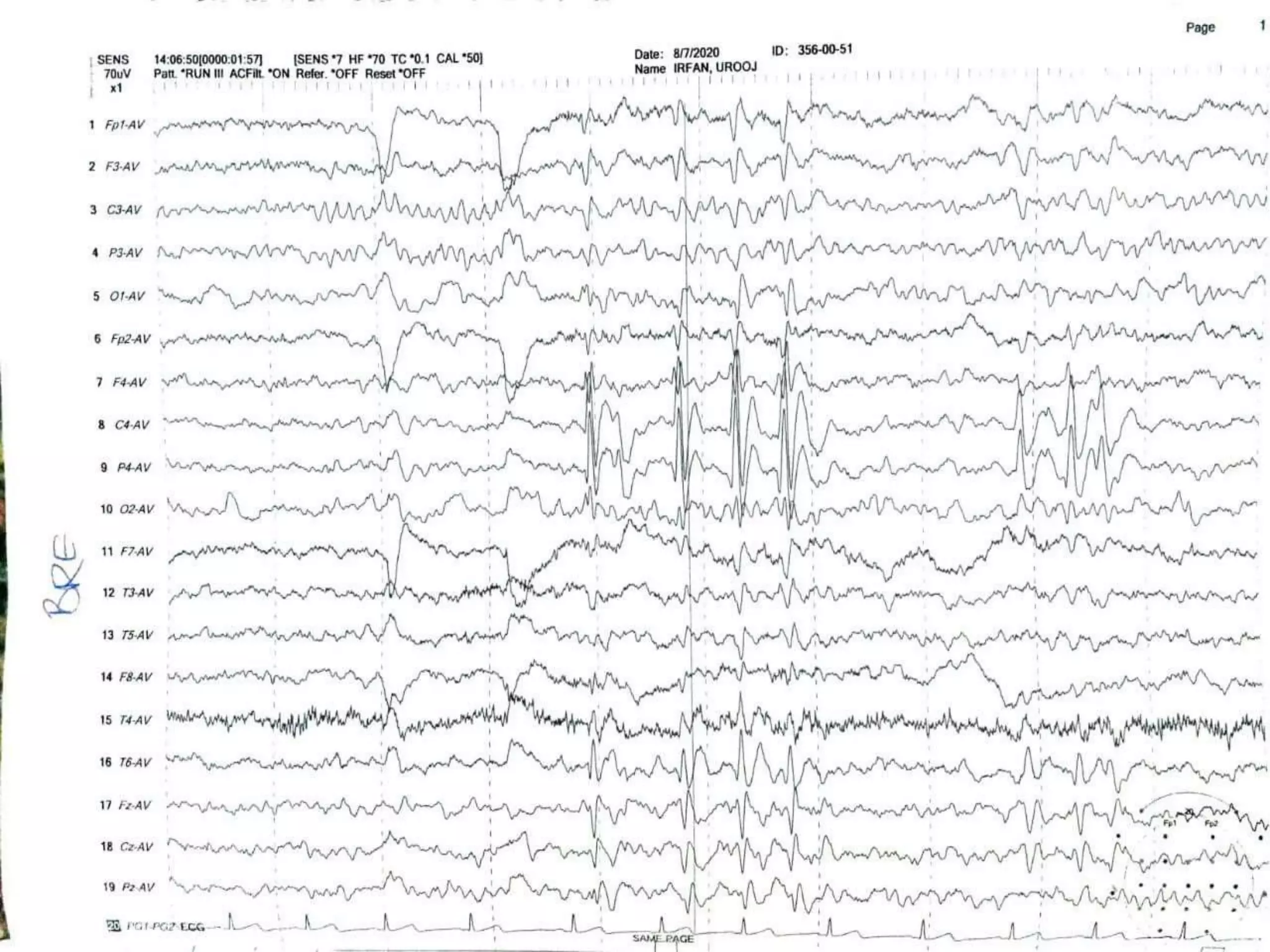
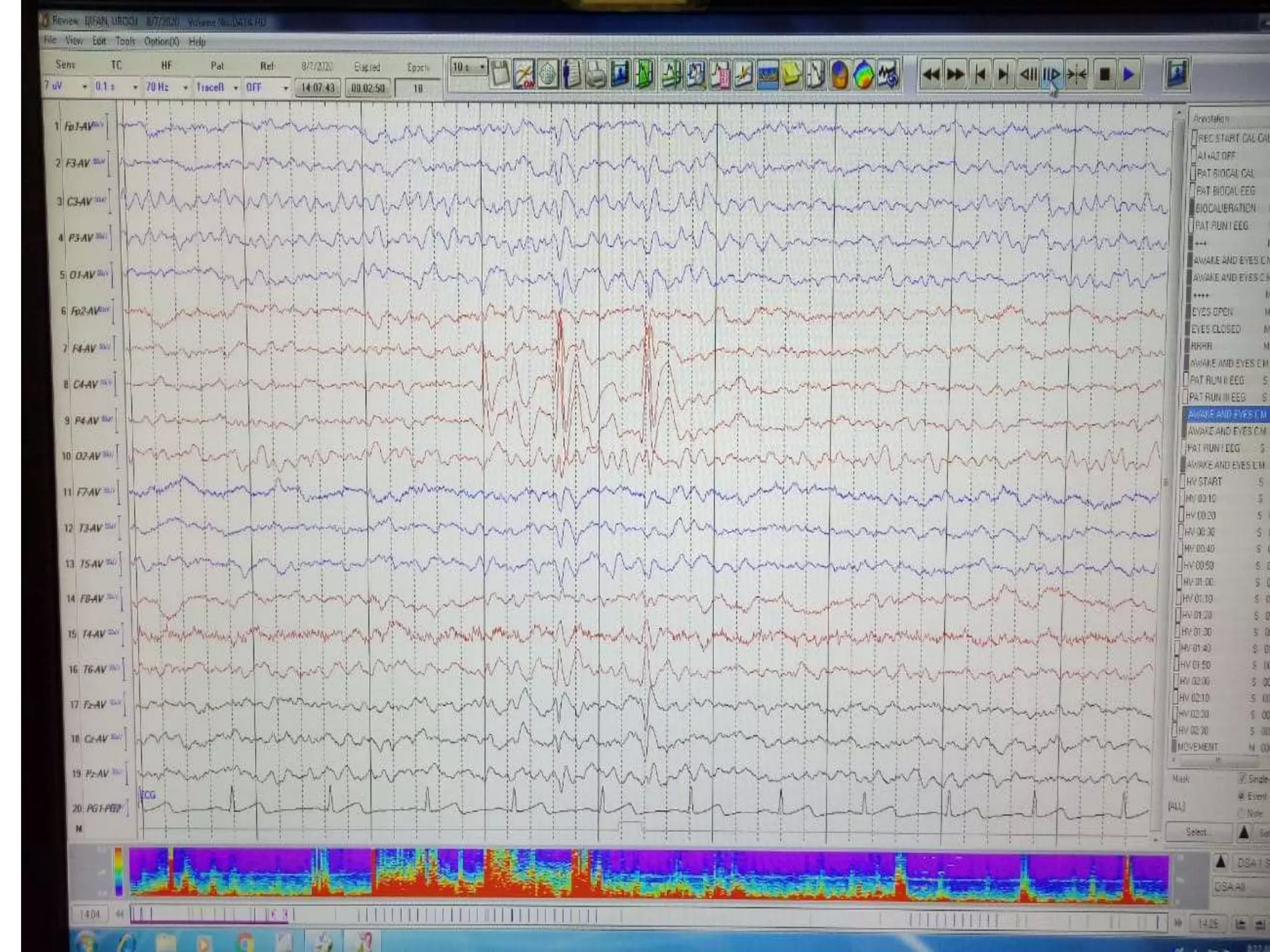
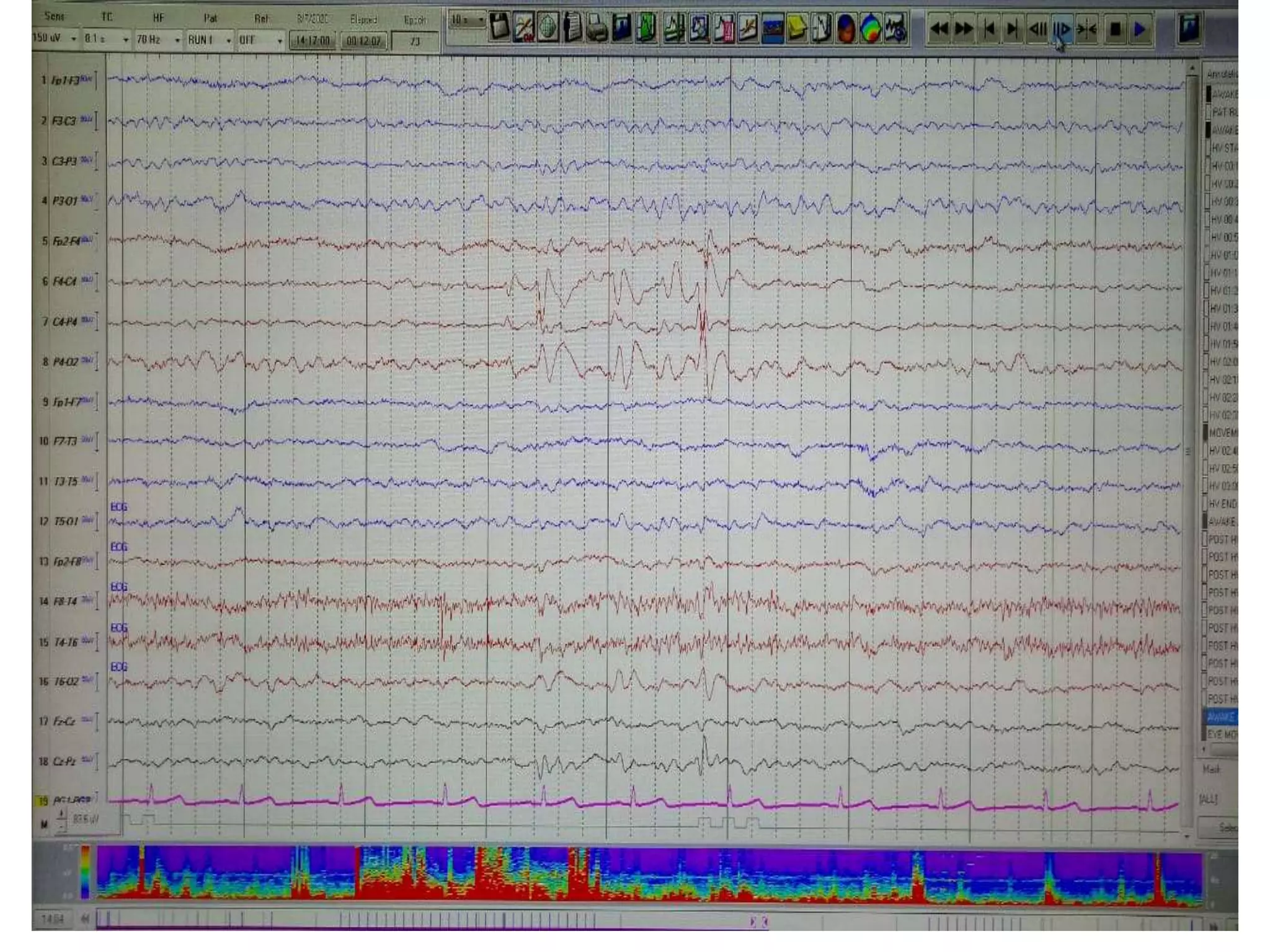
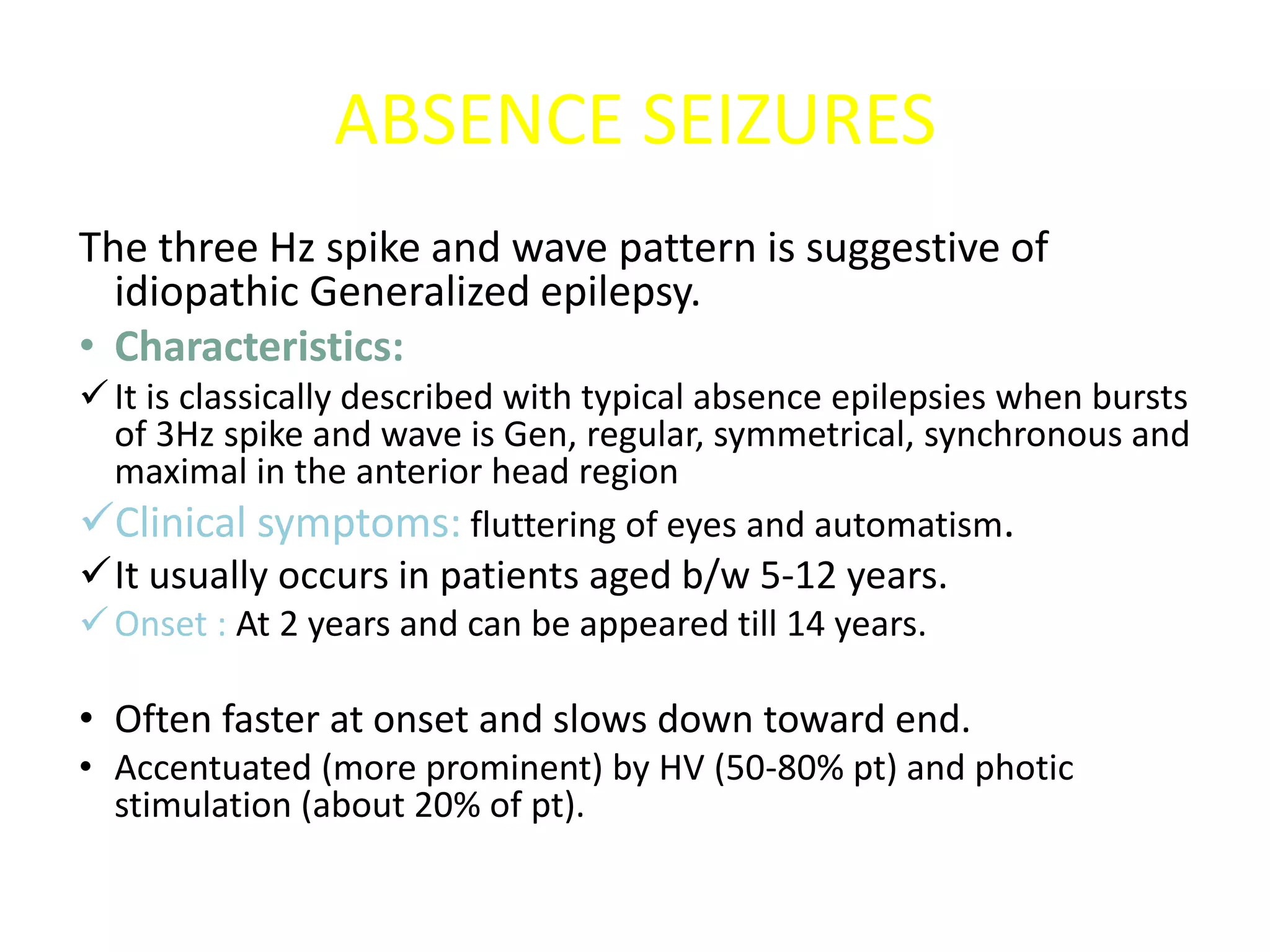
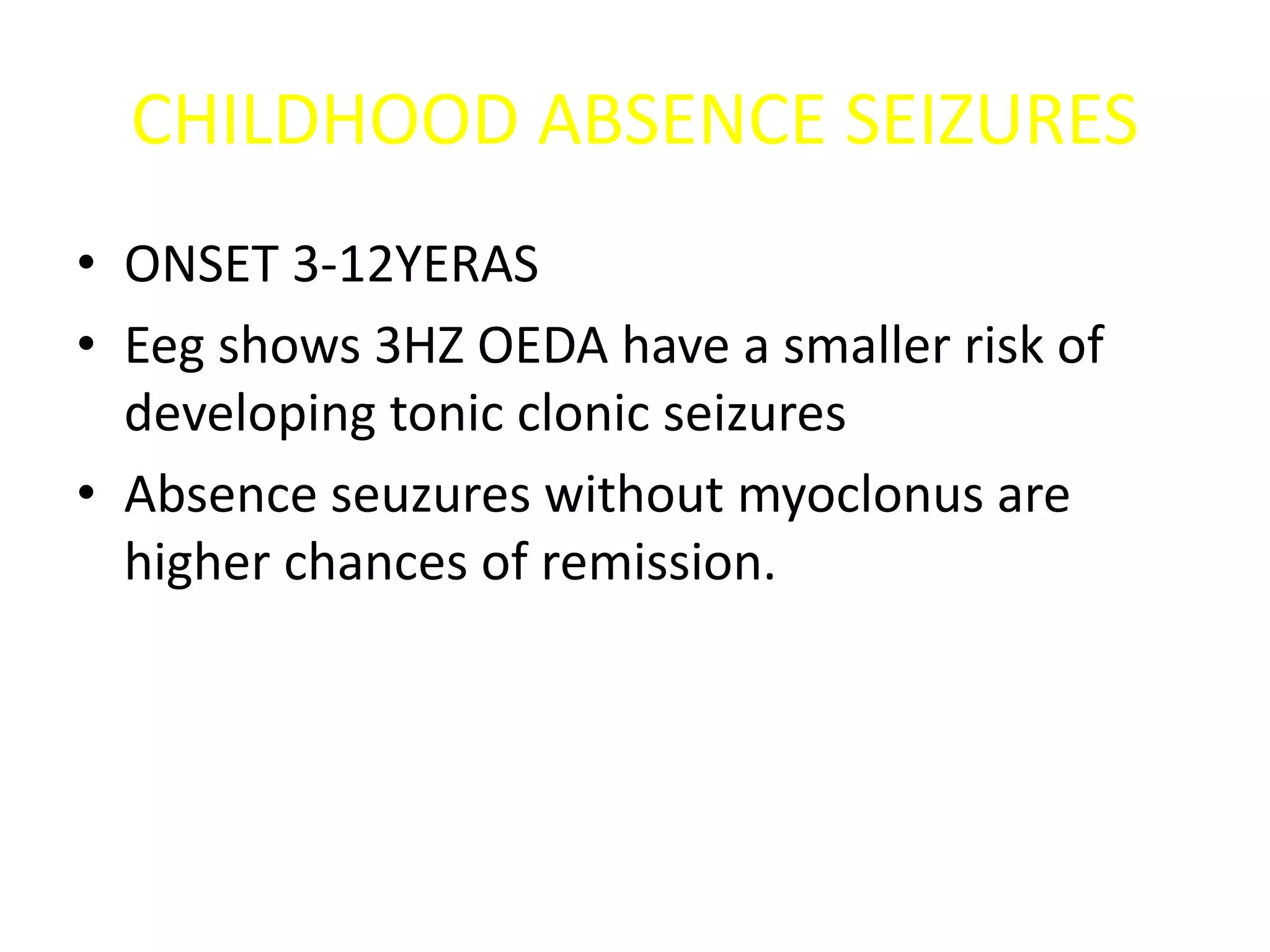
