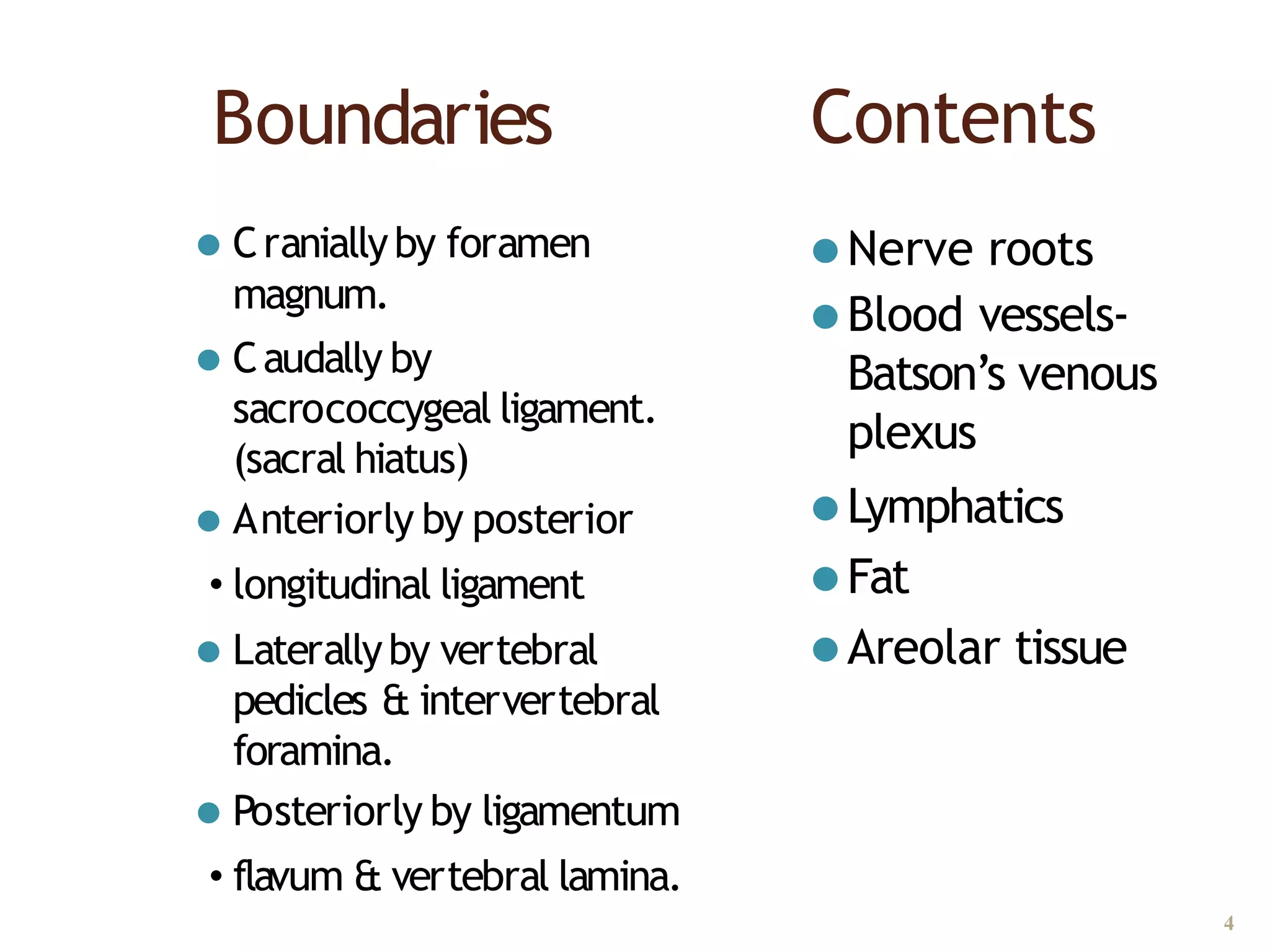
