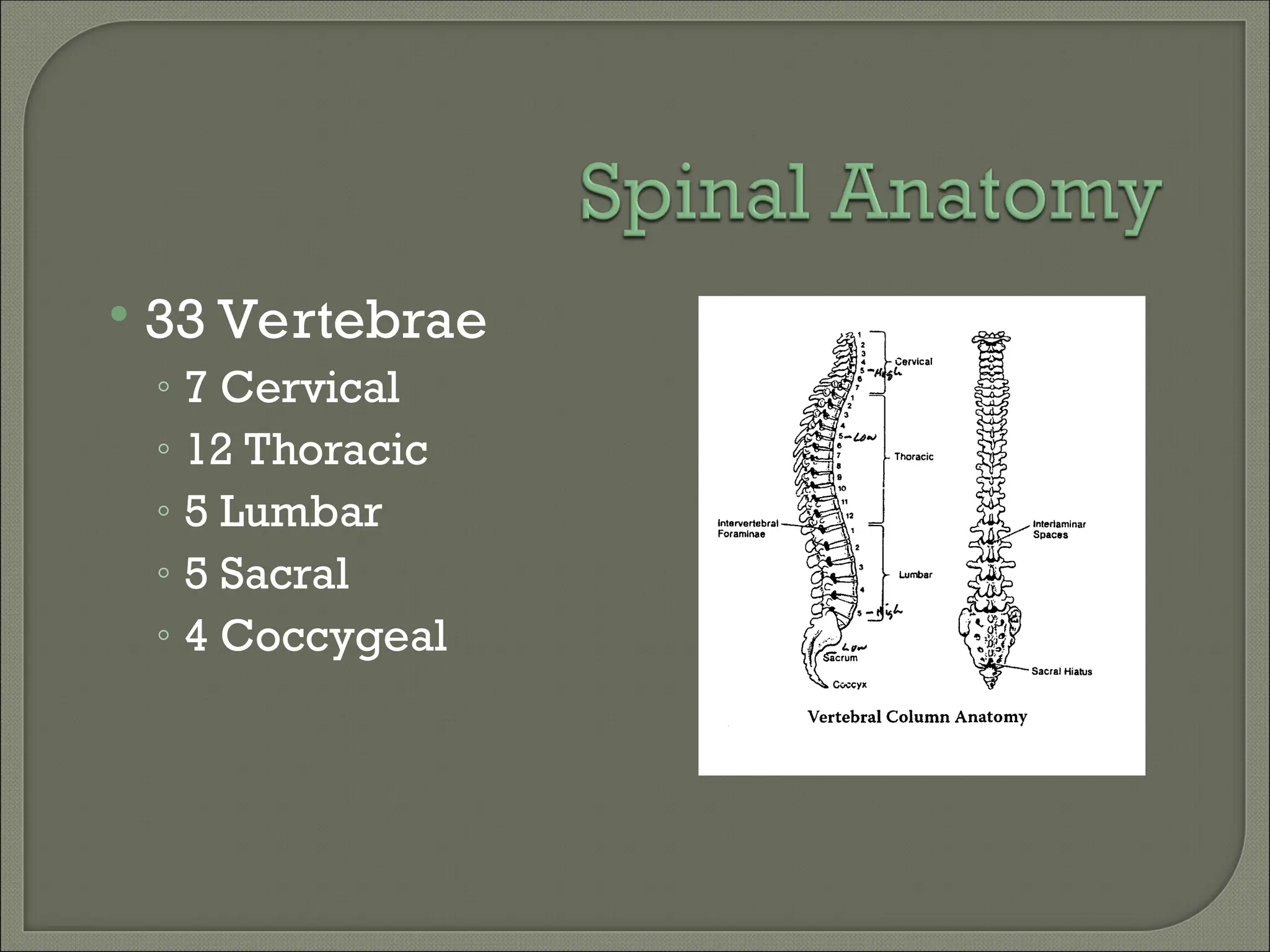
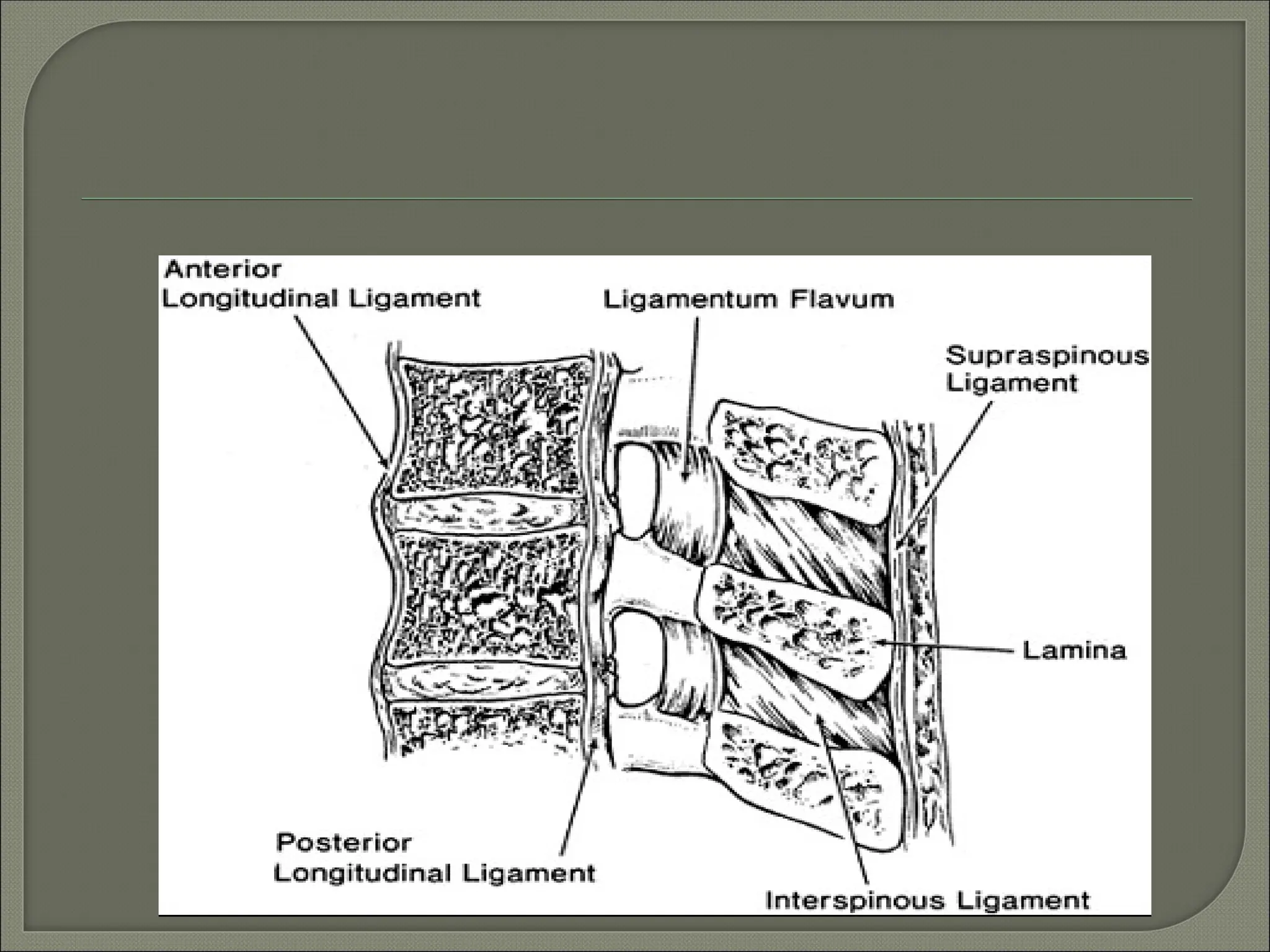