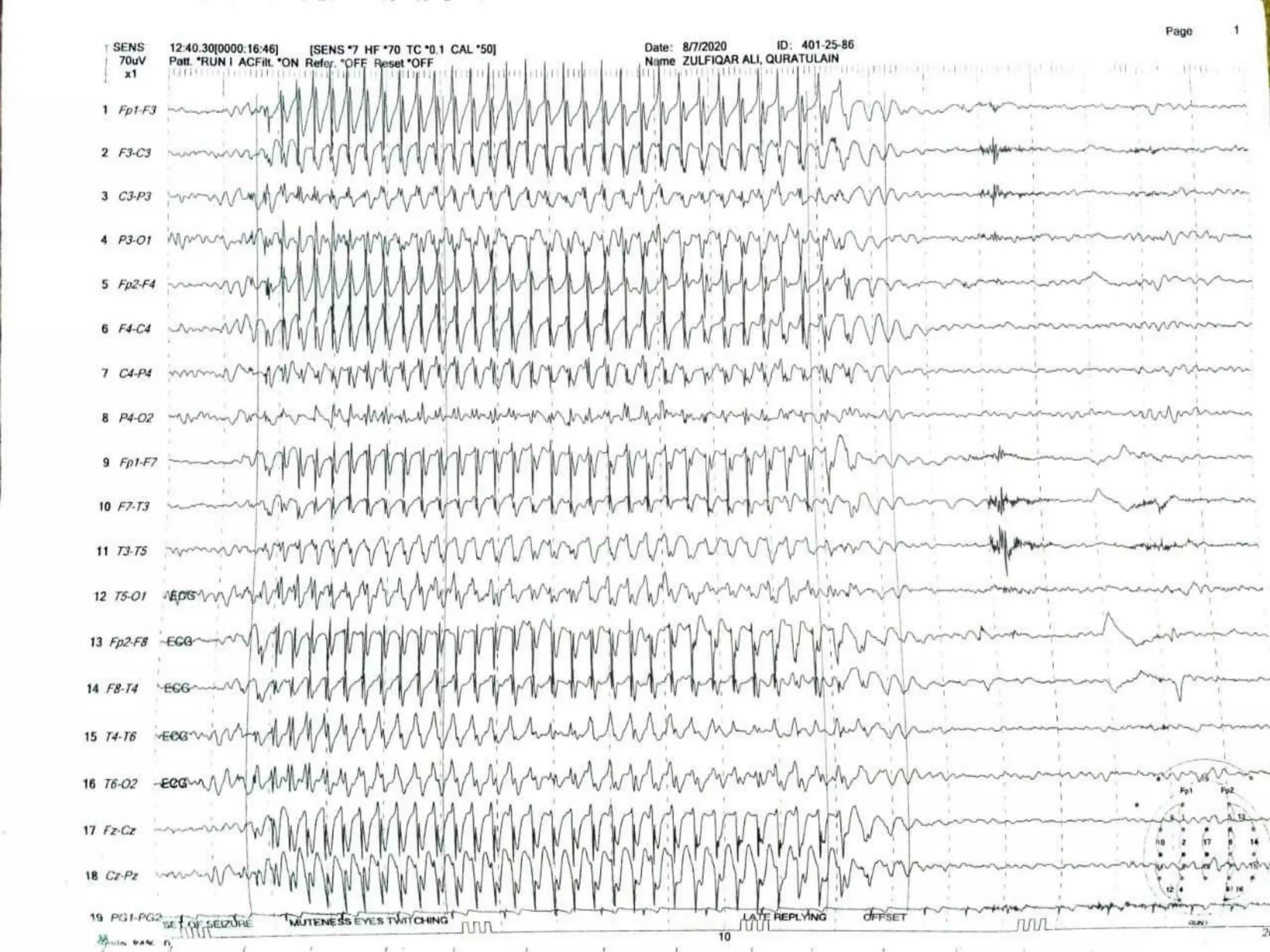
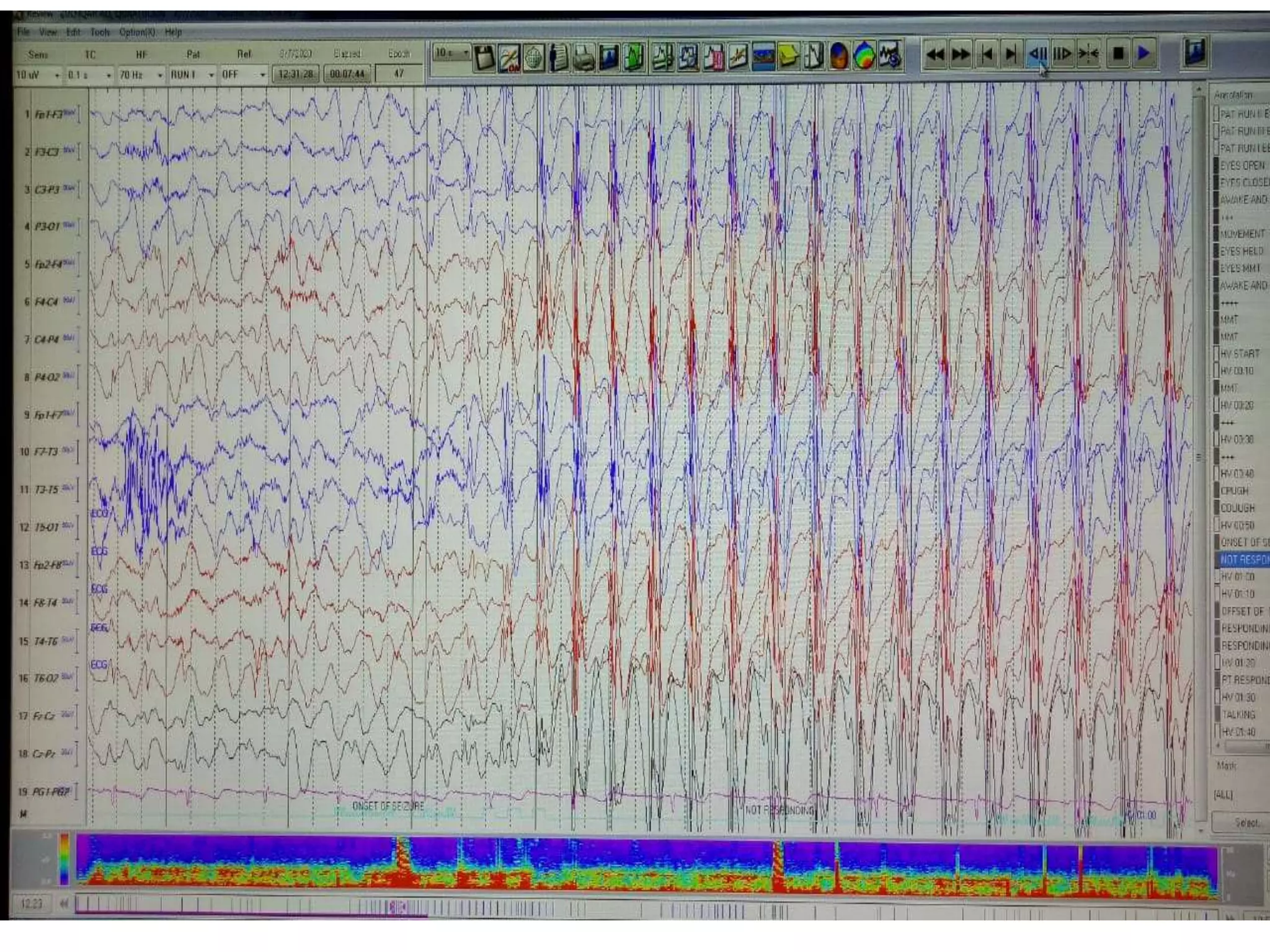
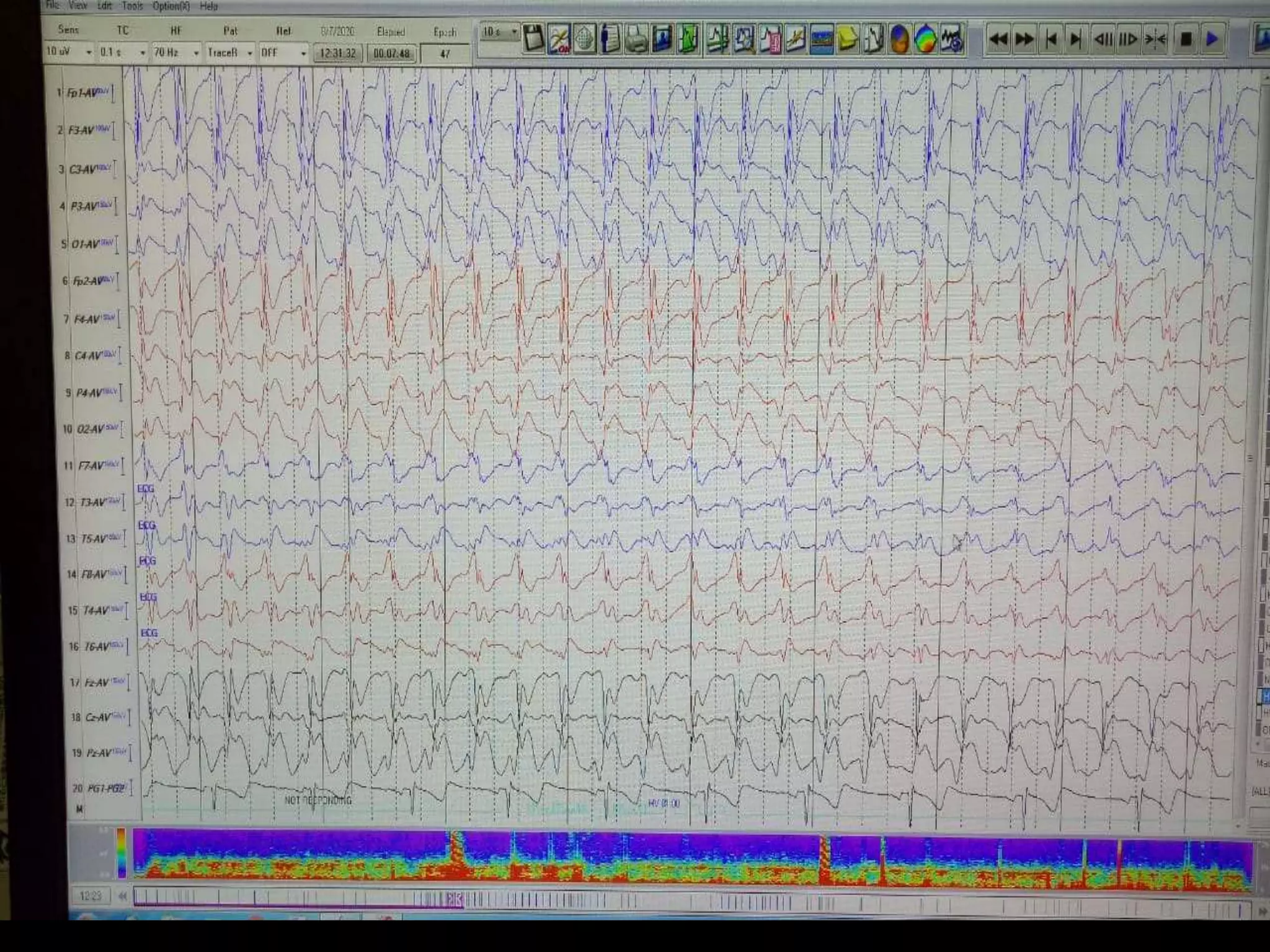
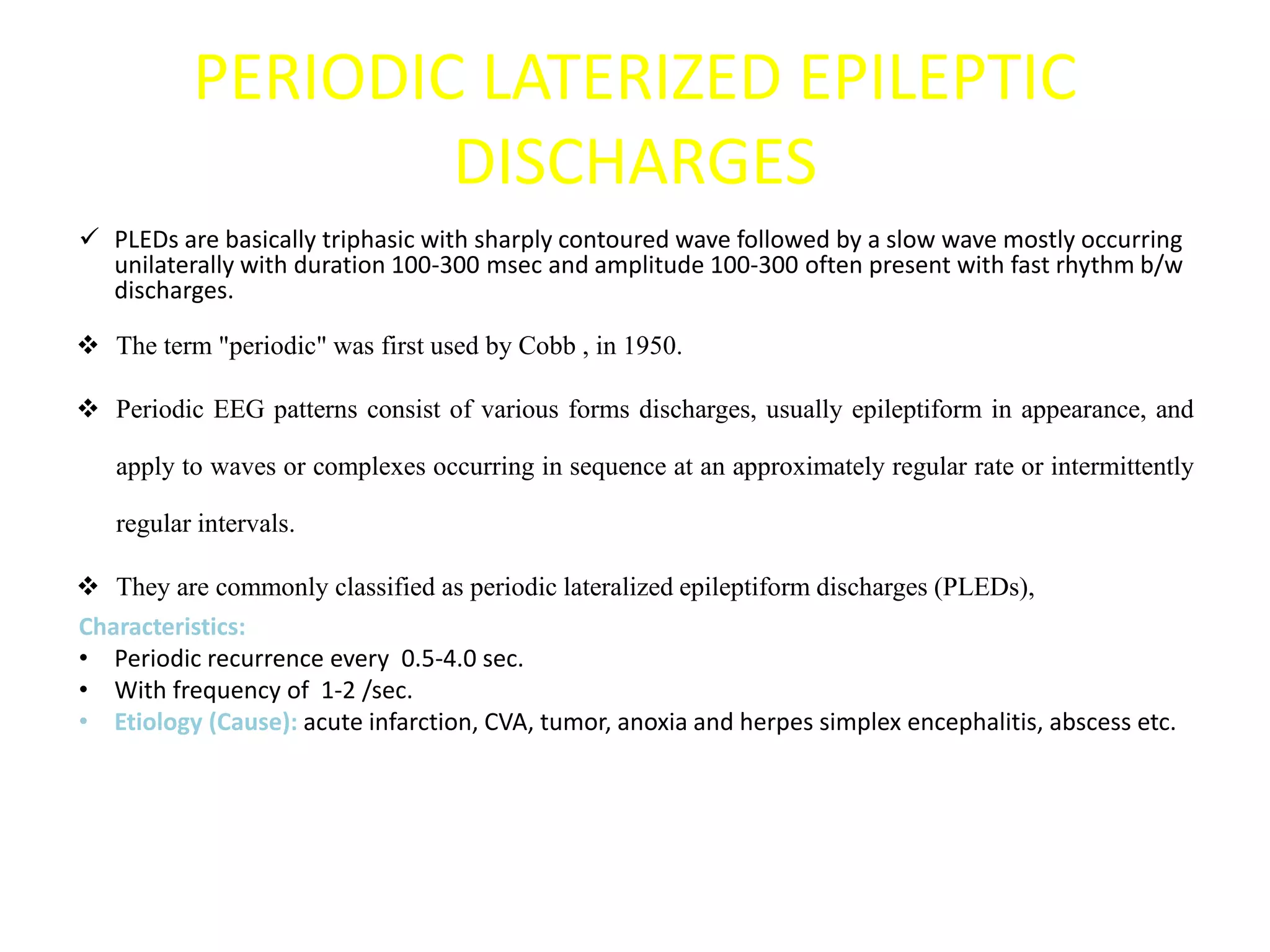
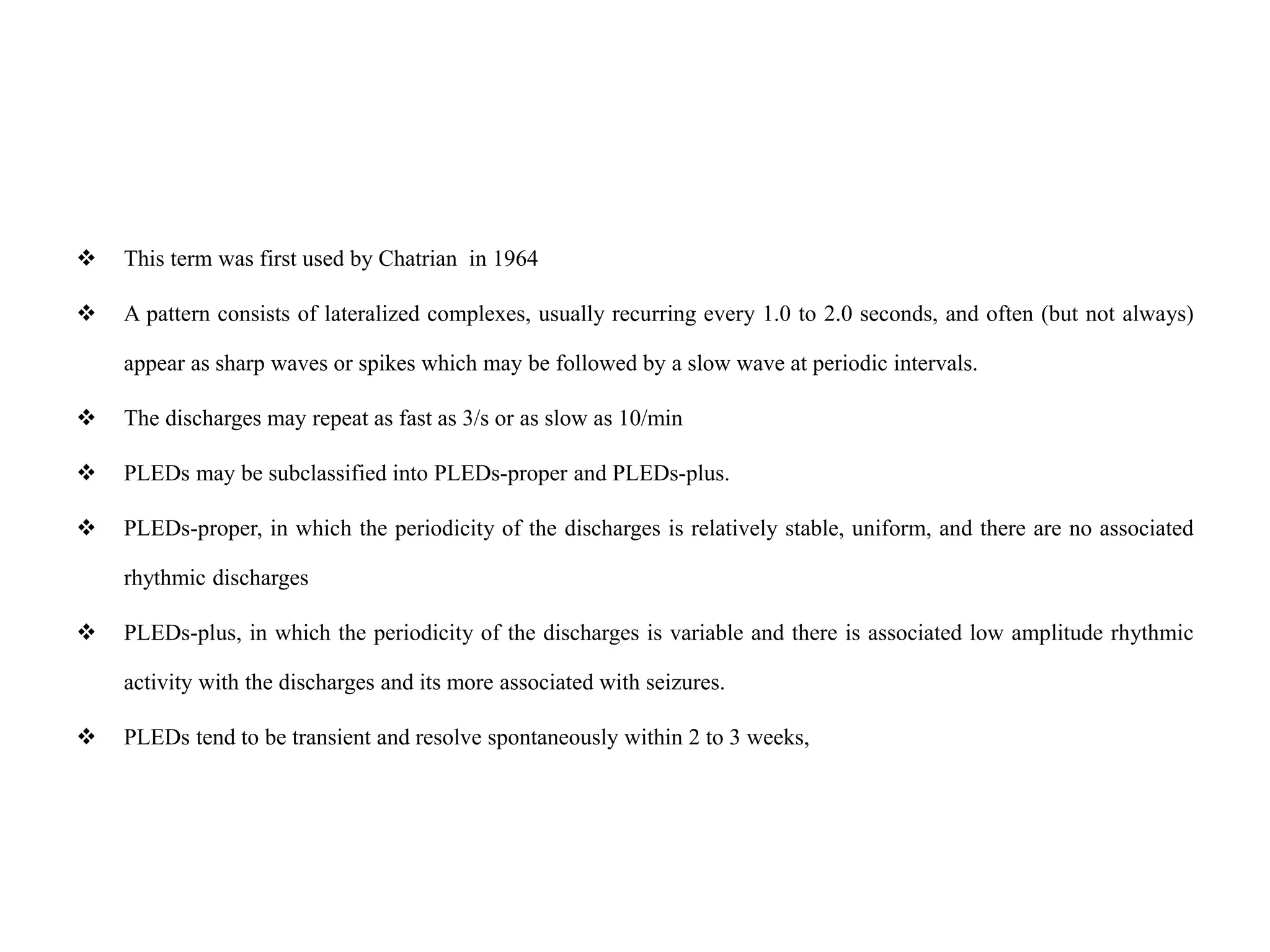
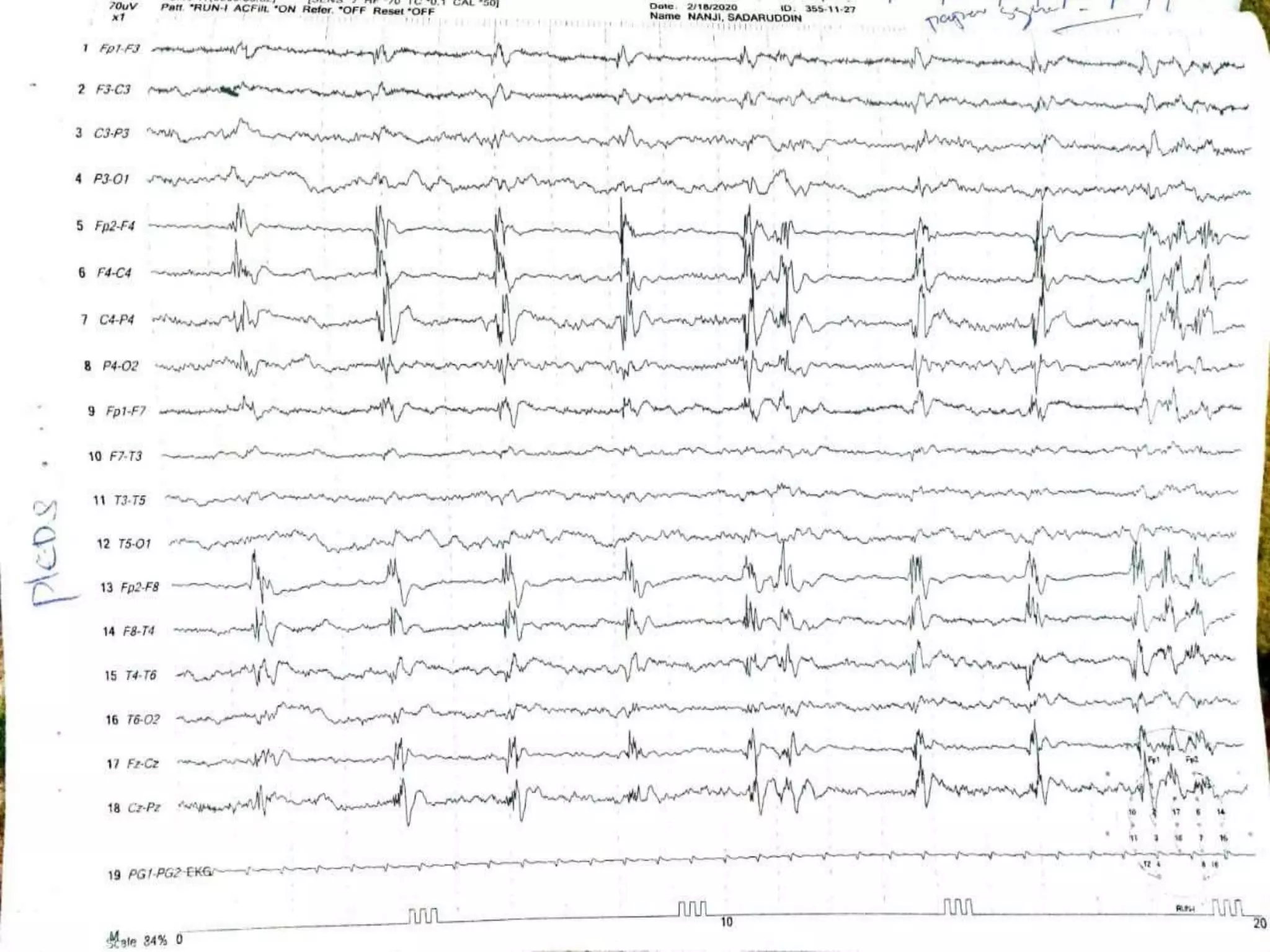