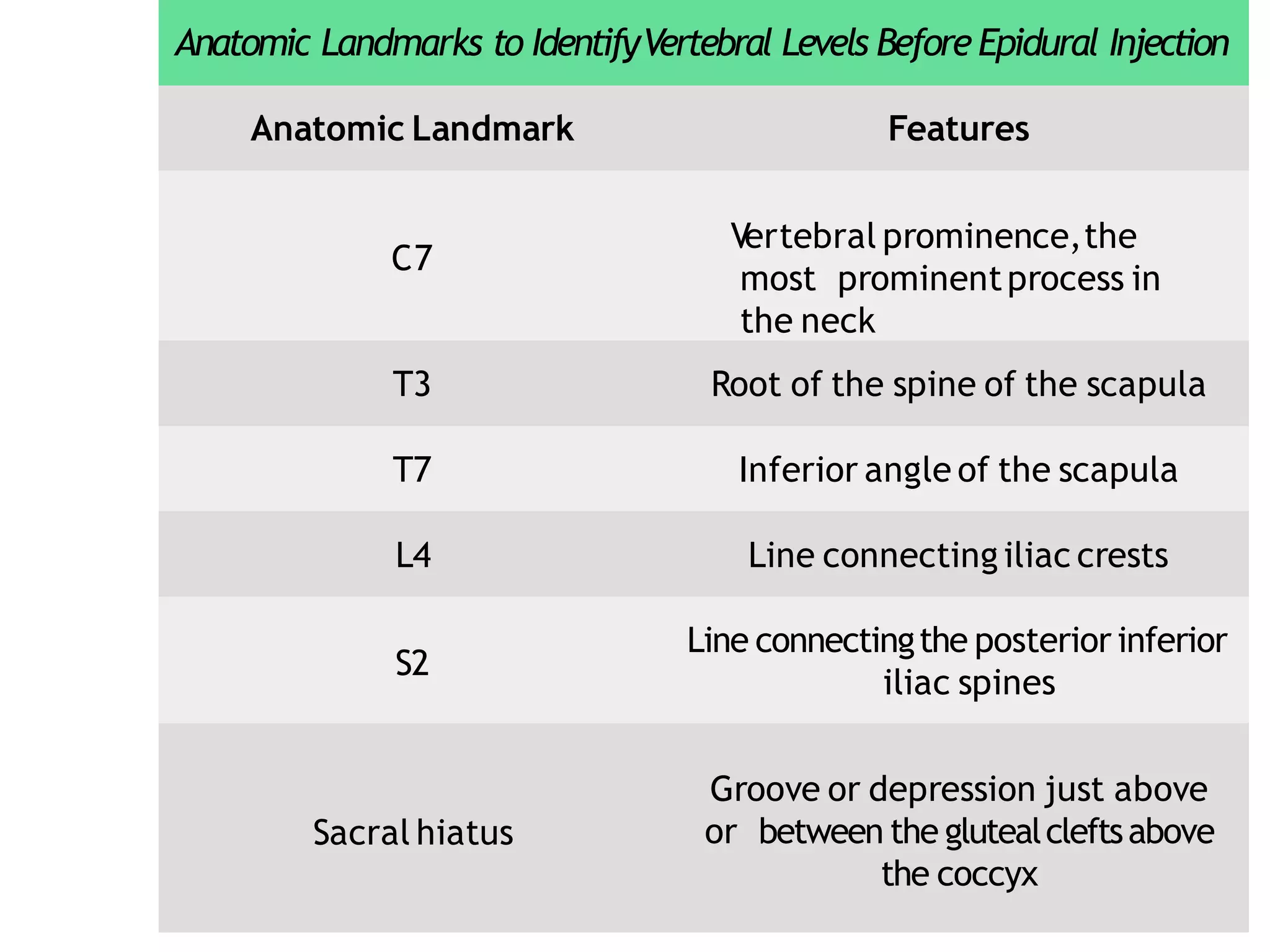
