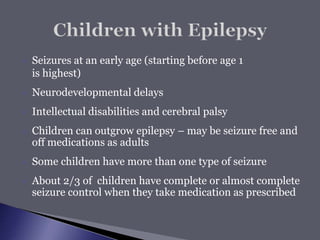
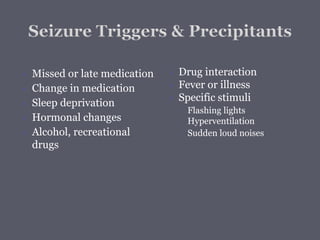
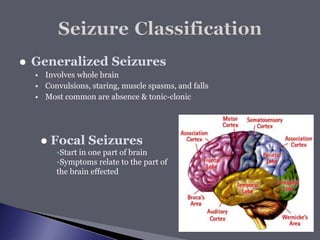
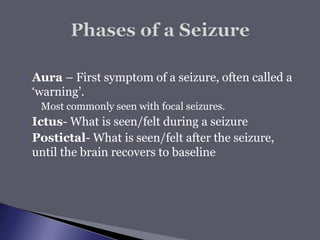
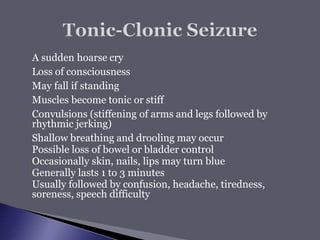
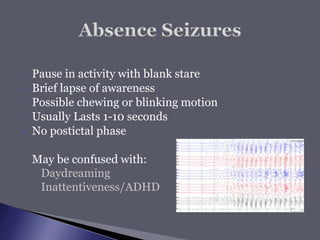
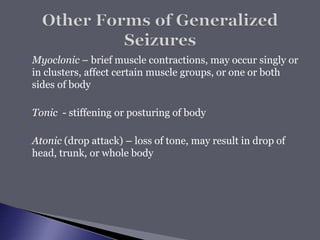
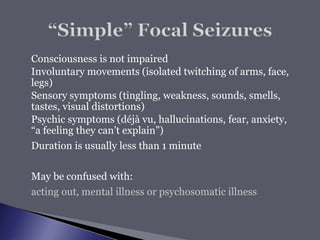
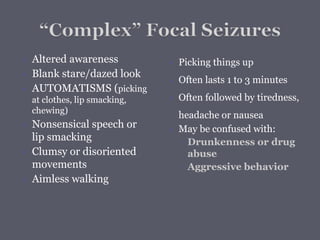
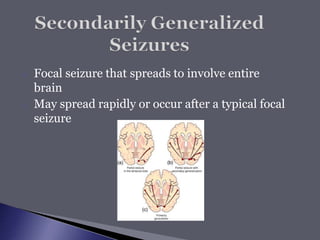
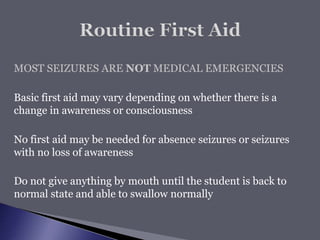
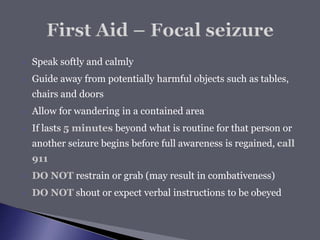
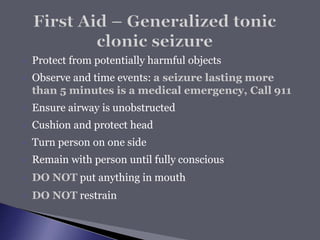
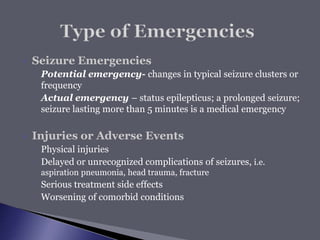
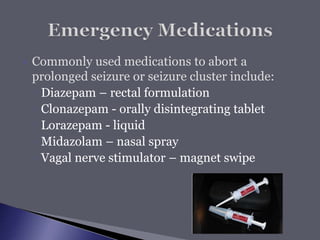
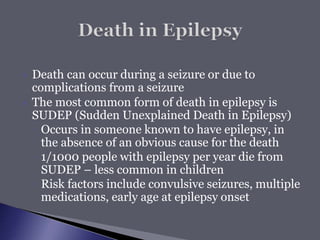
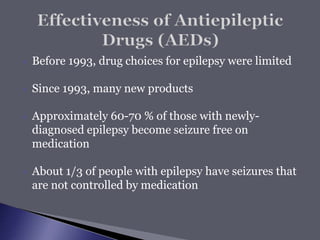
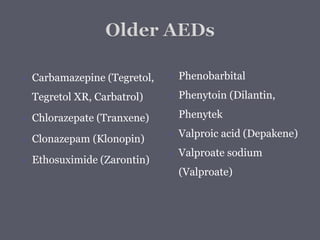
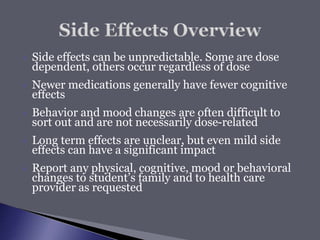
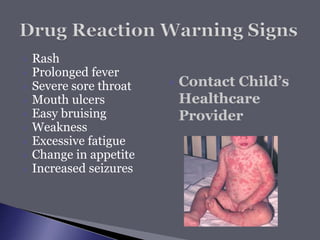
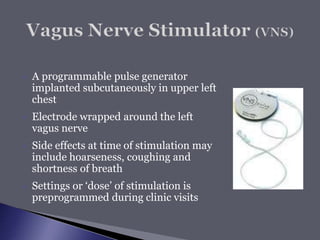
This document provides information about epilepsy and seizures. It defines epilepsy as a brain disorder characterized by recurrent, unprovoked seizures. It discusses the prevalence of epilepsy, common causes, seizure types including generalized and focal seizures, seizure emergencies, treatment options such as medications, surgery, diets and vagus nerve stimulators, and potential risks and side effects of seizures and treatments. The document is an educational guide covering many aspects of living with and managing epilepsy.