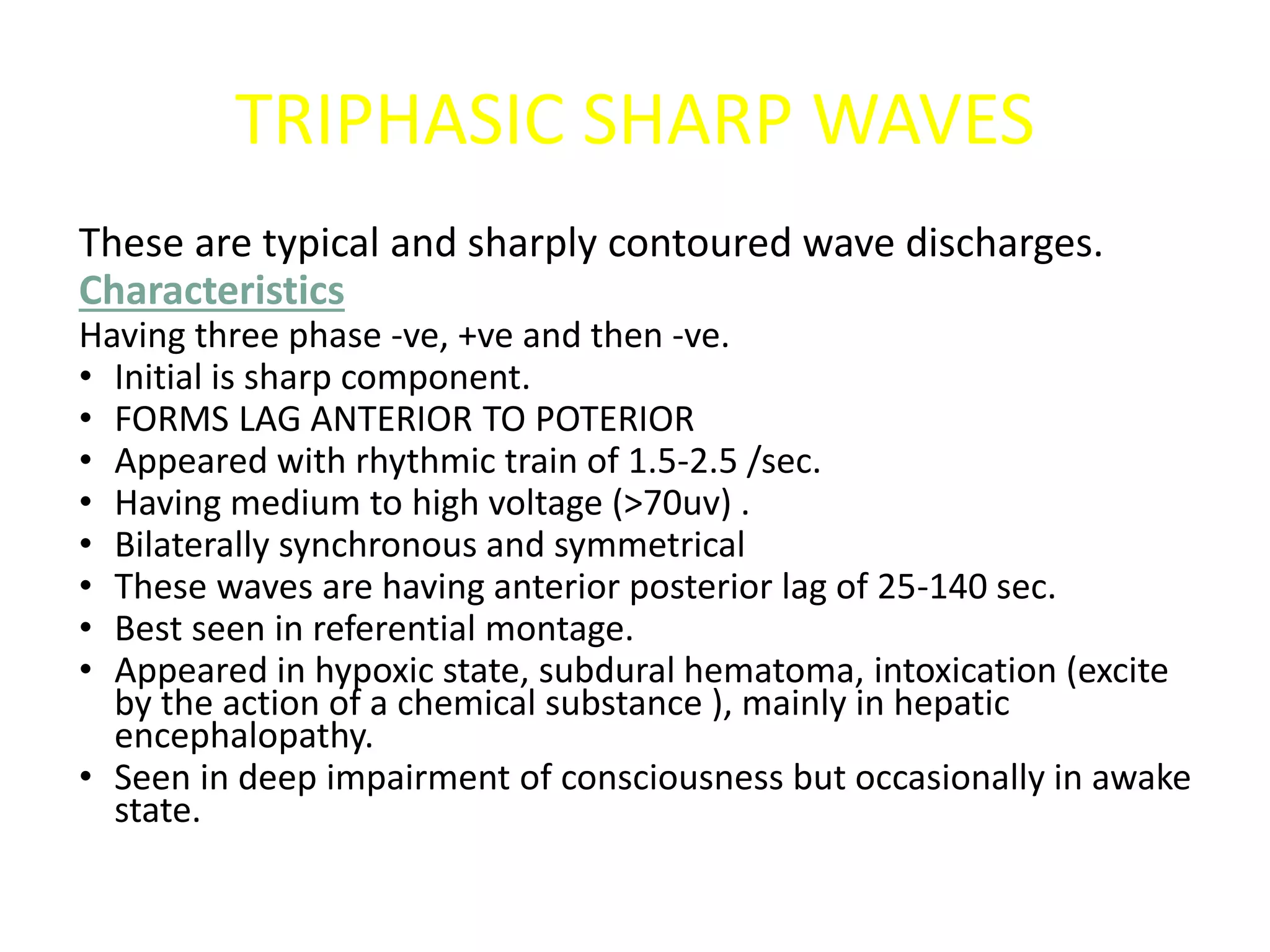
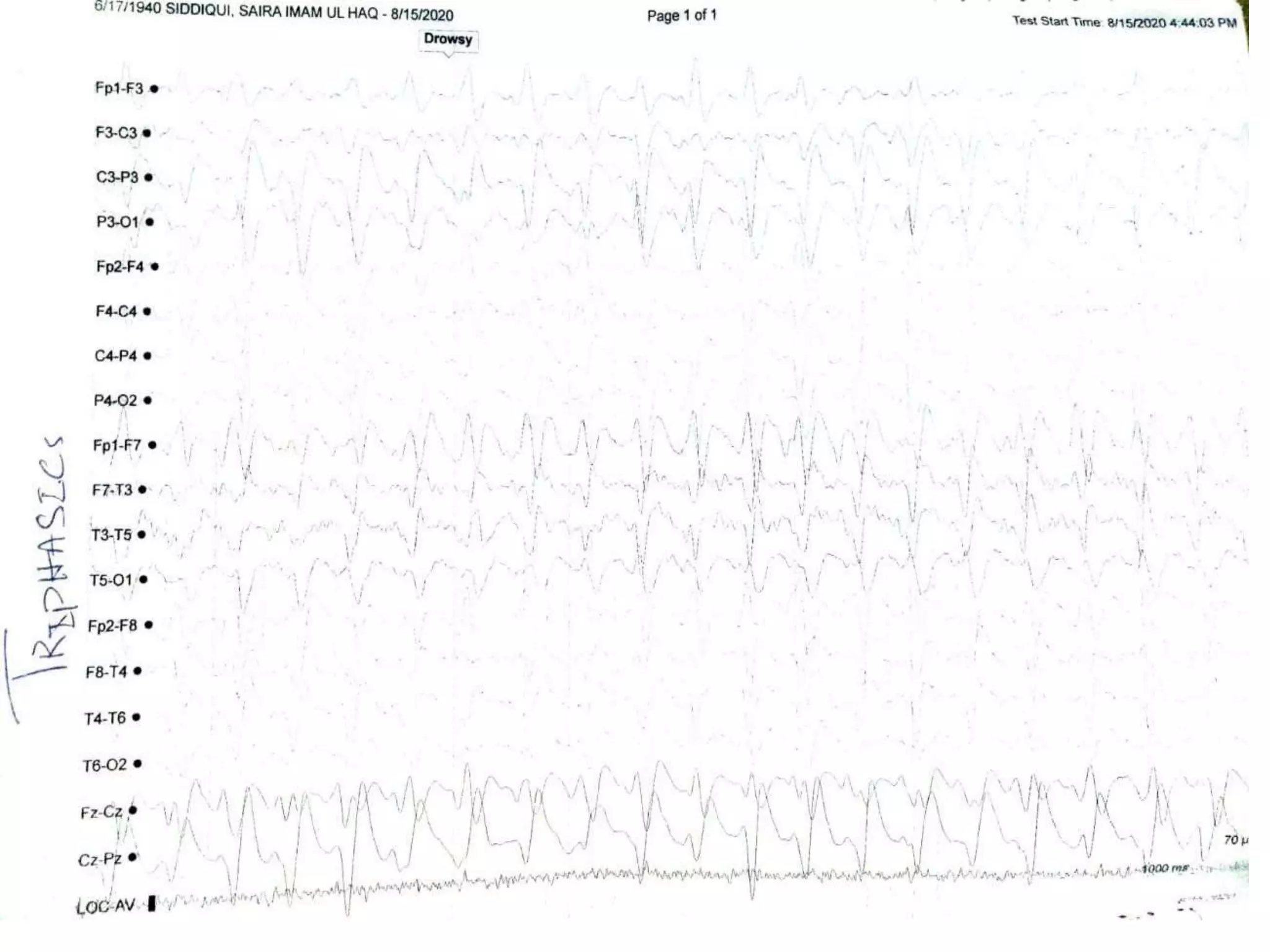
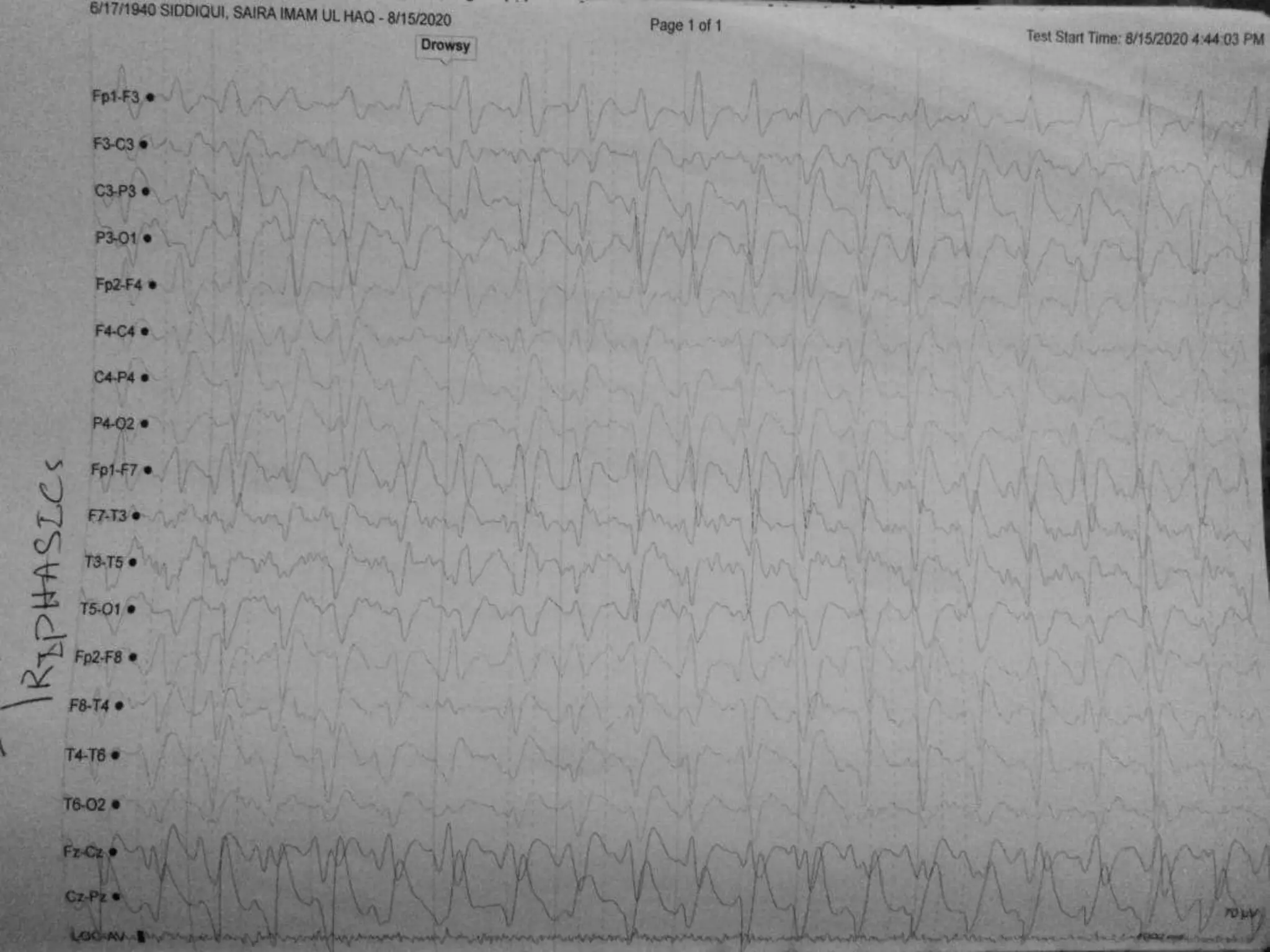
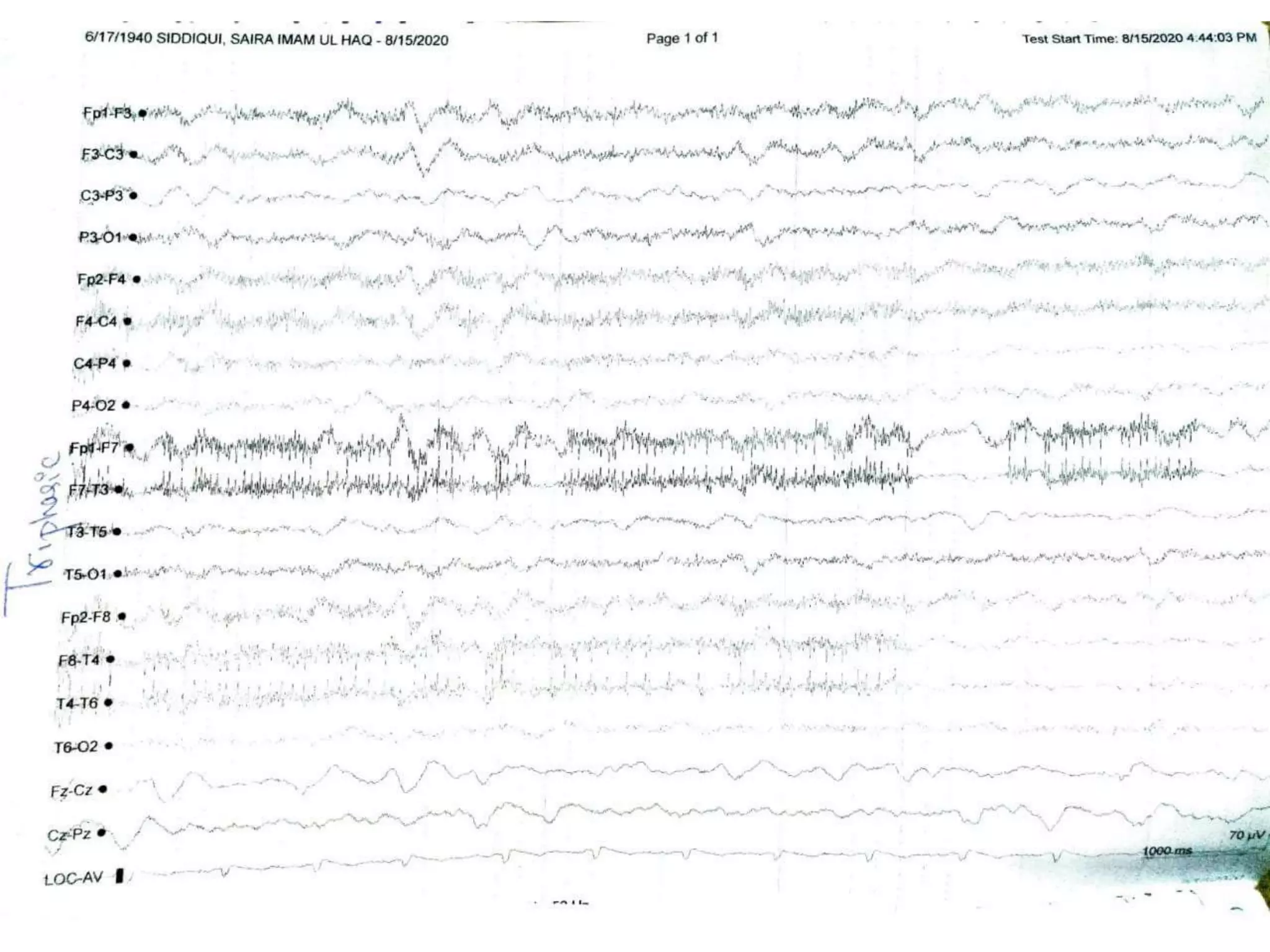
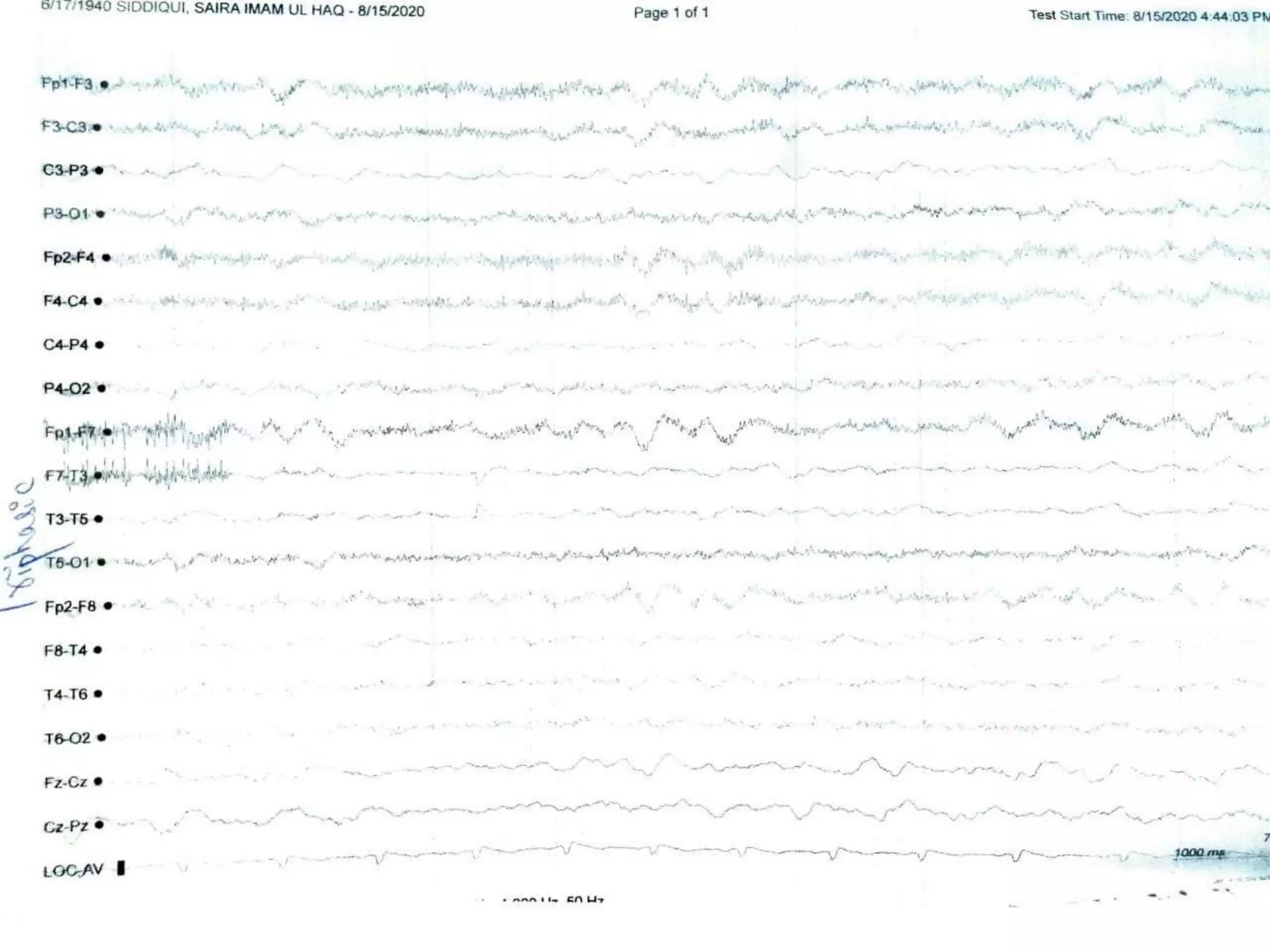