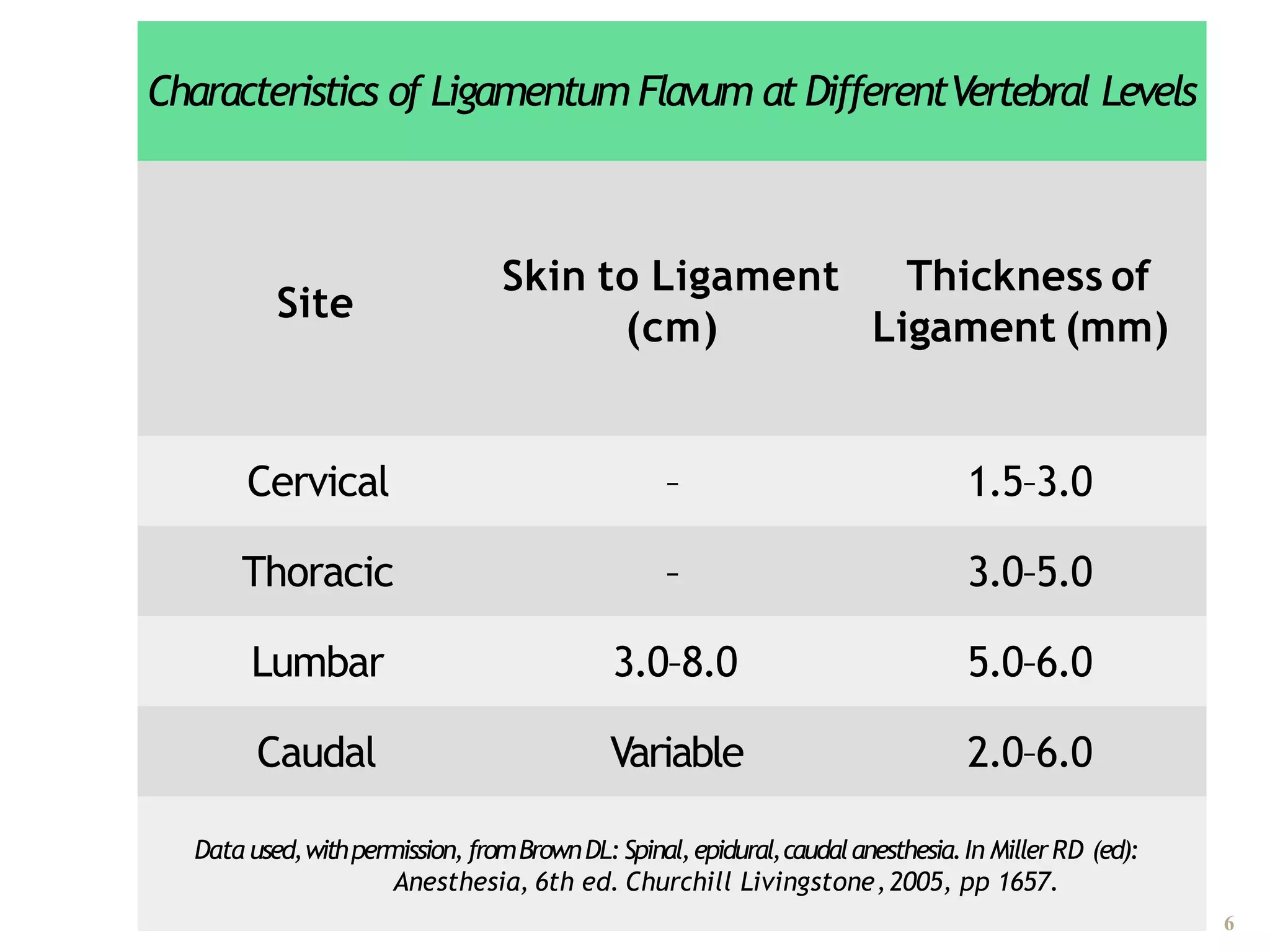