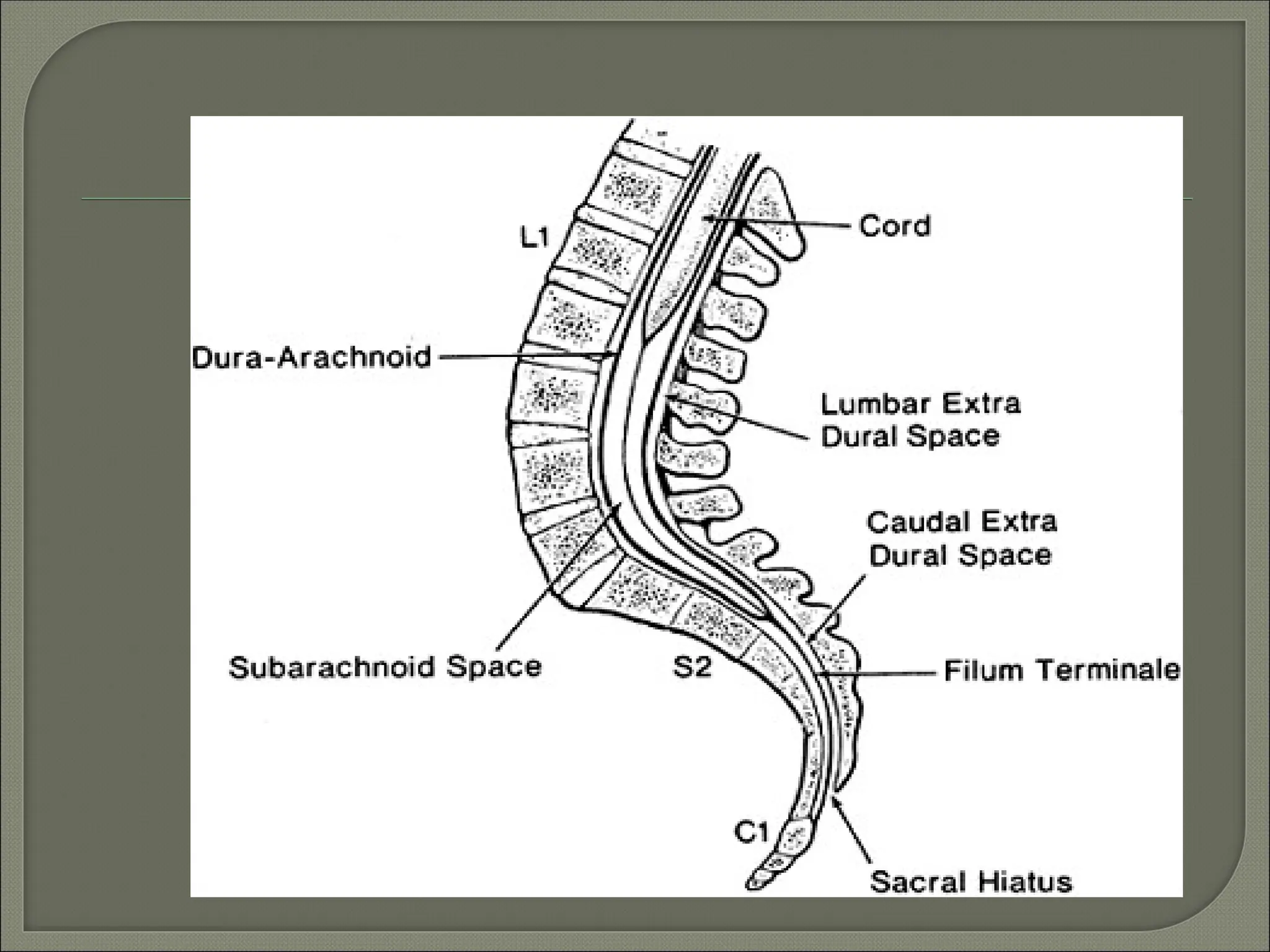
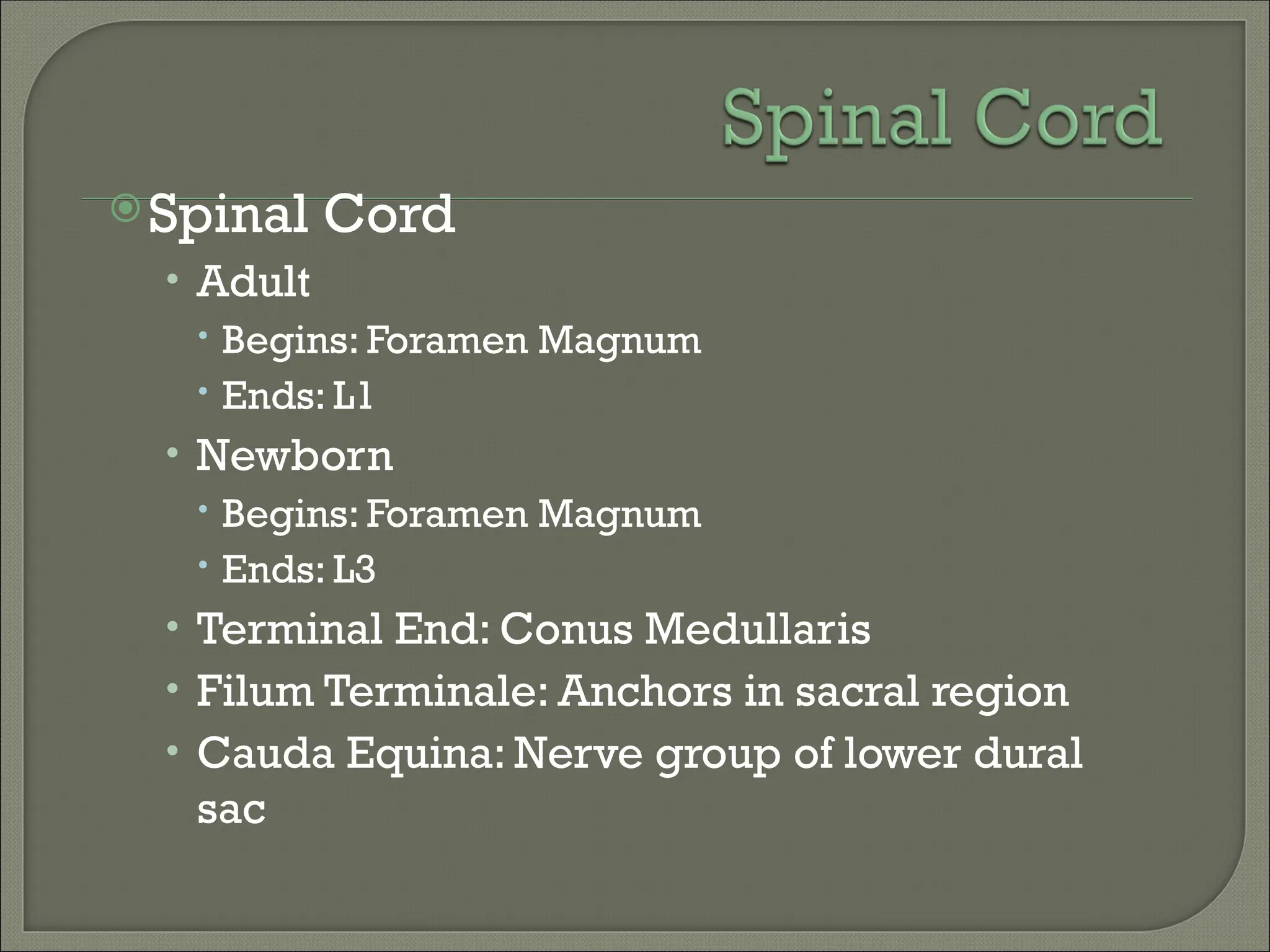
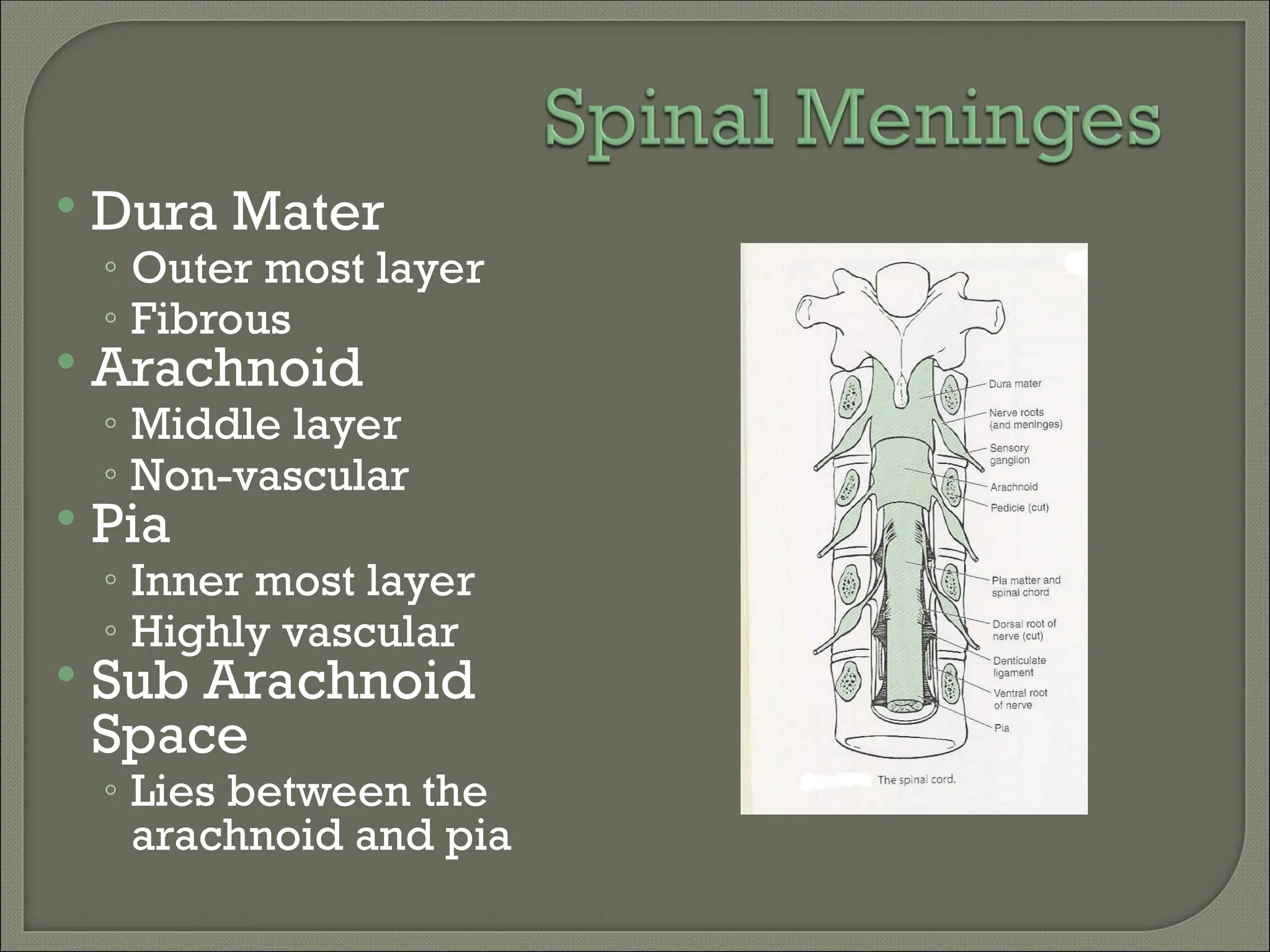