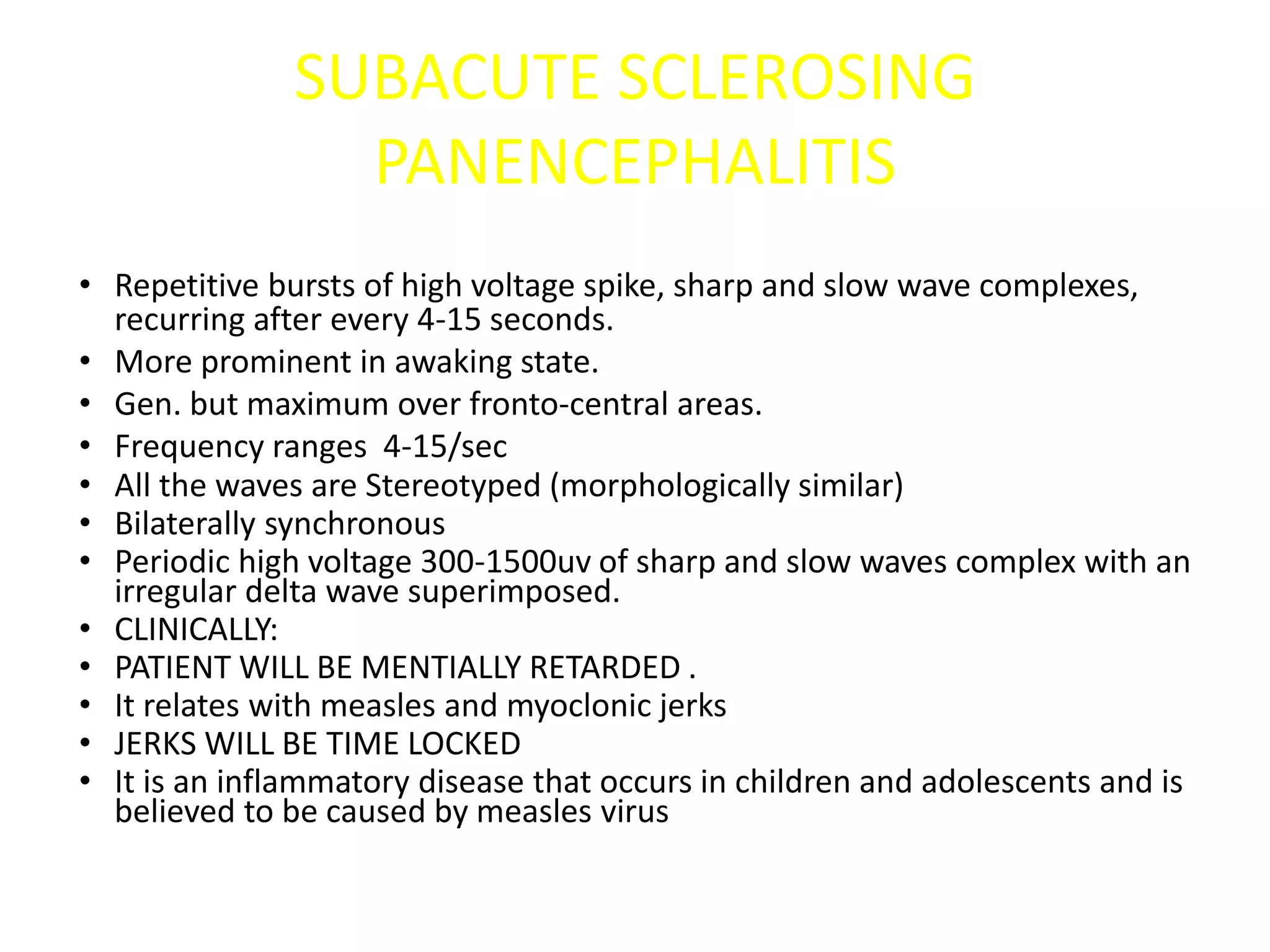
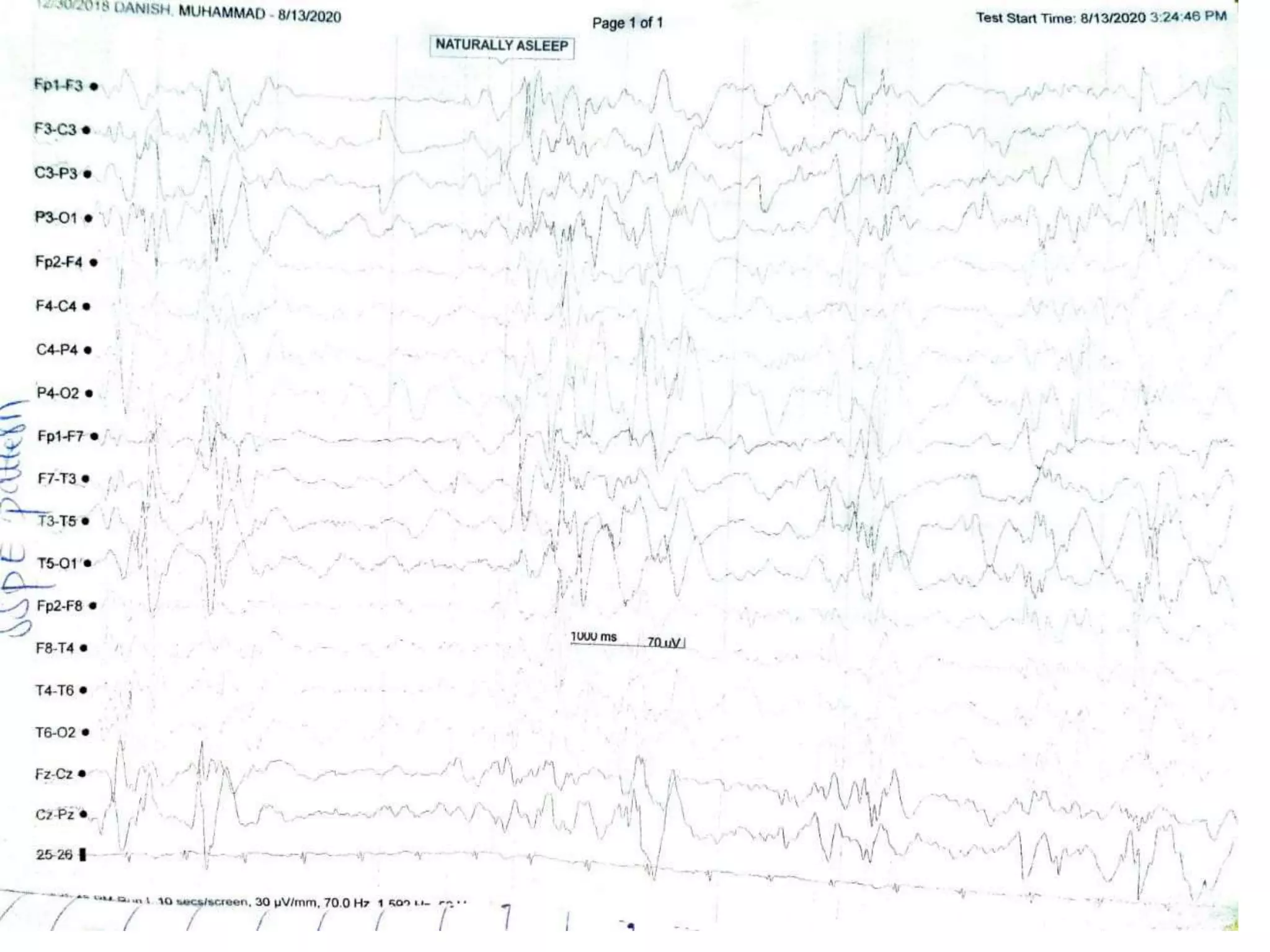
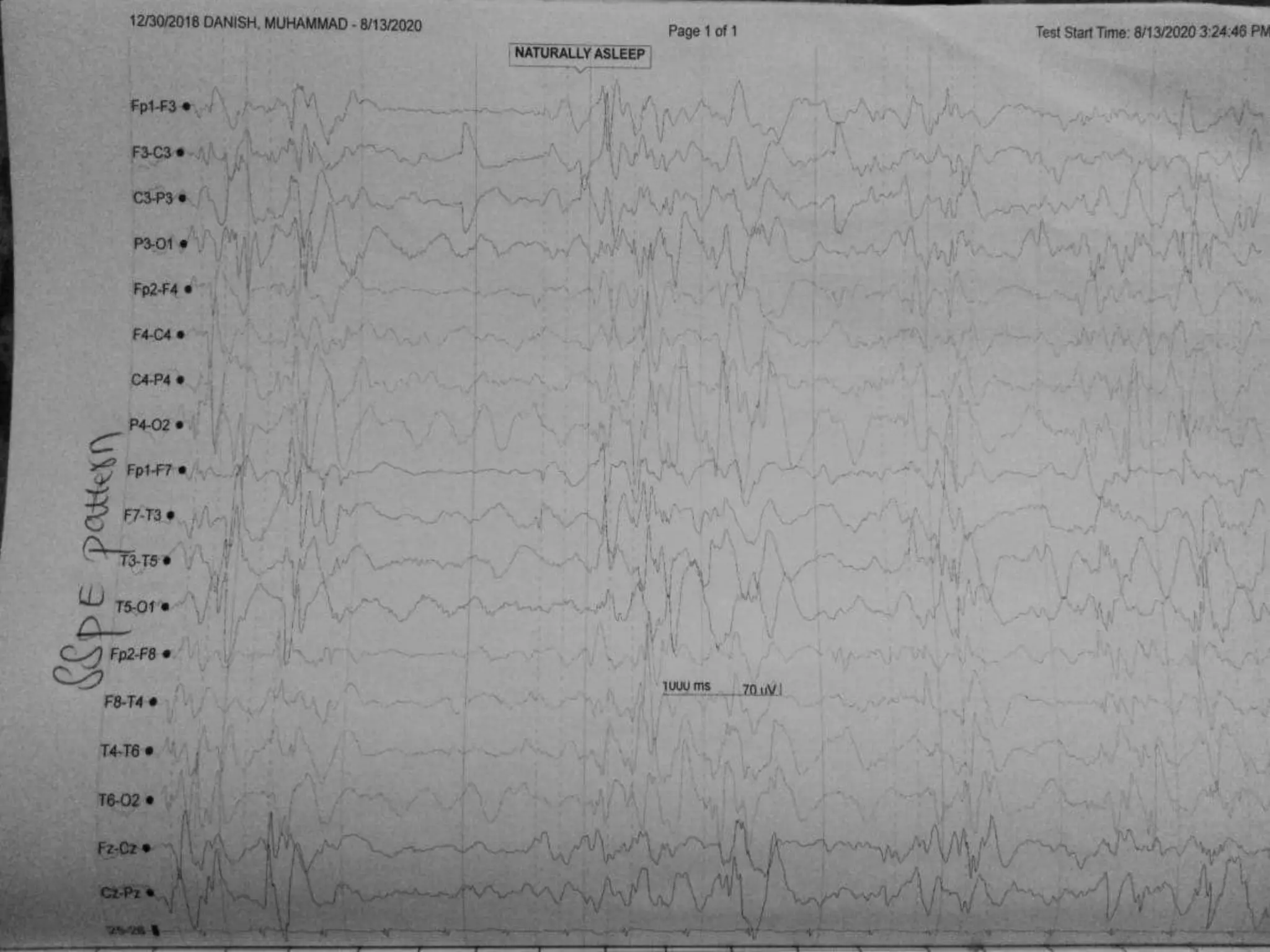
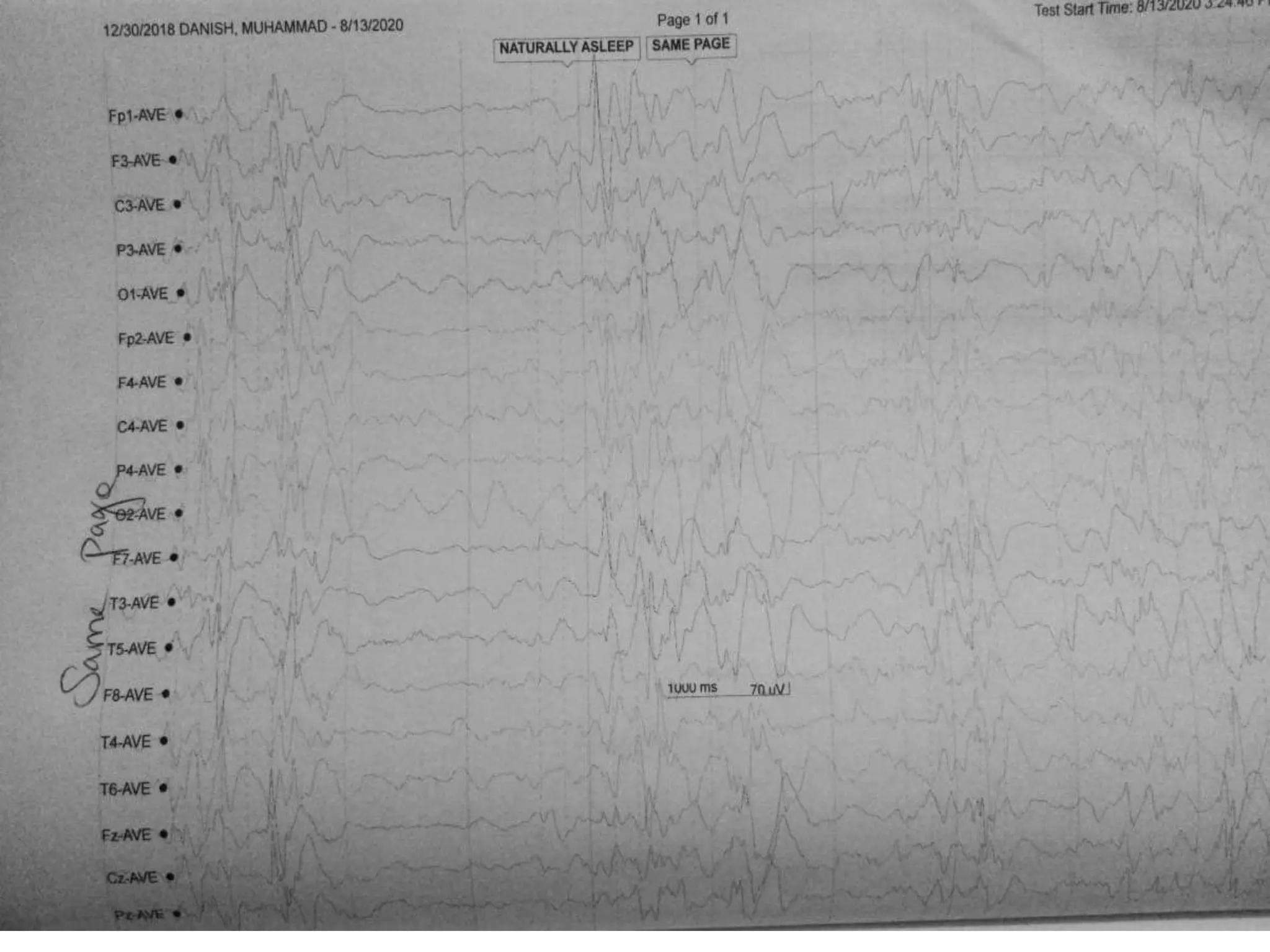
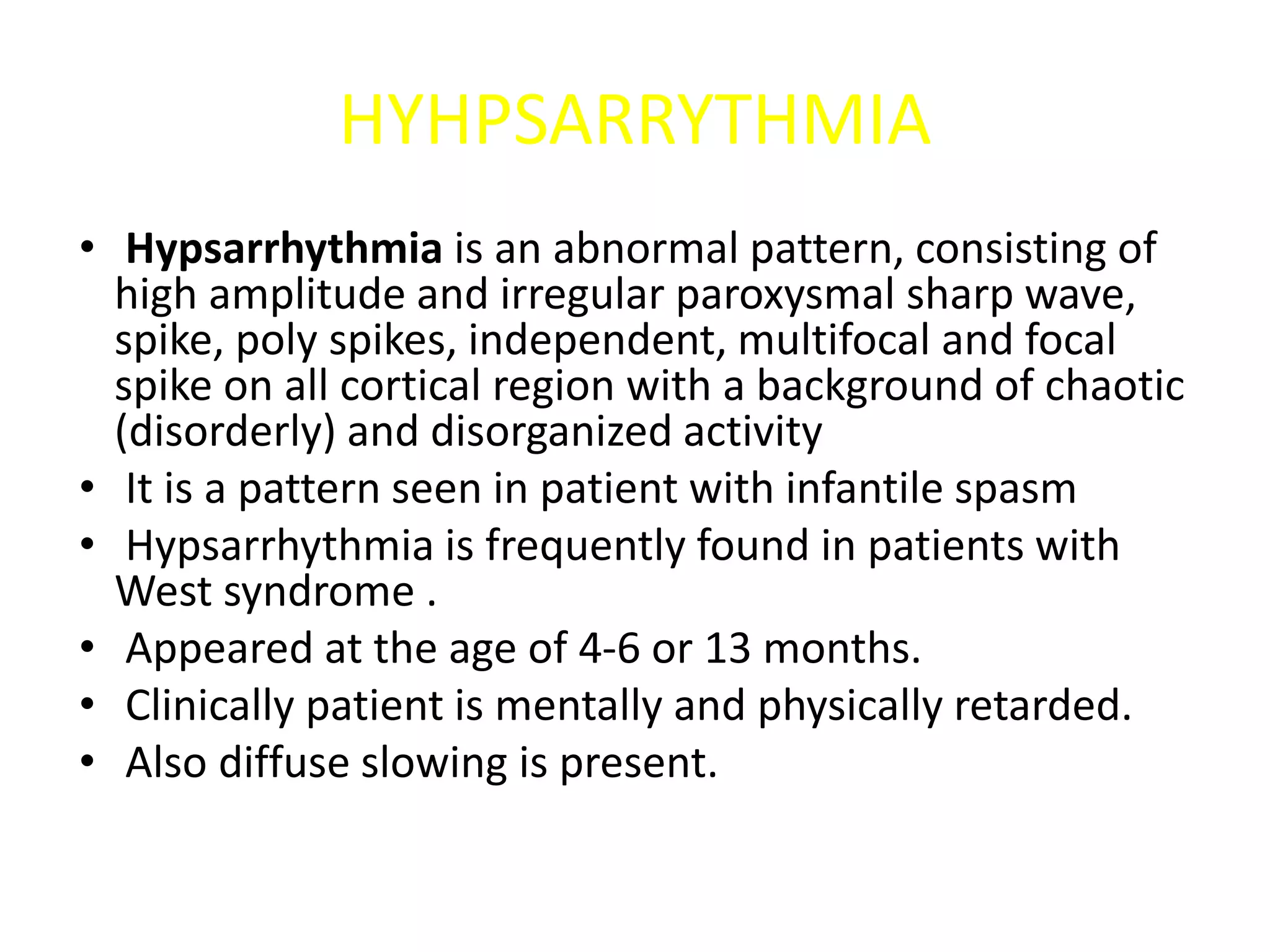
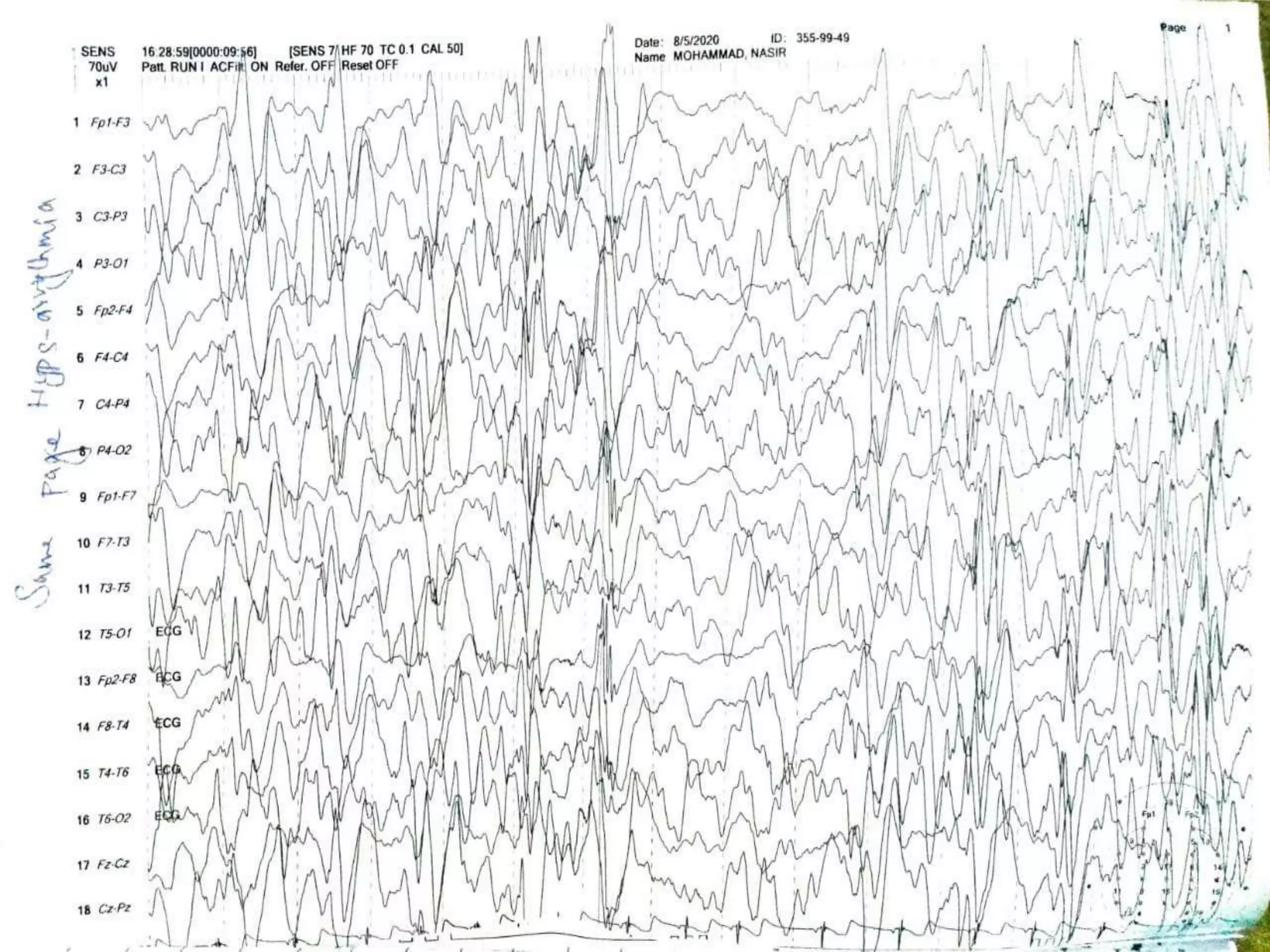
