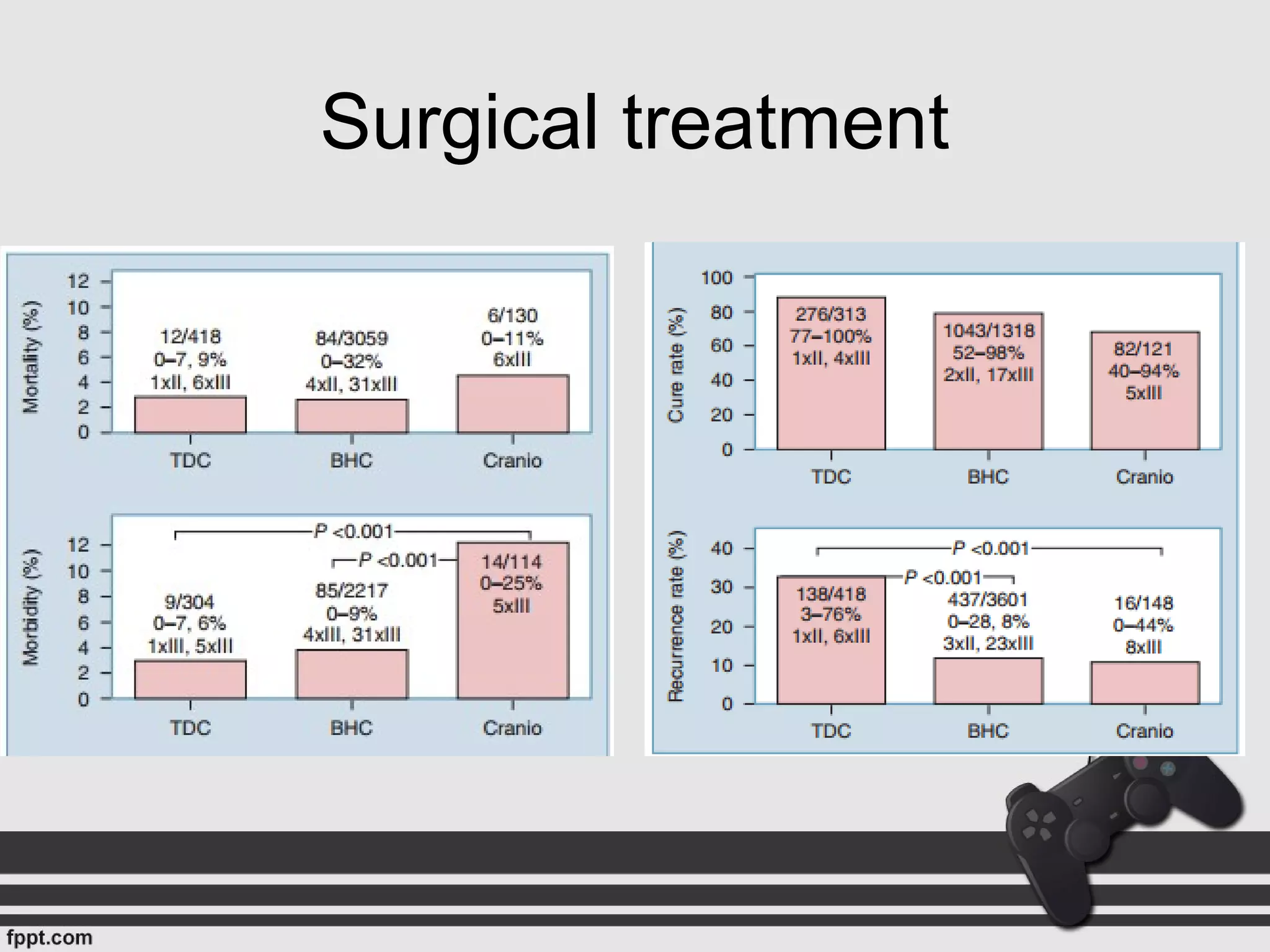
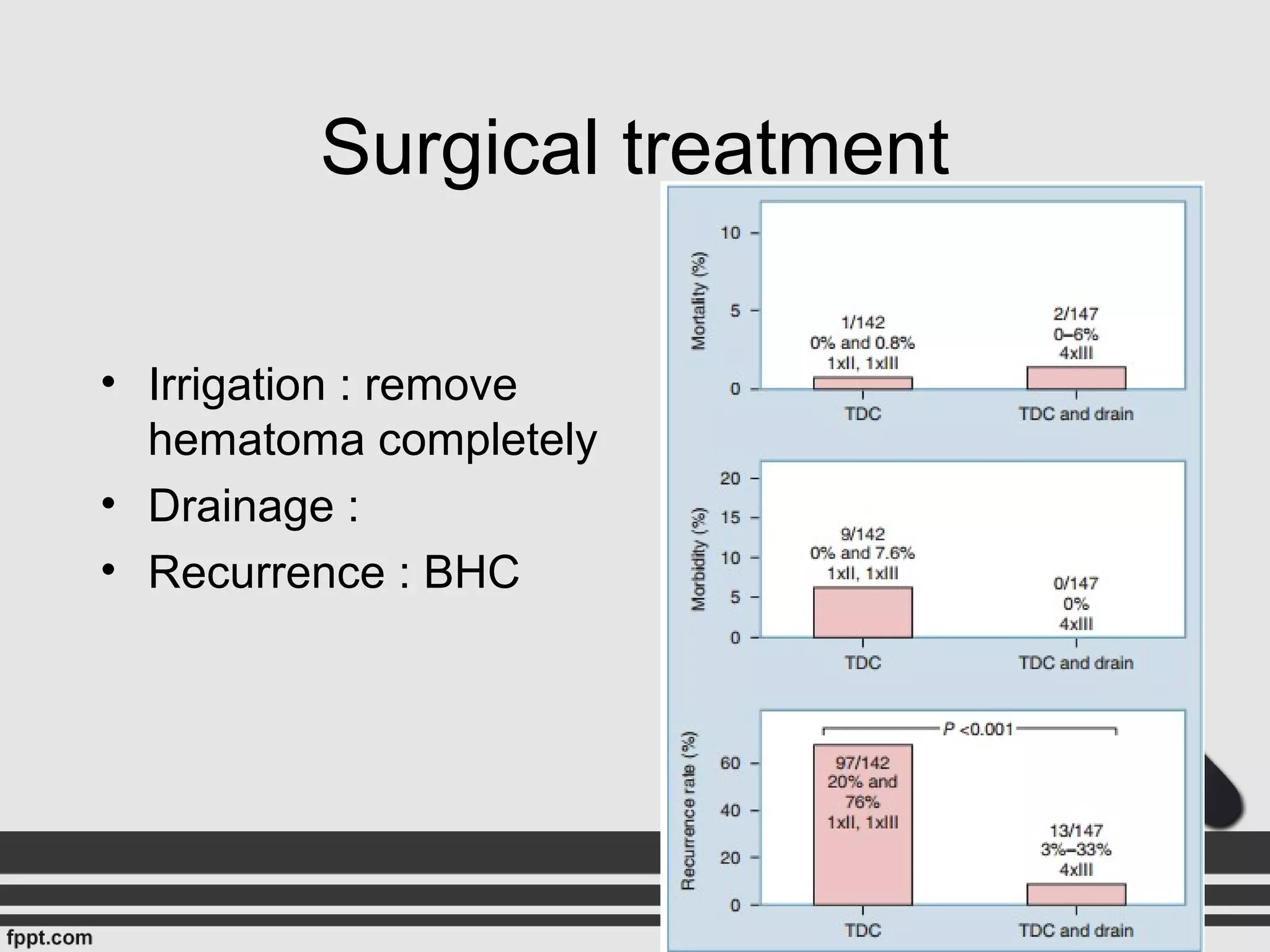
Subdural hematomas develop due to an osmotic gradient that increases protein content and oncotic pressure in the hematoma fluid. Microscopic examination shows fresh erythrocytes in CSDH fluid of any age. Neovasculature and abnormal dilated sinusoids in the outer CSDH membrane allow leakage of plasma and red blood cells into the hematoma cavity. Various surgical techniques are used to treat CSDHs including burr hole drainage, twist drill craniotomy, and craniotomy. Medical treatments like corticosteroids may help reduce recurrence by inhibiting neomembrane formation and inflammation. Postoperative care includes hydration and keeping patients flat to prevent recurrence in the first few days after