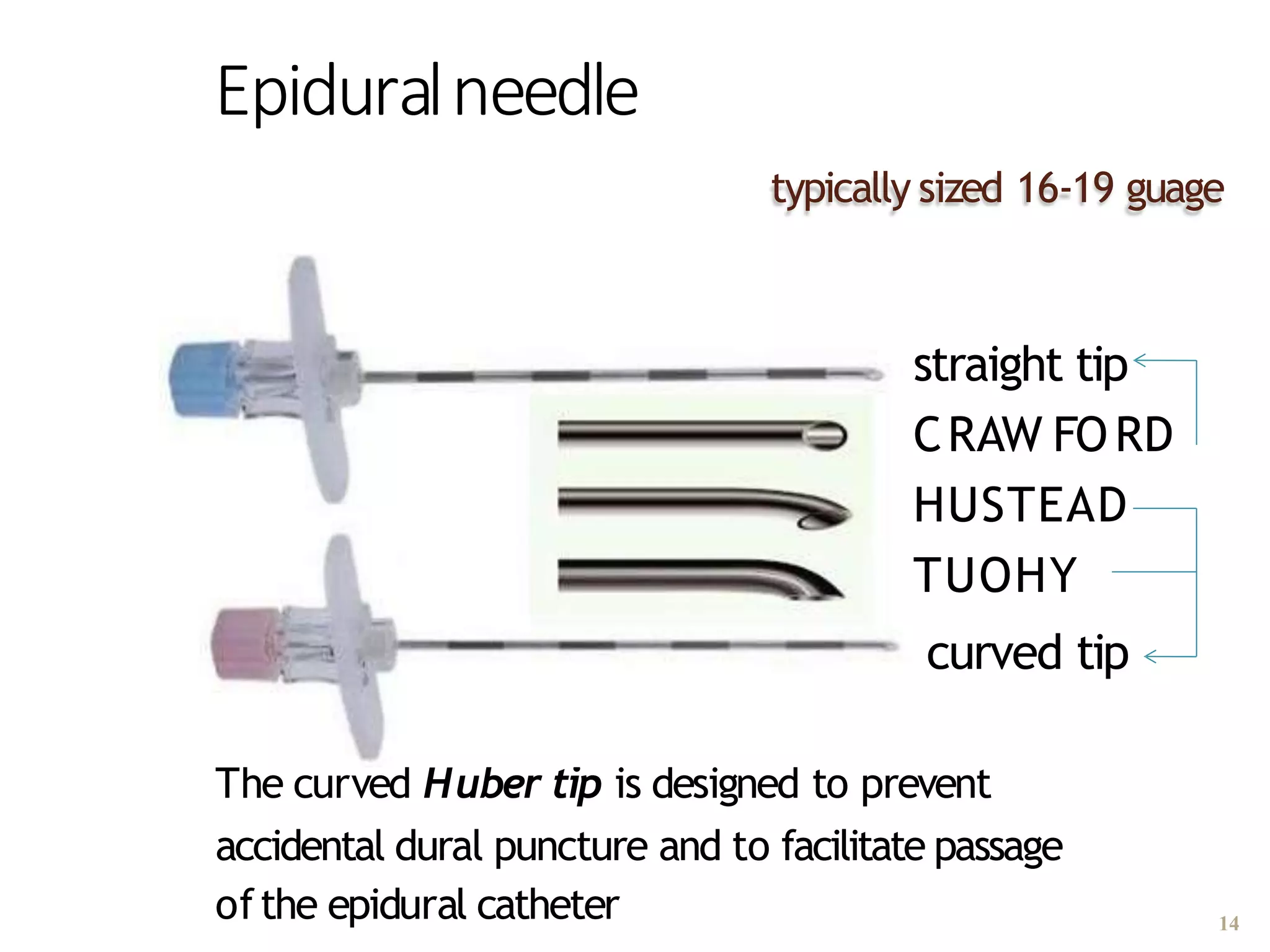