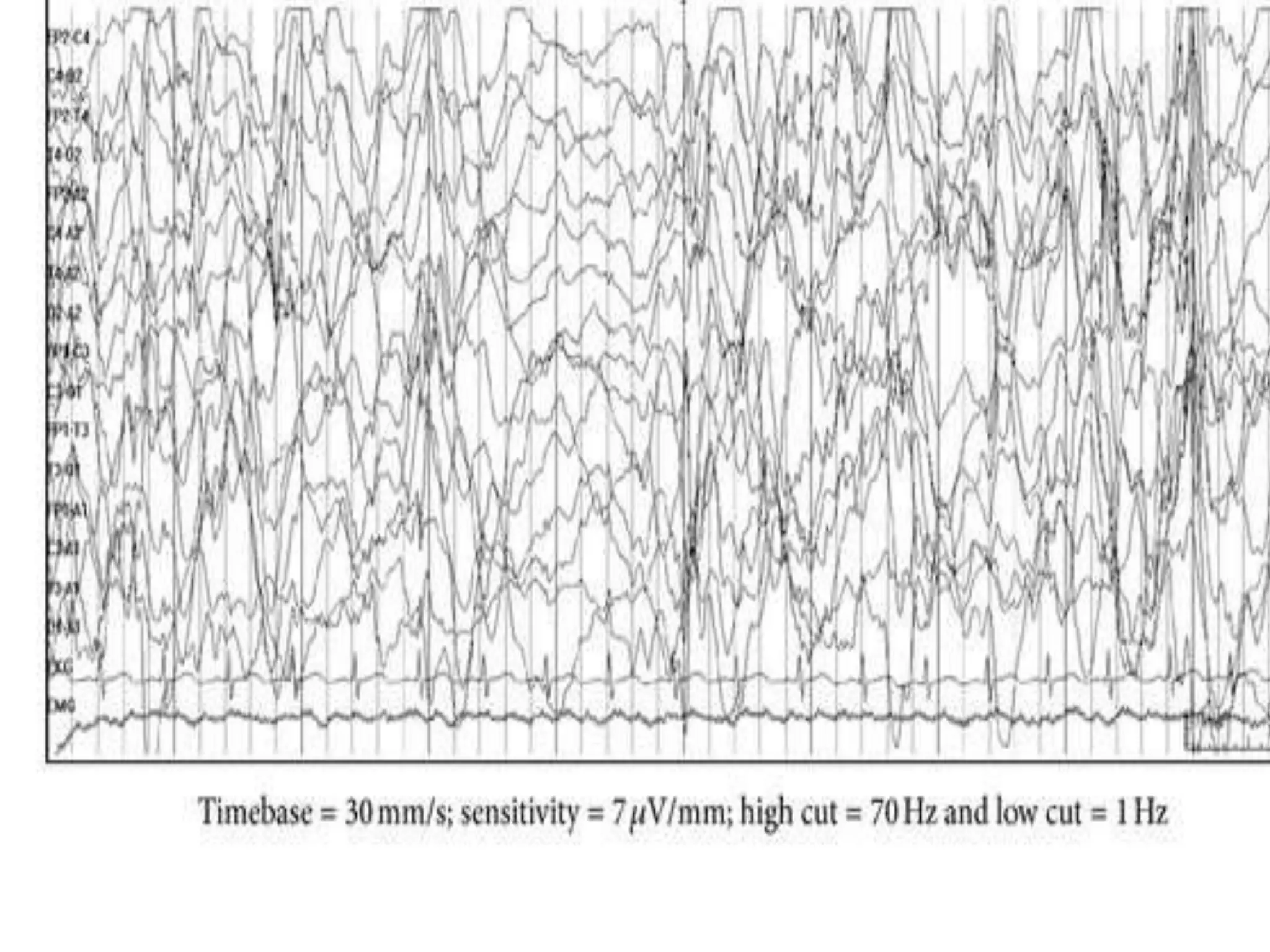
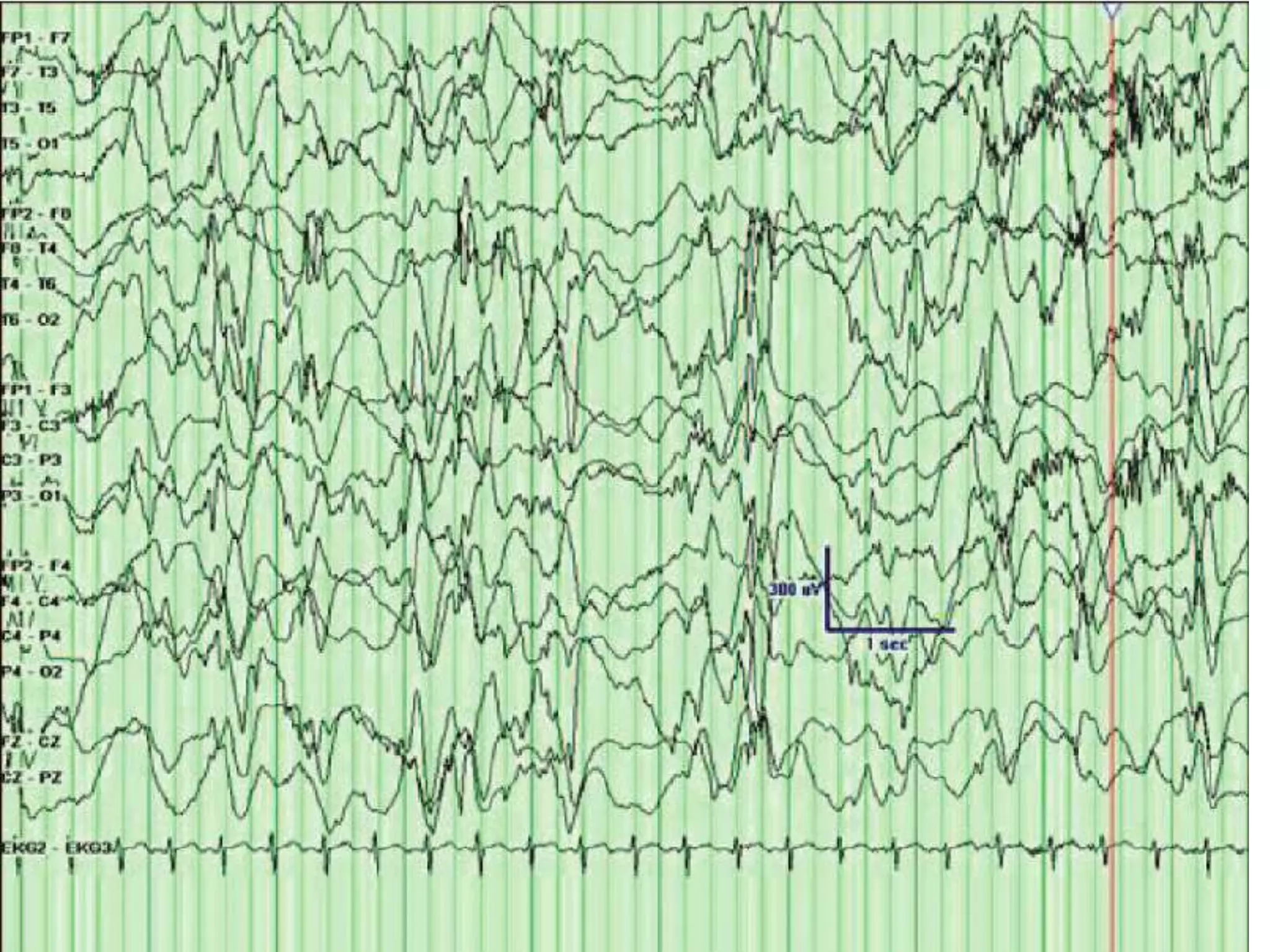
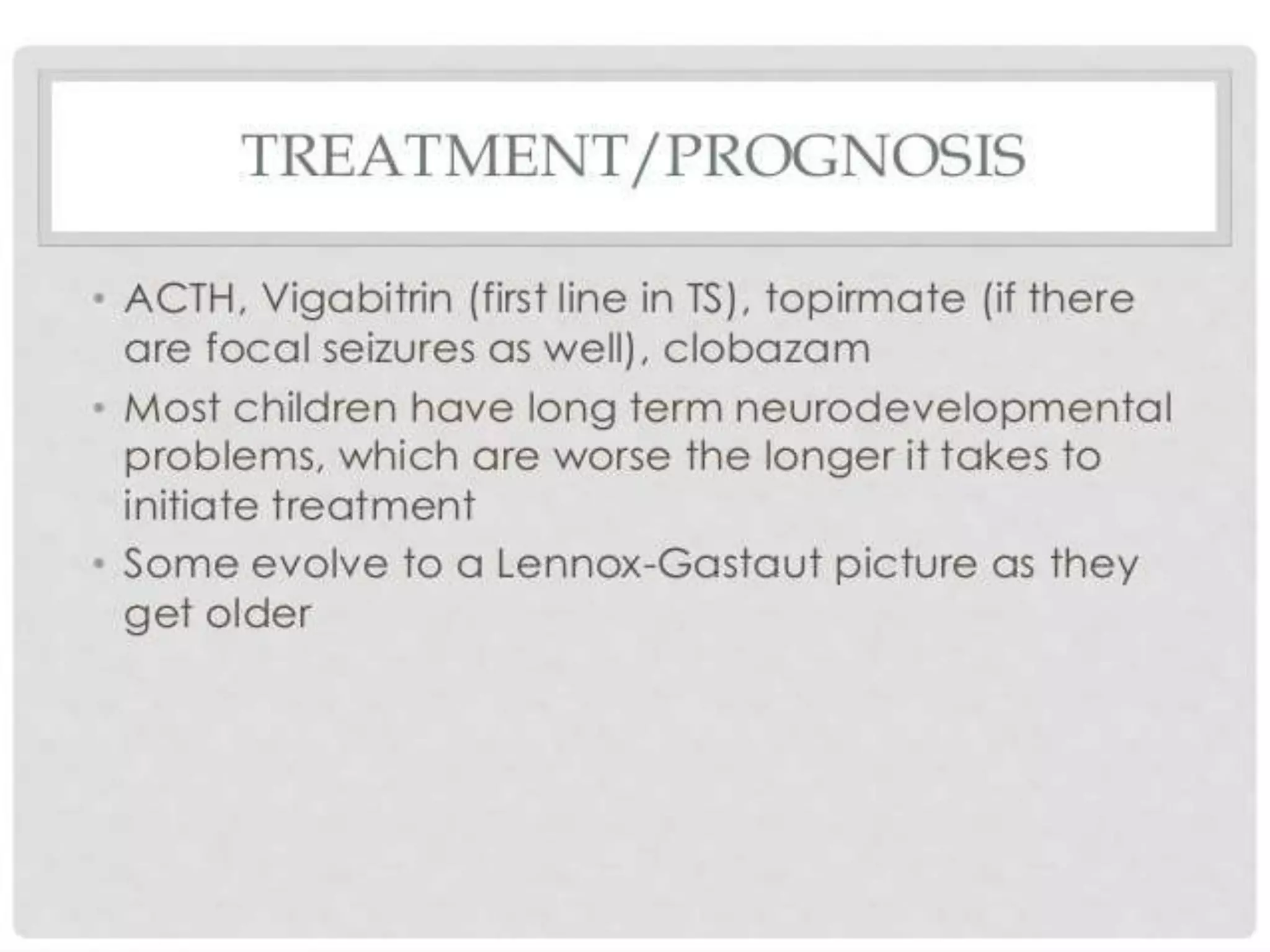
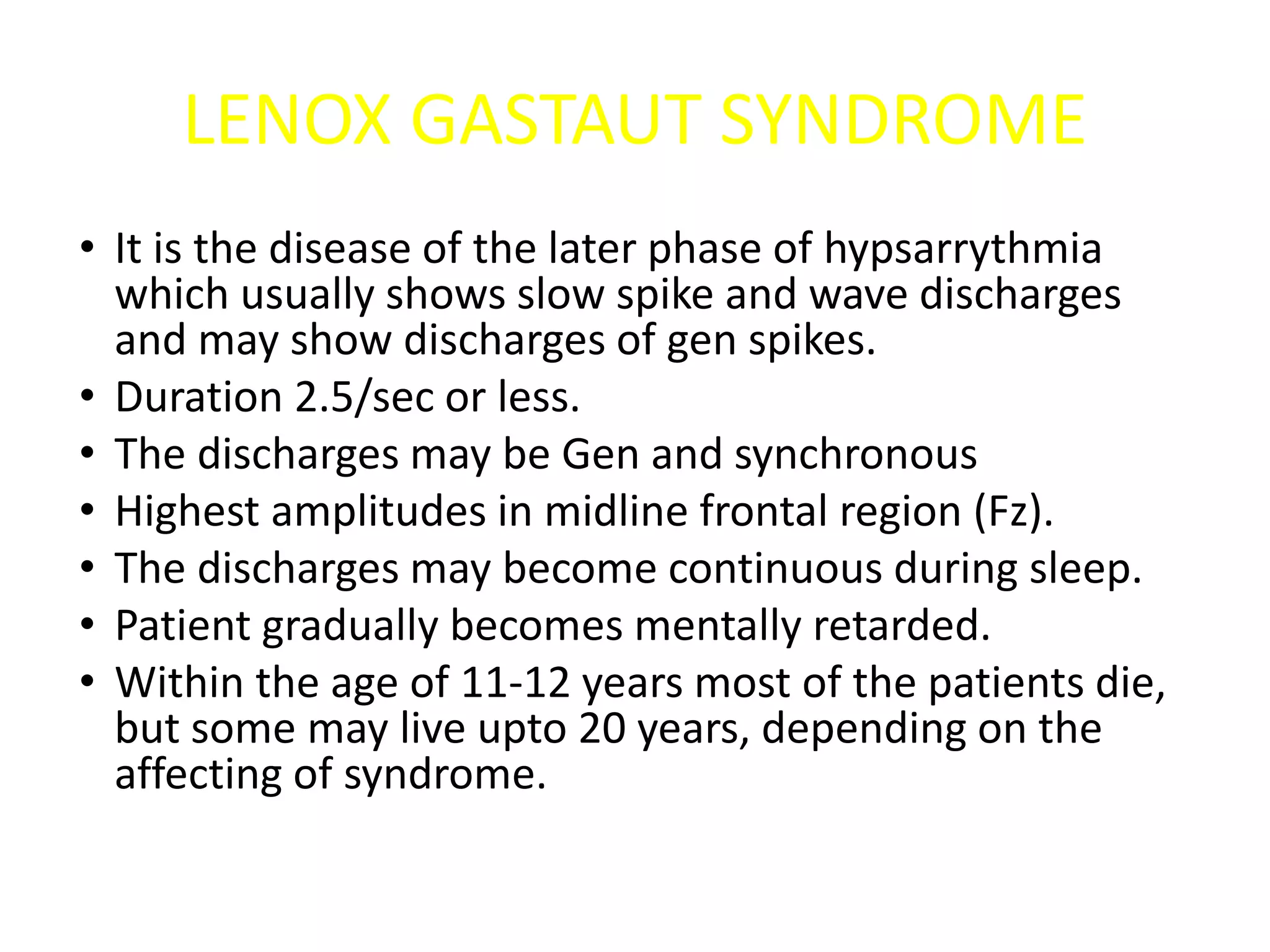
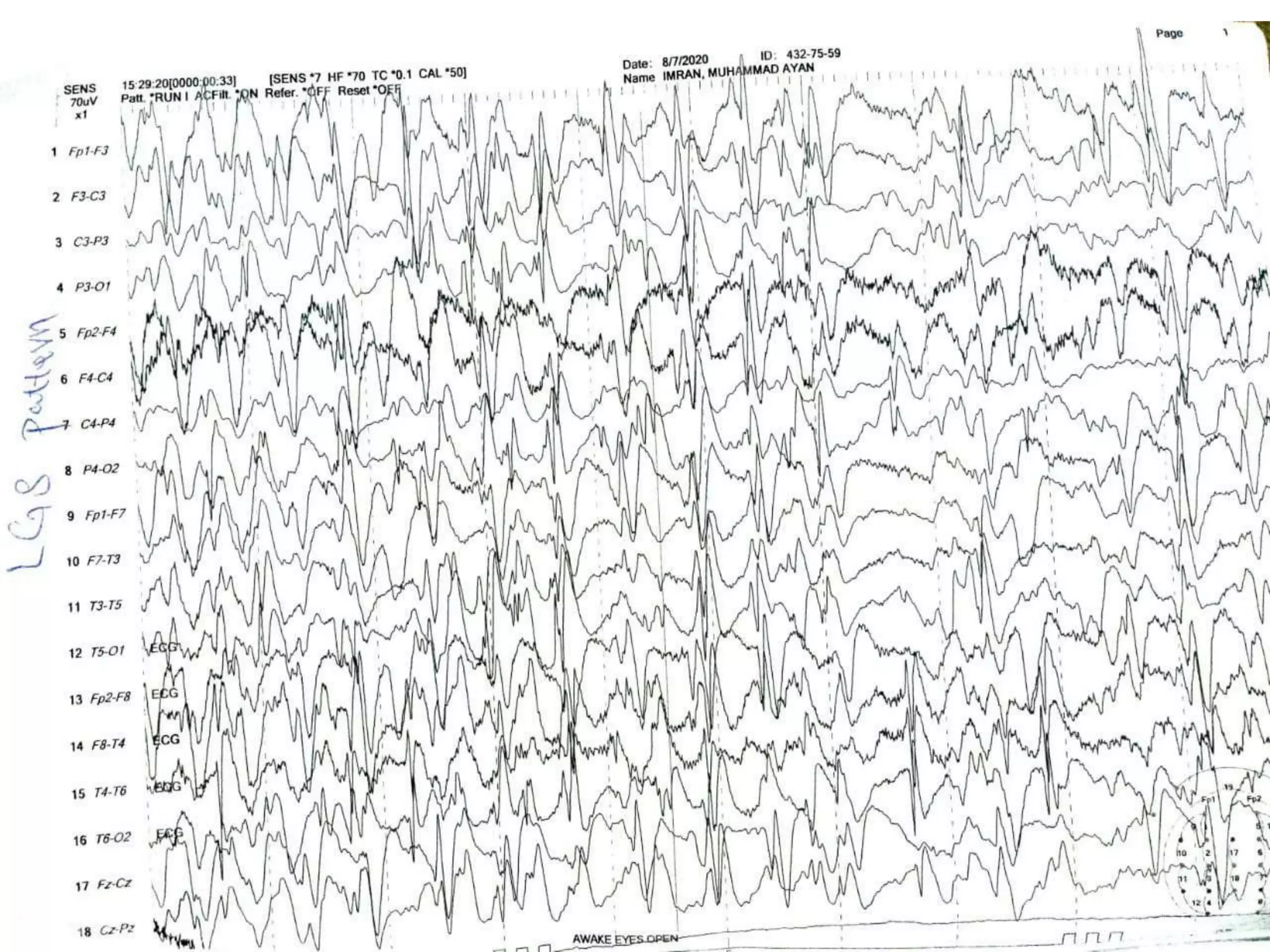