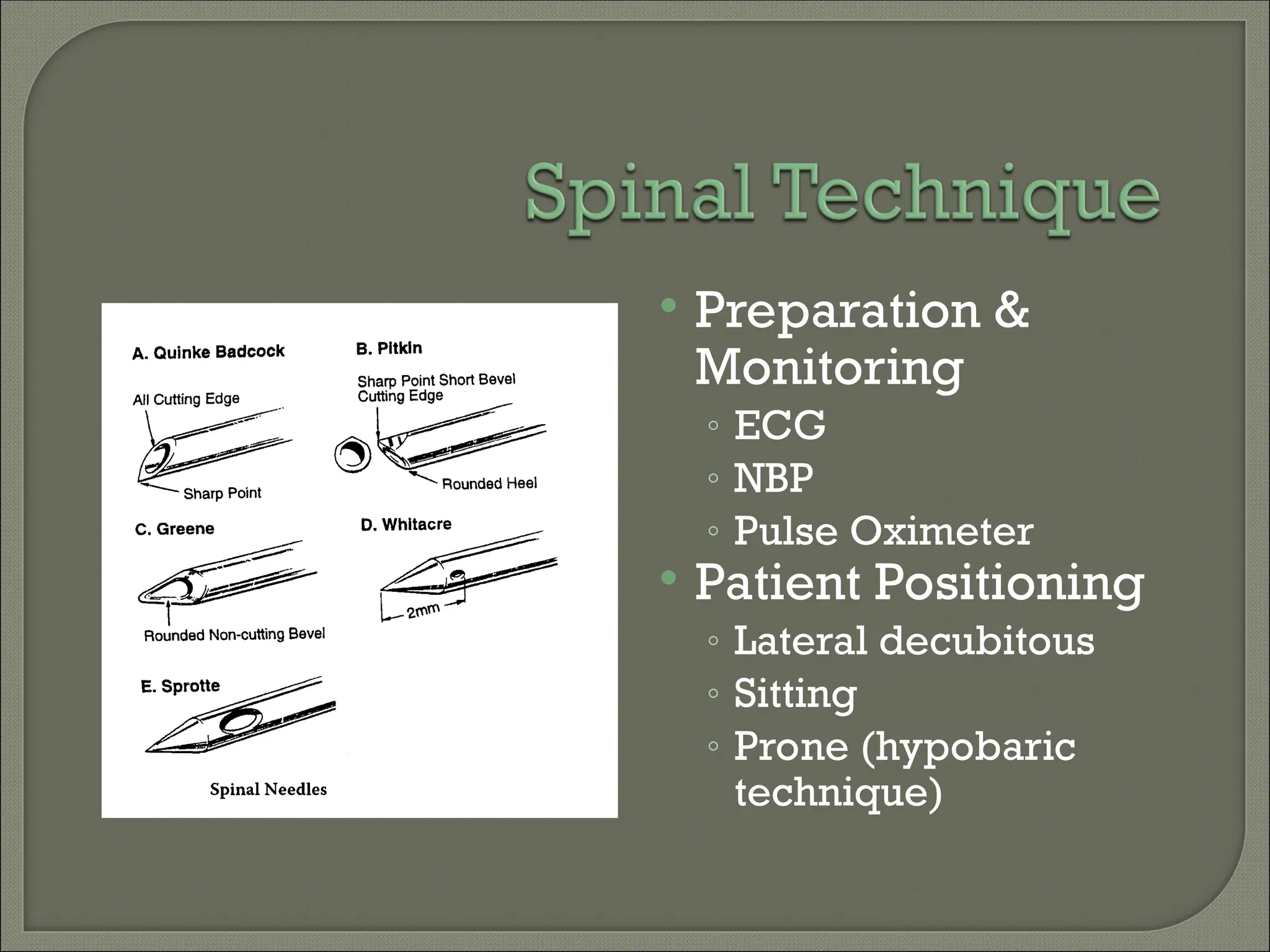
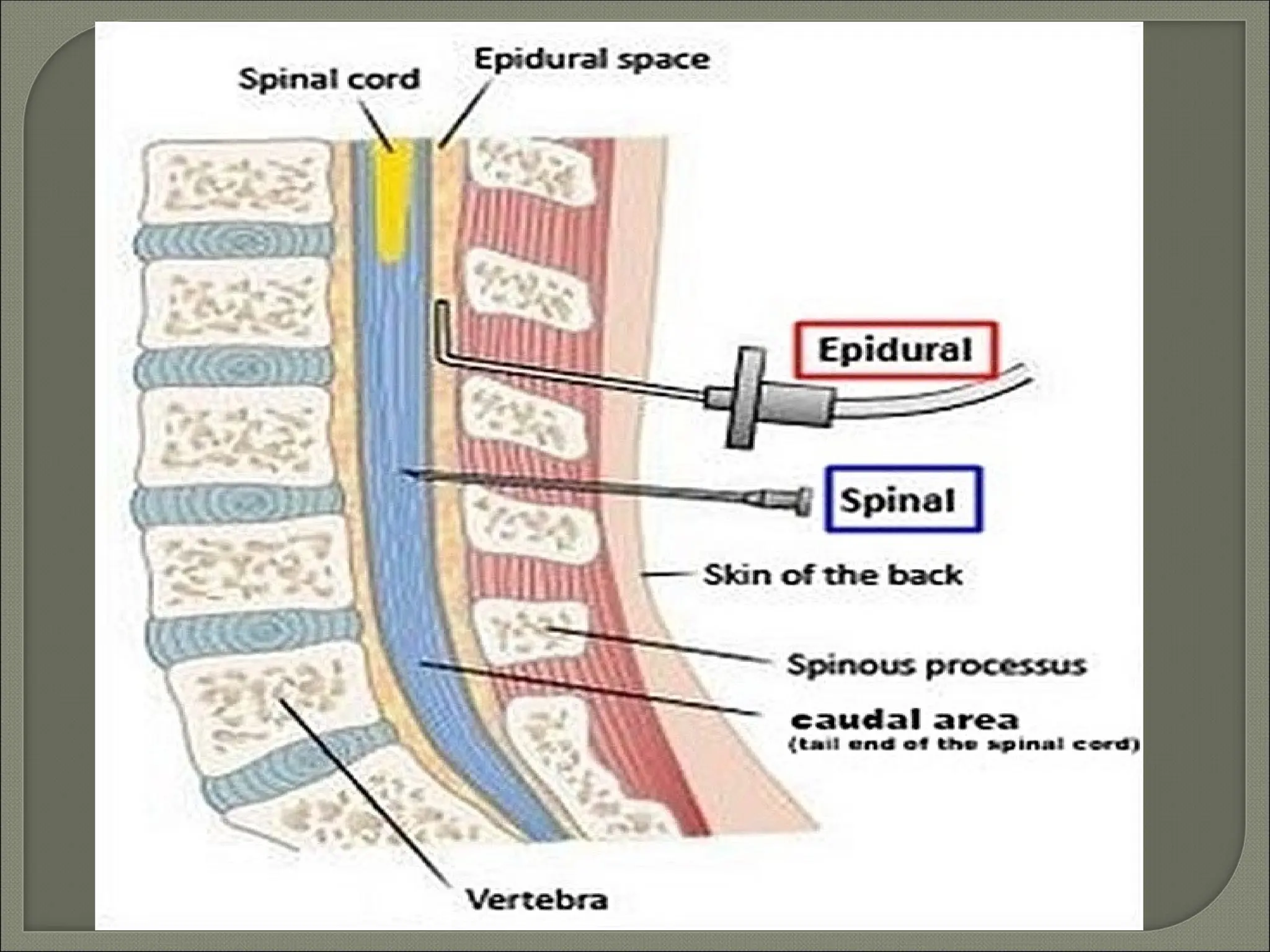