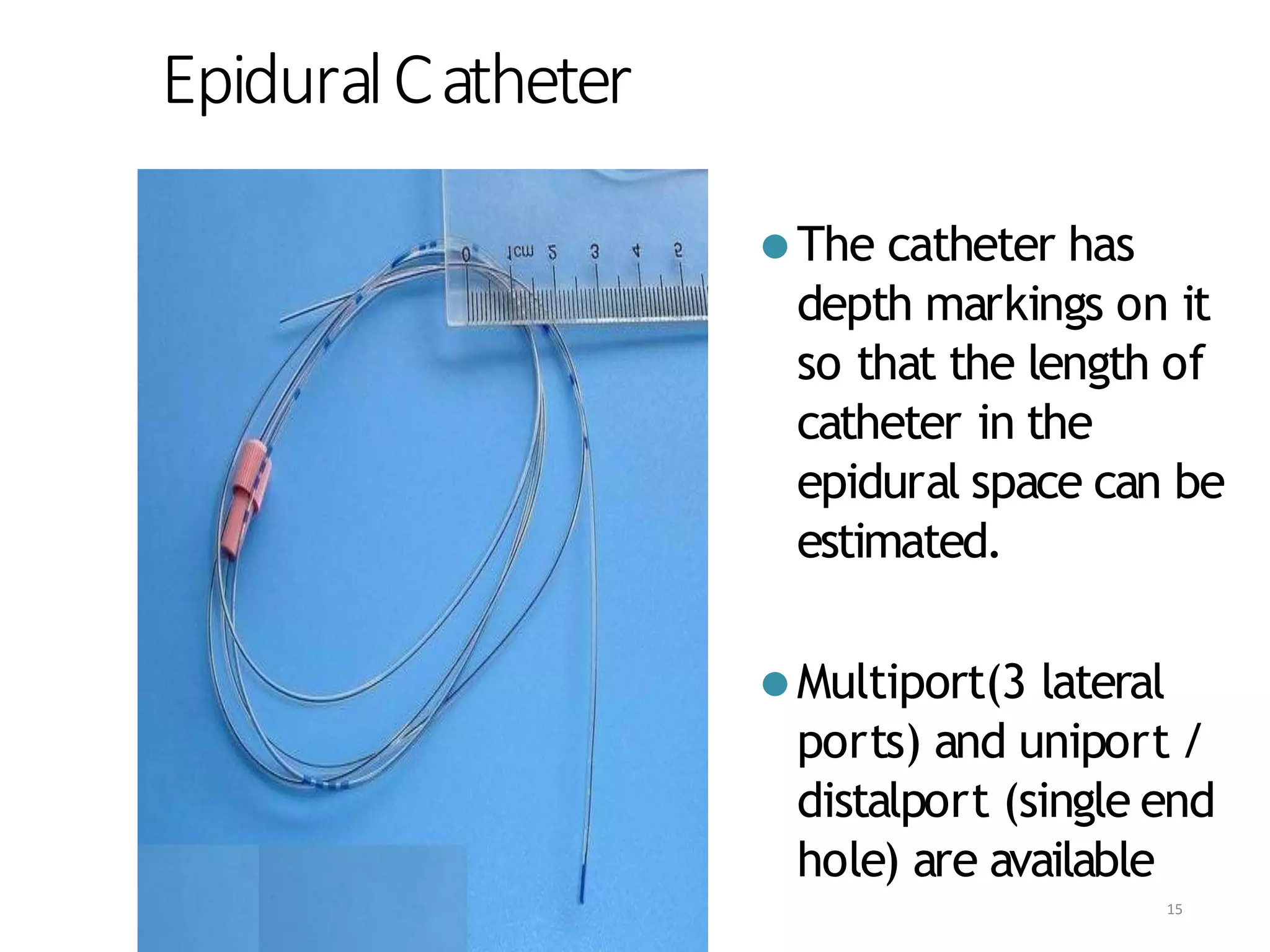
