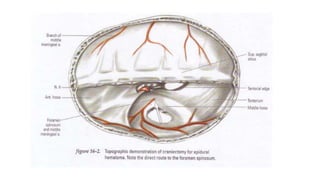
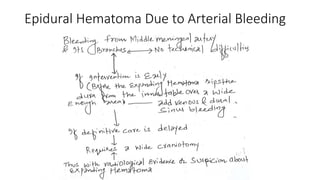
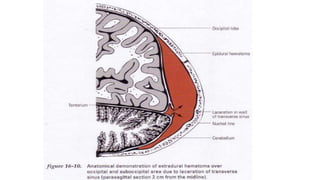
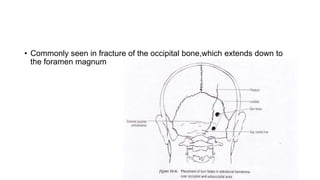
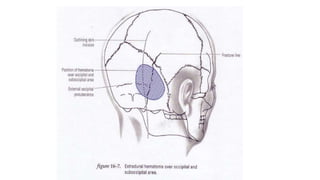
1. Epidural hematomas are usually caused by skull fractures that tear dural vessels, with bleeding accumulating in the epidural space. They account for 5-15% of fatal head injuries.
2. Clinical presentation varies from unconsciousness to brief coma to no loss of consciousness. Urgent surgical evacuation is indicated for hematomas over 30cc, midline shift over 5mm, or thickness over 15mm.
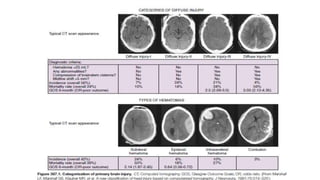
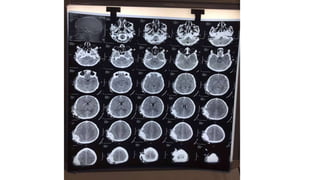
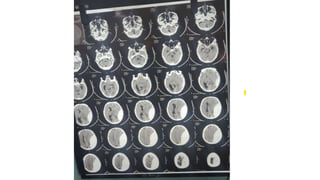
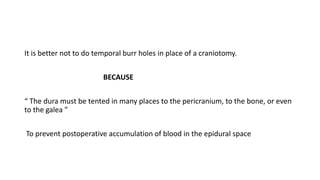
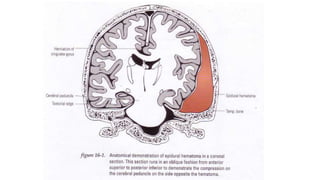
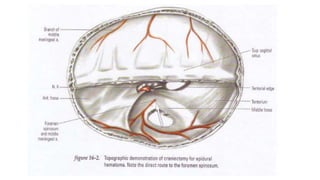
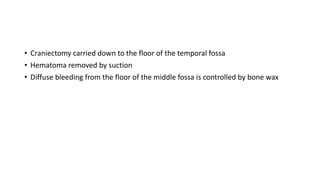
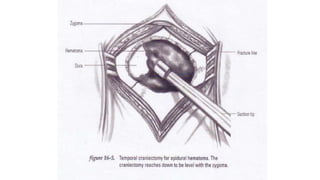
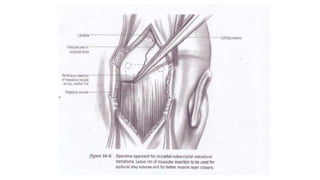
3. On CT scans, epidural hematomas appear as biconvex hyperdense lesions that can progress from acute to chronic forms over time. Surgical techniques involve craniotomy for evacuation and hemostasis to prevent reaccumulation.
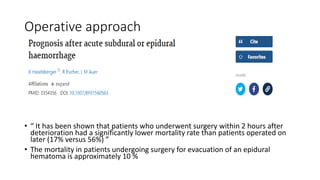
![• “ Reported incidences of epidural hematoma are a little more variable, ranging
from as low as 14% in a study by Paci and coworkers to 35% as reported by
Parzhuber and associates ”
• Paci GM, Sise MJ, Sise CB, et al. Preemptive craniectomy with craniotomy: what role in the
management of severe traumatic brain injury? J Trauma. 2009;67:531–536.
• 53. Parzhuber A, Wiedemann E, Richter-Turtur M, et al. [The contribution of the general and
trauma surgeon in neurotraumatology: experiences and results of 10 years]. Unfallchirurg.](https://image.slidesharecdn.com/epiduralhematoma-230407070652-3dafd26b/85/EPIDURAL-HEMATOMA-2-320.jpg)