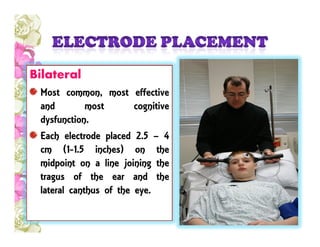
ECT, also known as electroconvulsive therapy, is a psychiatric treatment where seizures are electrically induced in anesthetized patients for therapeutic effects. It was first introduced in 1938 and has been established for treating severe depression, bipolar disorder, schizophrenia, and other conditions when other treatments have failed. The document discusses the procedure of ECT, including electrode placement, electrical dosage, risks and side effects like cognitive impairment and memory loss. It also covers indications, contraindications, the process before, during, and after treatment, and notes that some patients may undergo ECT against their will if deemed a risk to themselves or others.