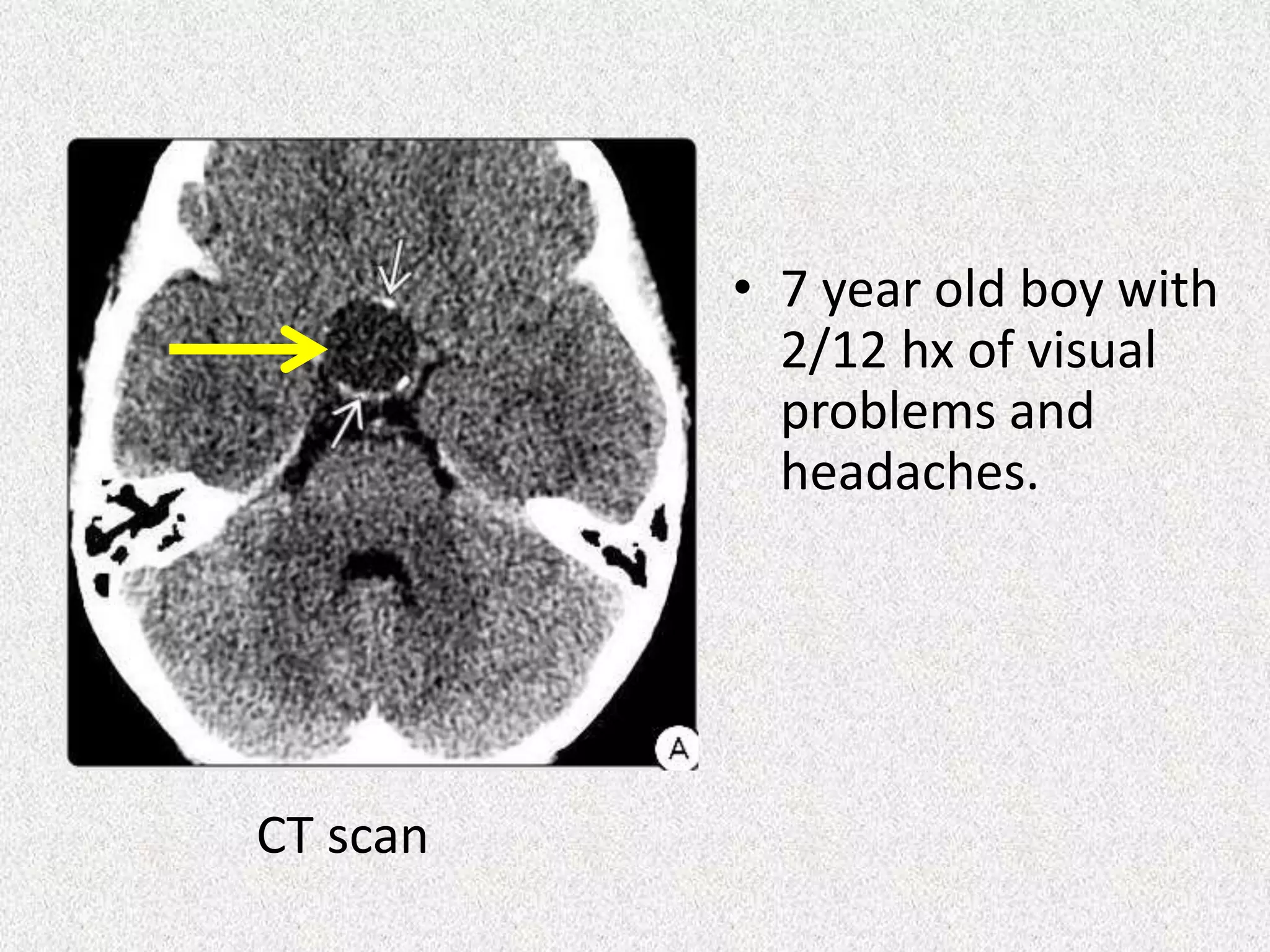
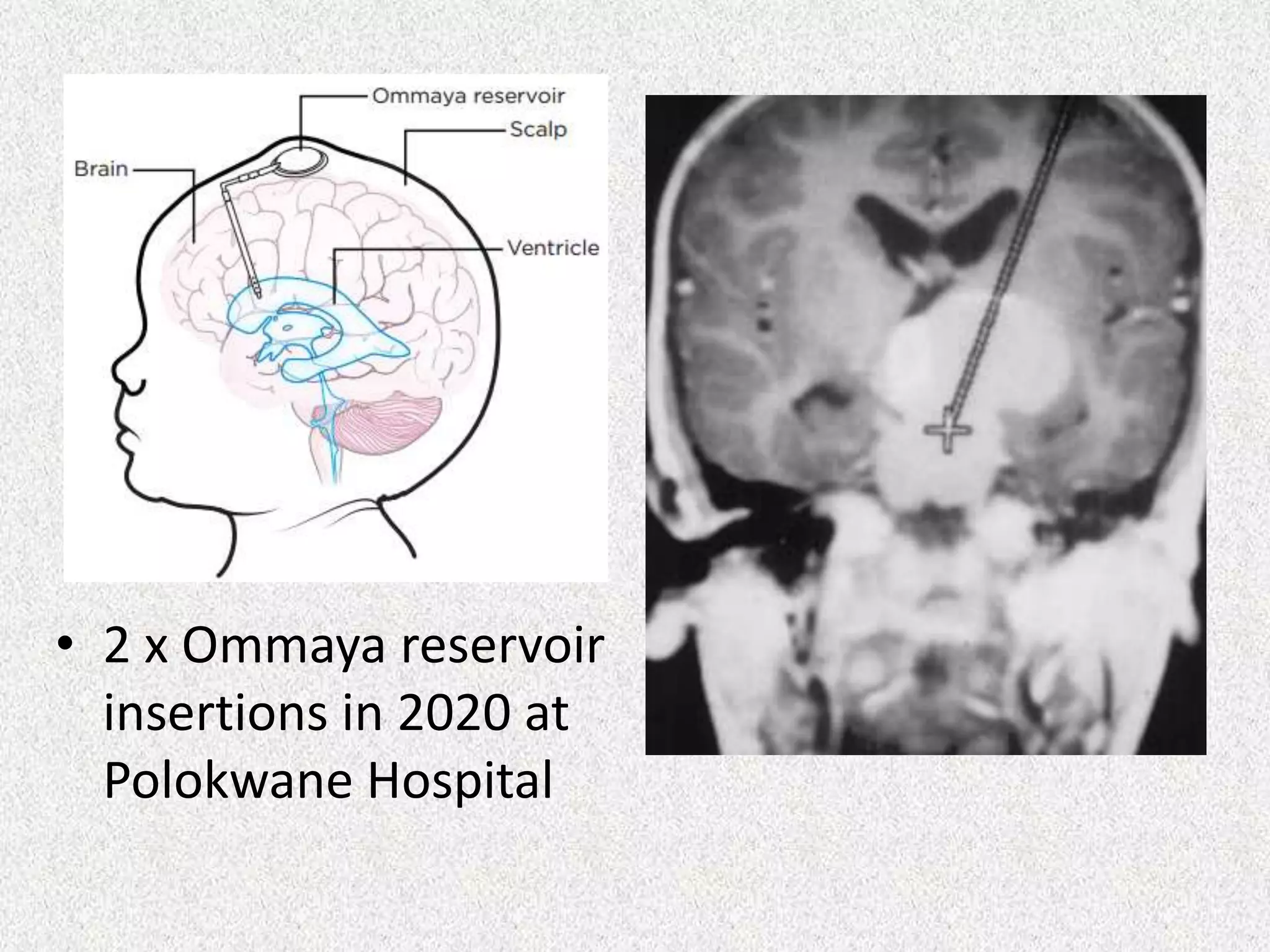
Craniopharyngioma is a benign but complex brain tumor that occurs near the pituitary gland. It can cause vision problems, hormone deficiencies, and other issues due to its location near critical structures. Treatment involves maximal safe surgical removal combined with radiation therapy or other adjuvant therapies. While surgery and radiation can control the tumor, long-term management of complications is challenging due to the effects on pituitary and hypothalamic function. Future treatments may involve targeted molecular therapies based on genetic mutations in some craniopharyngiomas.