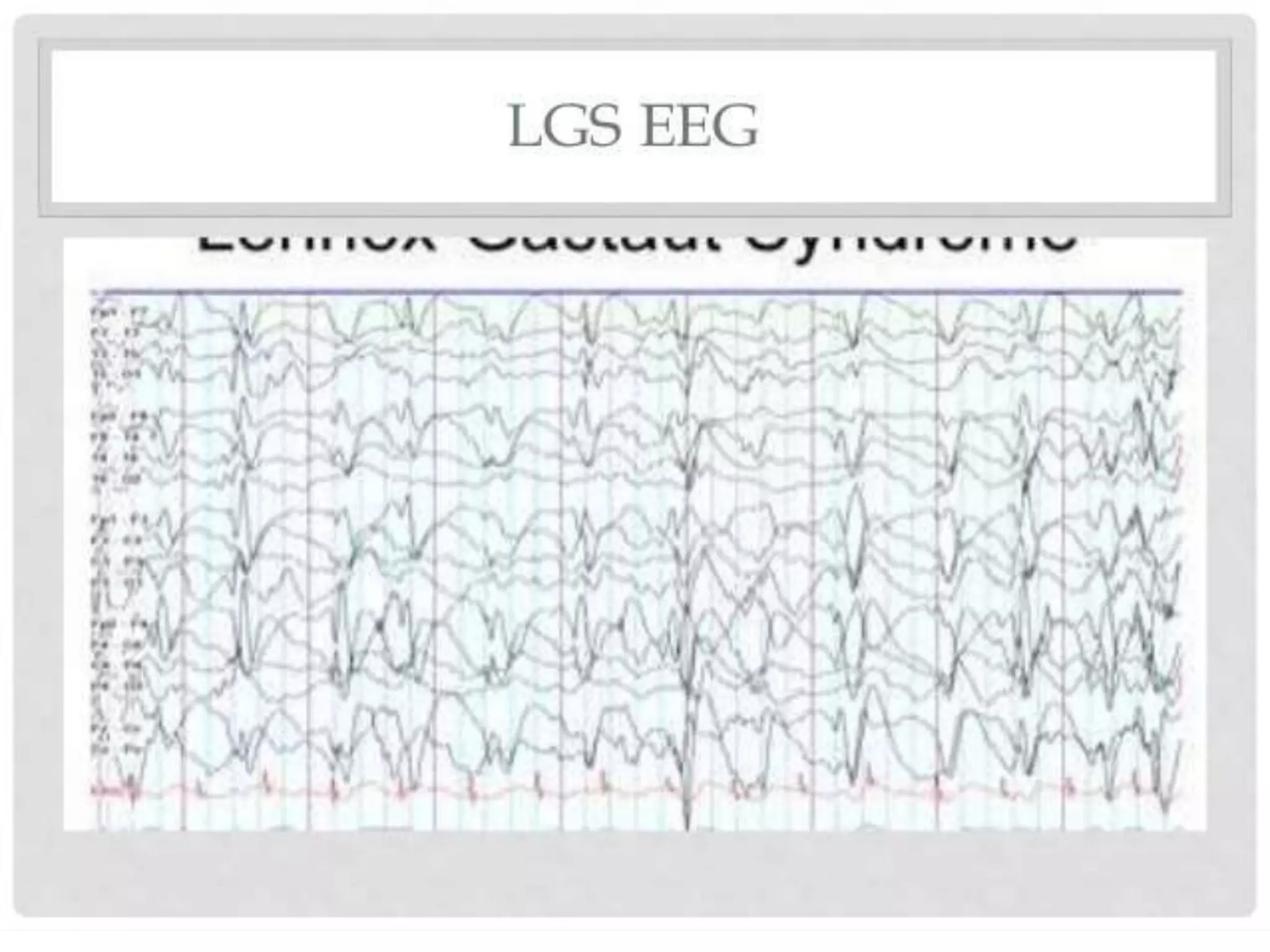
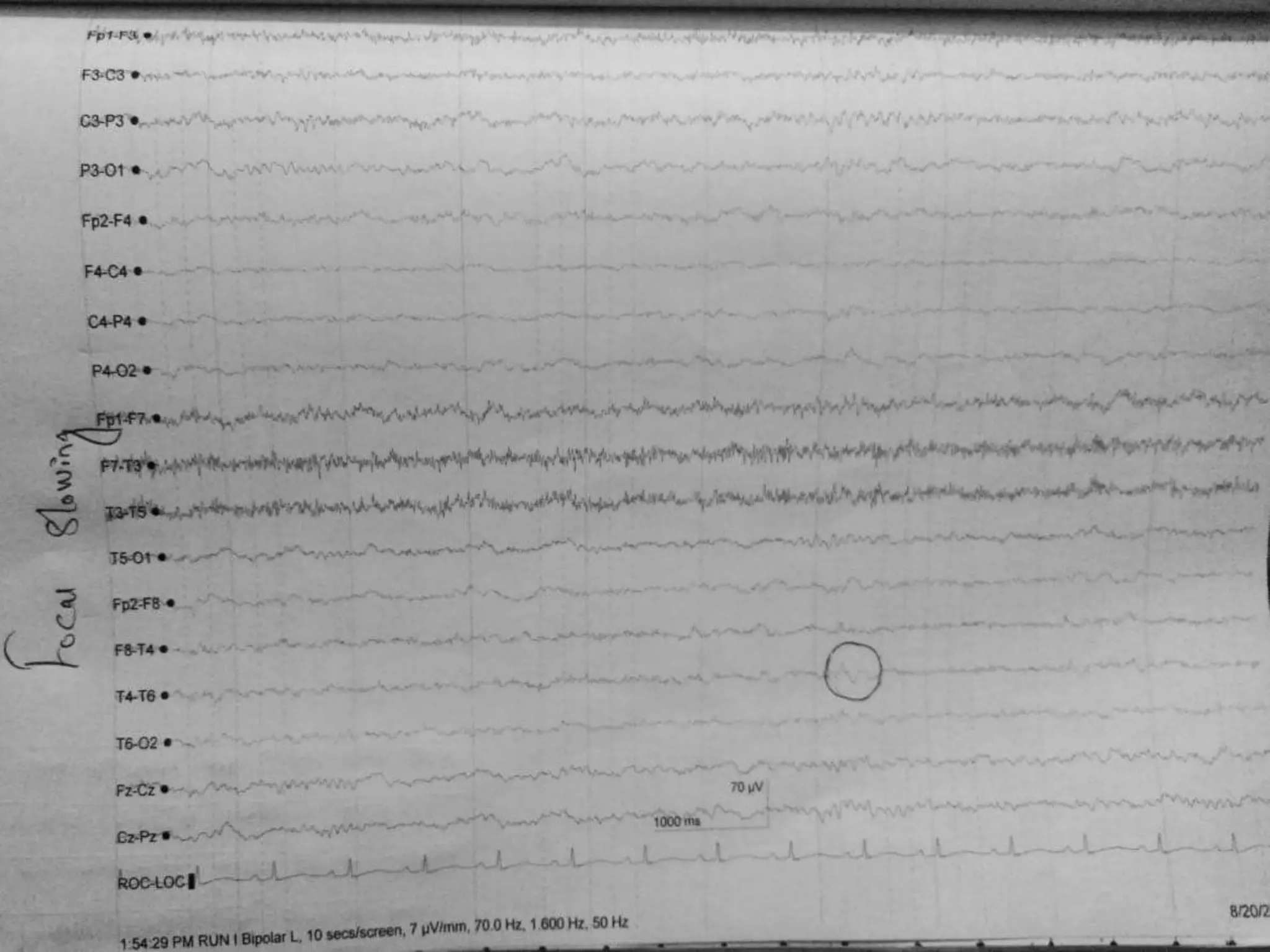
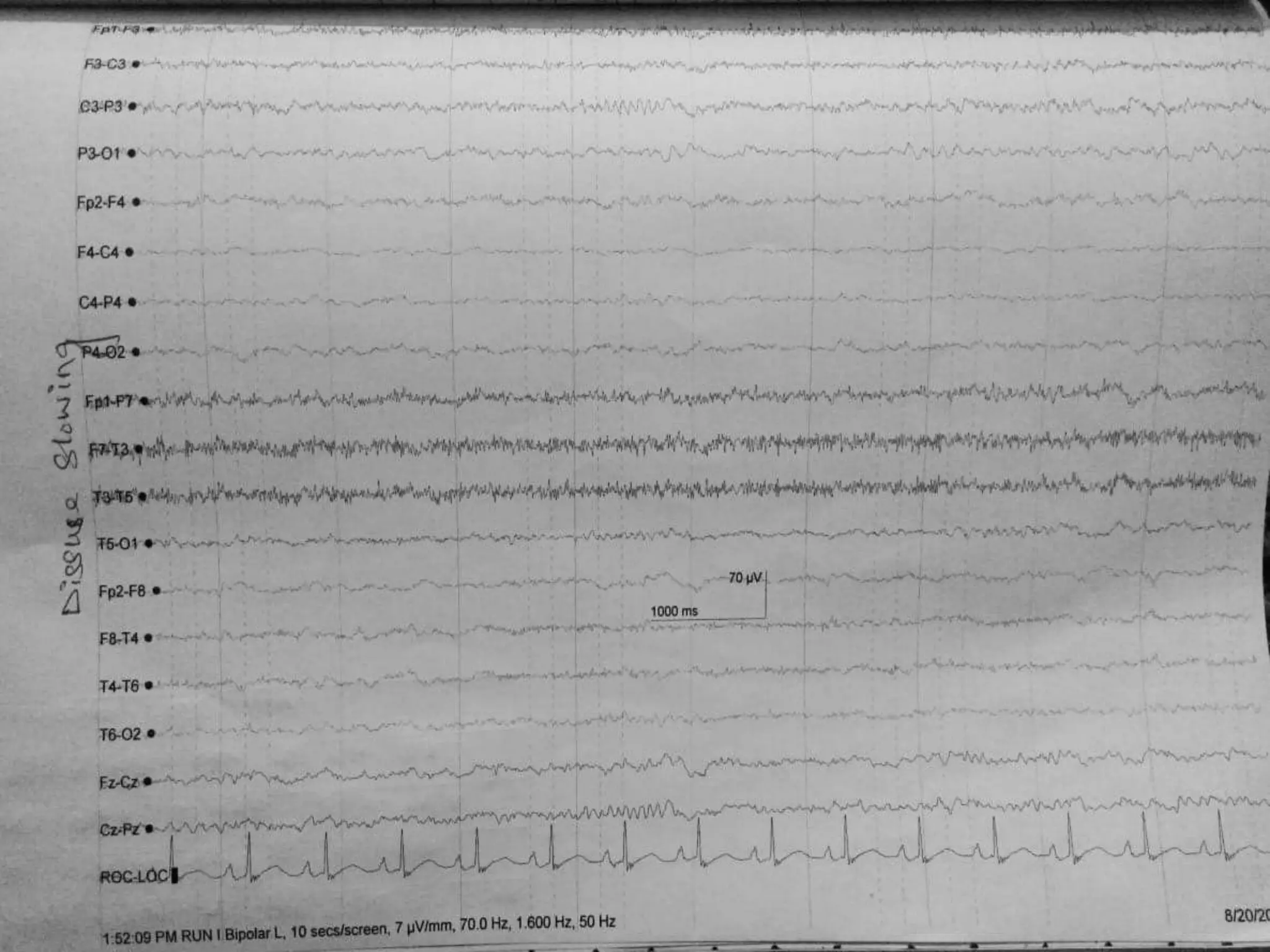
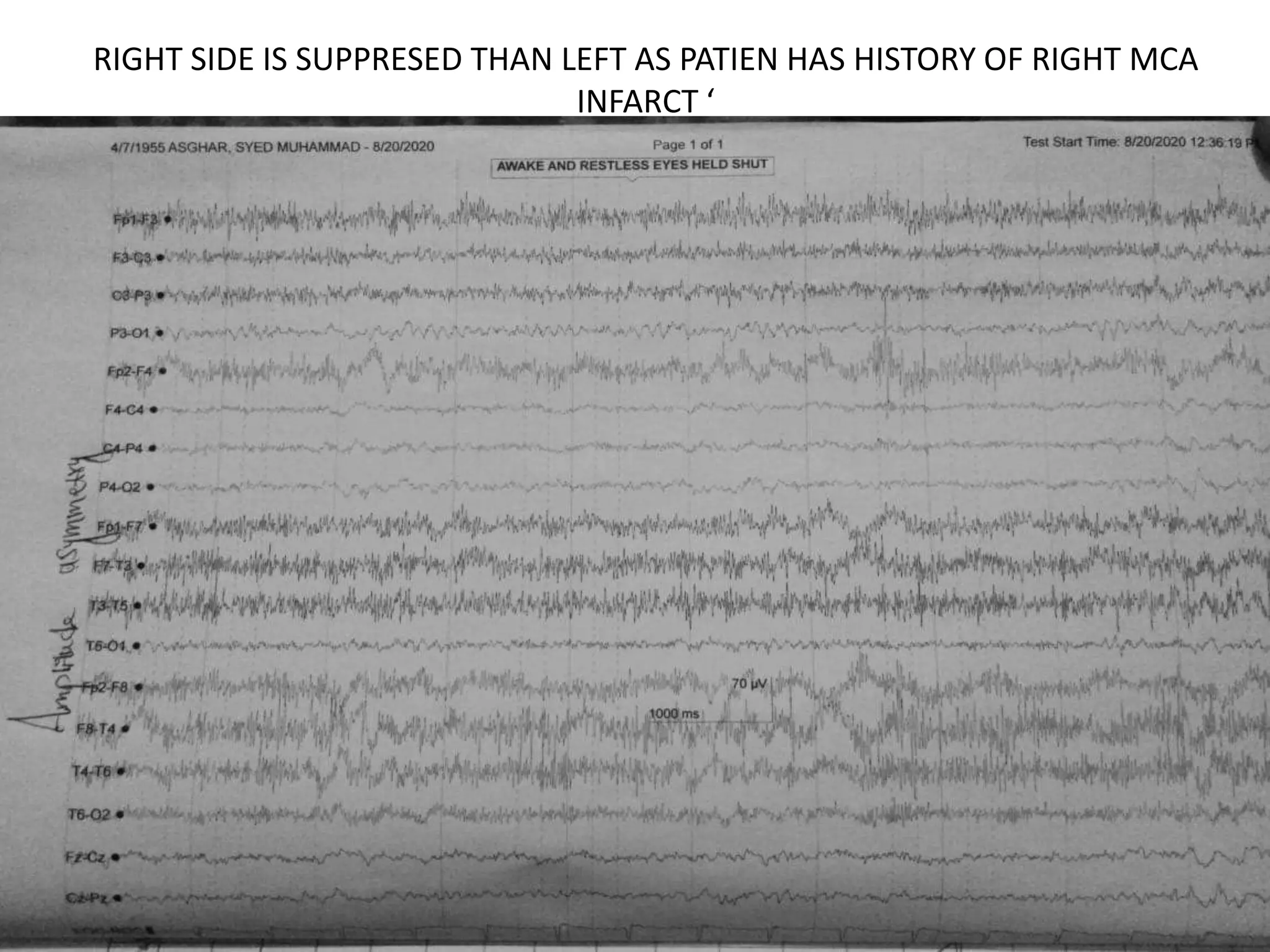
This document discusses various abnormal EEG patterns, including both epileptic and non-epileptic abnormalities. It provides details on specific epileptic patterns such as benign rolandic epilepsy, 3Hz spike and wave patterns indicative of absence seizures, periodic lateralized epileptiform discharges, and other conditions including Lennox Gastaut syndrome and Creutzfeldt-Jakob disease. It describes the characteristic EEG findings, clinical symptoms, age of onset and other factors for each of these abnormal patterns.