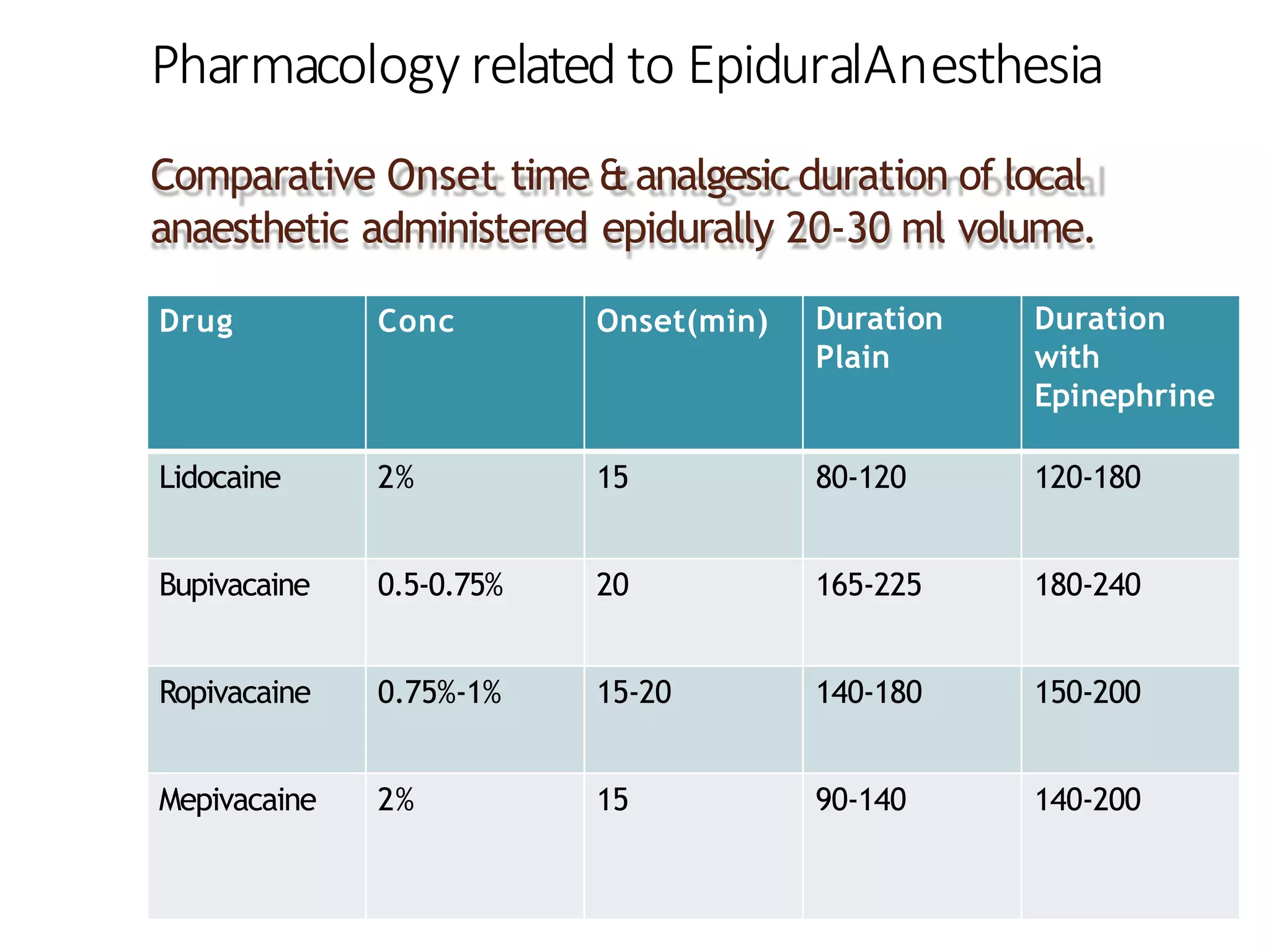
