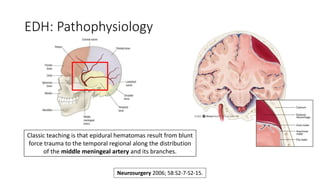
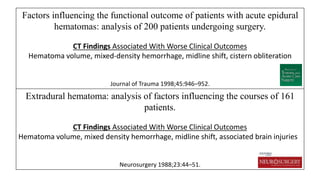
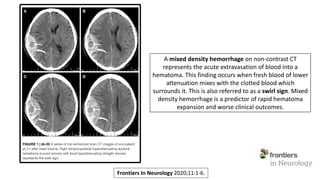
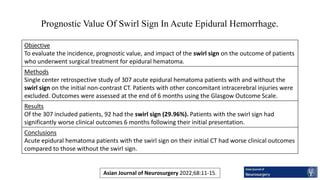
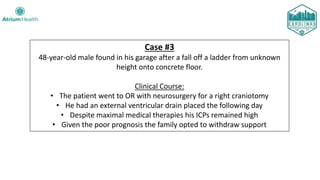
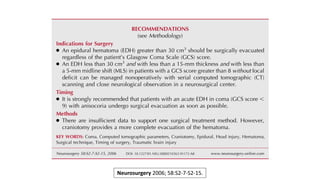
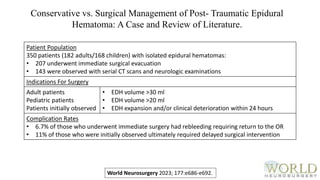
The document discusses acute epidural hematomas (EDH), highlighting case studies, pathophysiology, CT characteristics, and prognostic factors impacting patient outcomes. It emphasizes the significance of the 'swirl sign' on CT scans as an indicator of worse clinical outcomes and compares surgical vs. conservative management of EDH. Additionally, it presents statistical data on mortality and recovery outcomes based on Glasgow Coma Scale (GCS) scores and other factors affecting prognosis.

![Disclosures
This ongoing series is proudly sponsored by the Emergency Medicine and
Neurosurgery Residency Programs at Carolinas Medical Center.
The goal is to promote widespread mastery of imaging interpretation.
There is no personal health information [PHI] within, and all ages have
been changed to protect patient confidentiality.](https://image.slidesharecdn.com/edhpresentation-11-16-23-231118150529-51551e29/85/Neuroimaging-Mastery-Project-Presentation-4-Acute-Epidural-Hematomas-2-320.jpg)