The document provides information about epidural anesthesia, including:
- Definitions, advantages, physiology, effects, dosages, factors influencing effects, levels, techniques, and contraindications of epidural anesthesia.
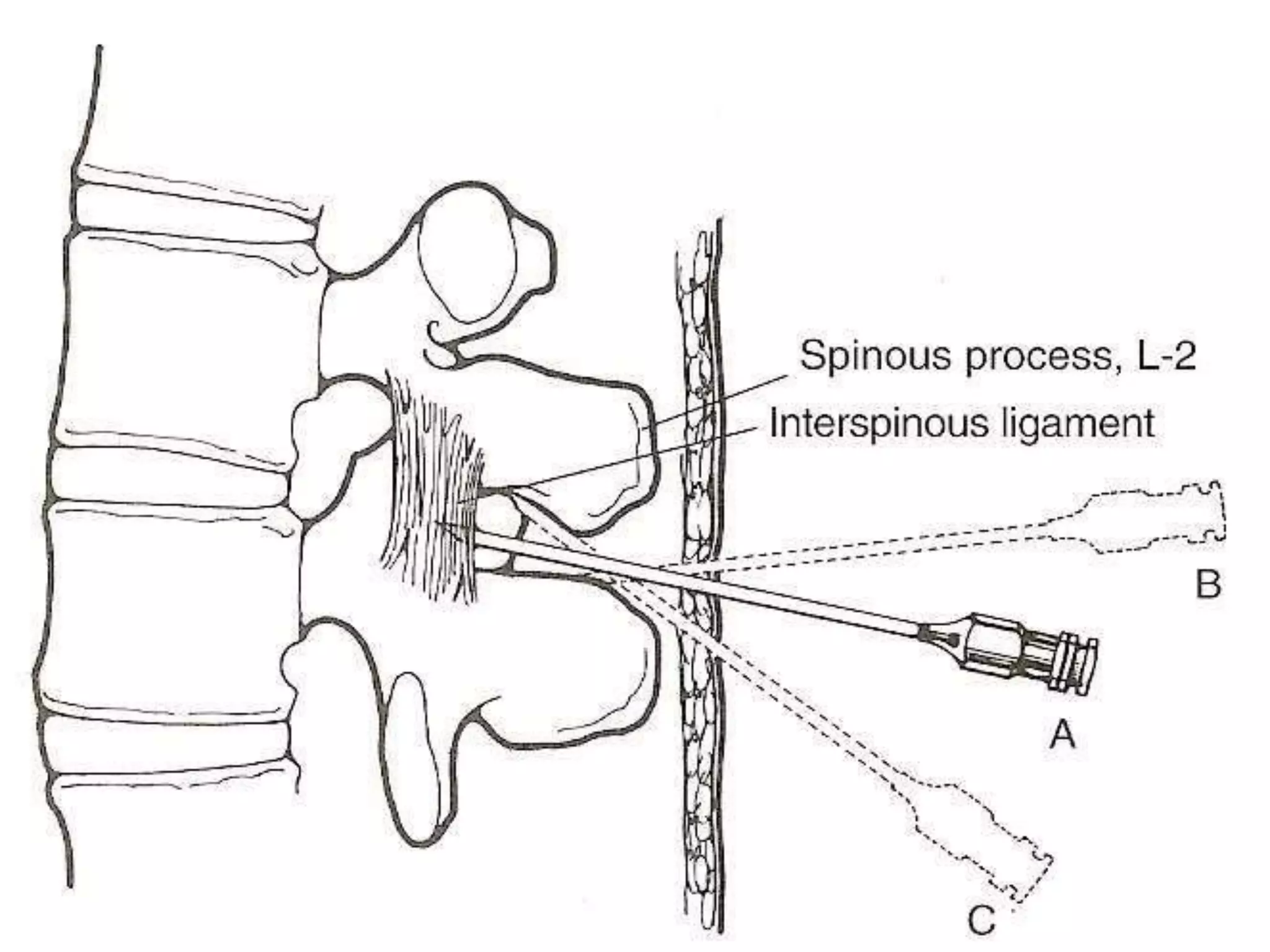
- Local anesthetics or other solutions injected into the epidural space spread anatomically within the epidural space and may diffuse into the cerebrospinal fluid and leak through intervertebral foramina.
- Injection site, dose, volume, concentration, position, age, and speed of injection can influence the level and spread of epidural blockade. Different local anesthetics have varying durations of effect from their administration via epidural.