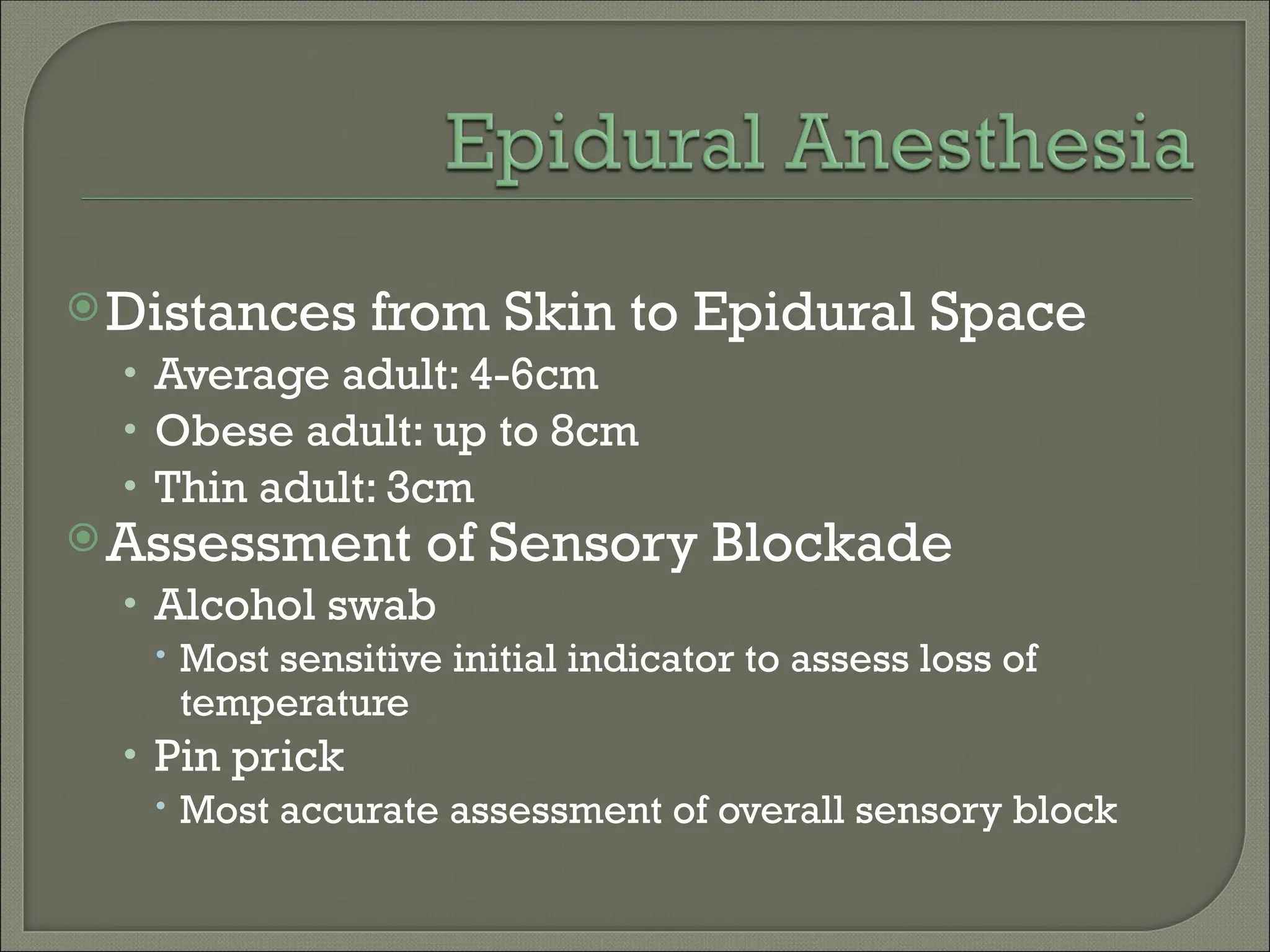
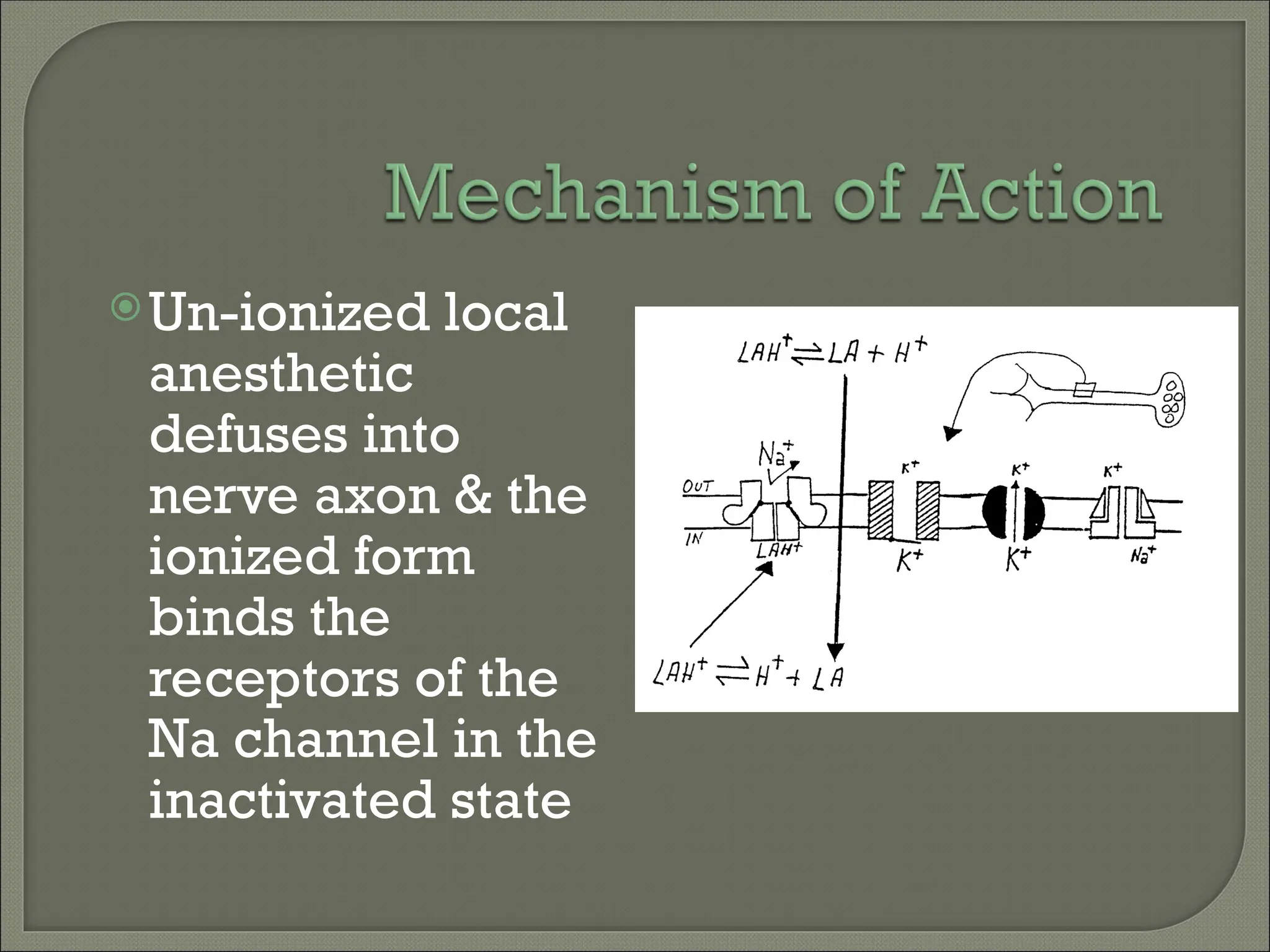
The document provides a comprehensive overview of regional anesthesia, specifically spinal, epidural, and caudal blocks, detailing their benefits, anatomical considerations, and contraindications. It discusses the layers of the spinal cord and meninges, as well as factors affecting the distribution and duration of anesthesia. Additionally, it covers potential complications, recommended dosages, and techniques for effective administration.