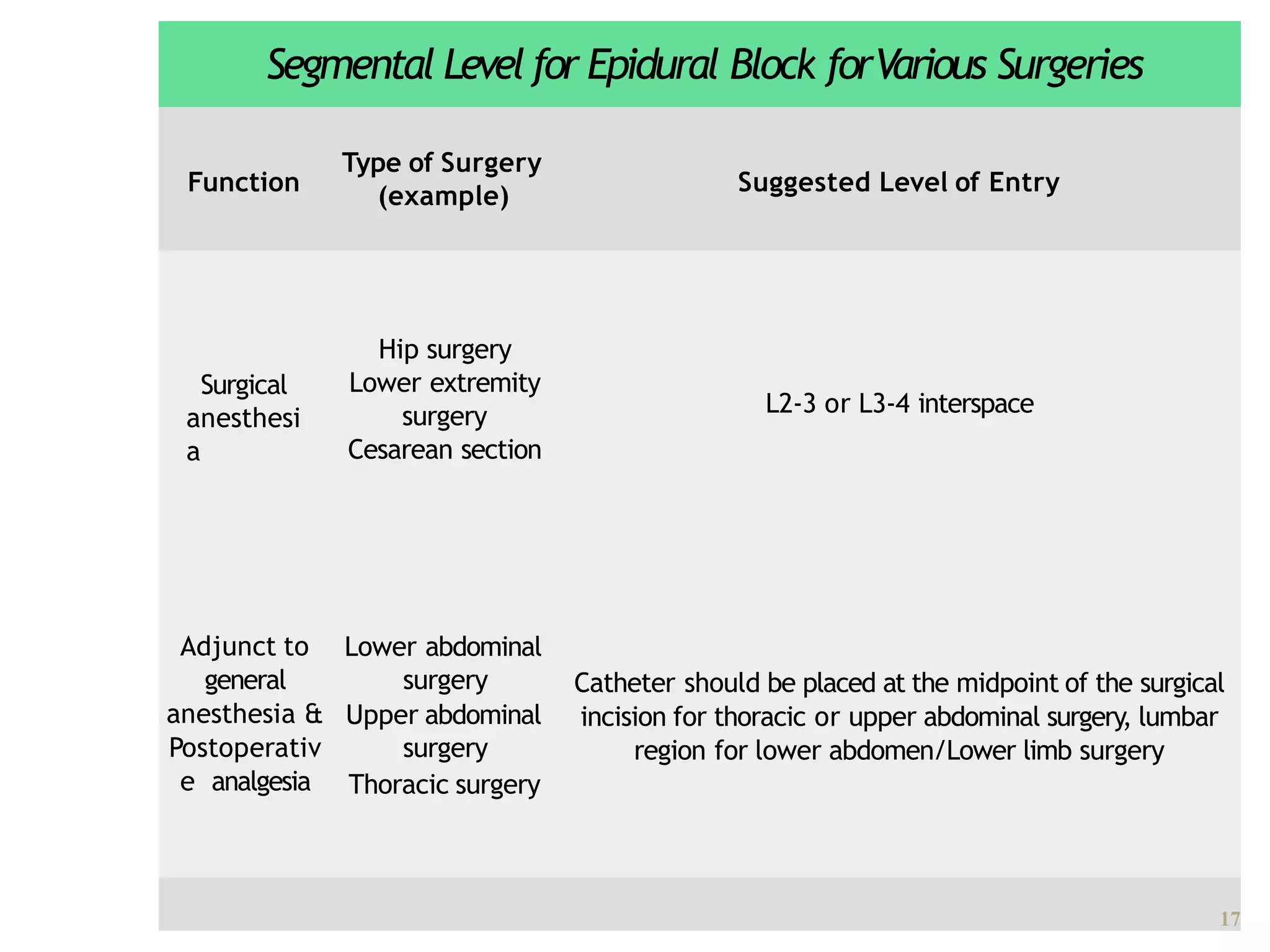
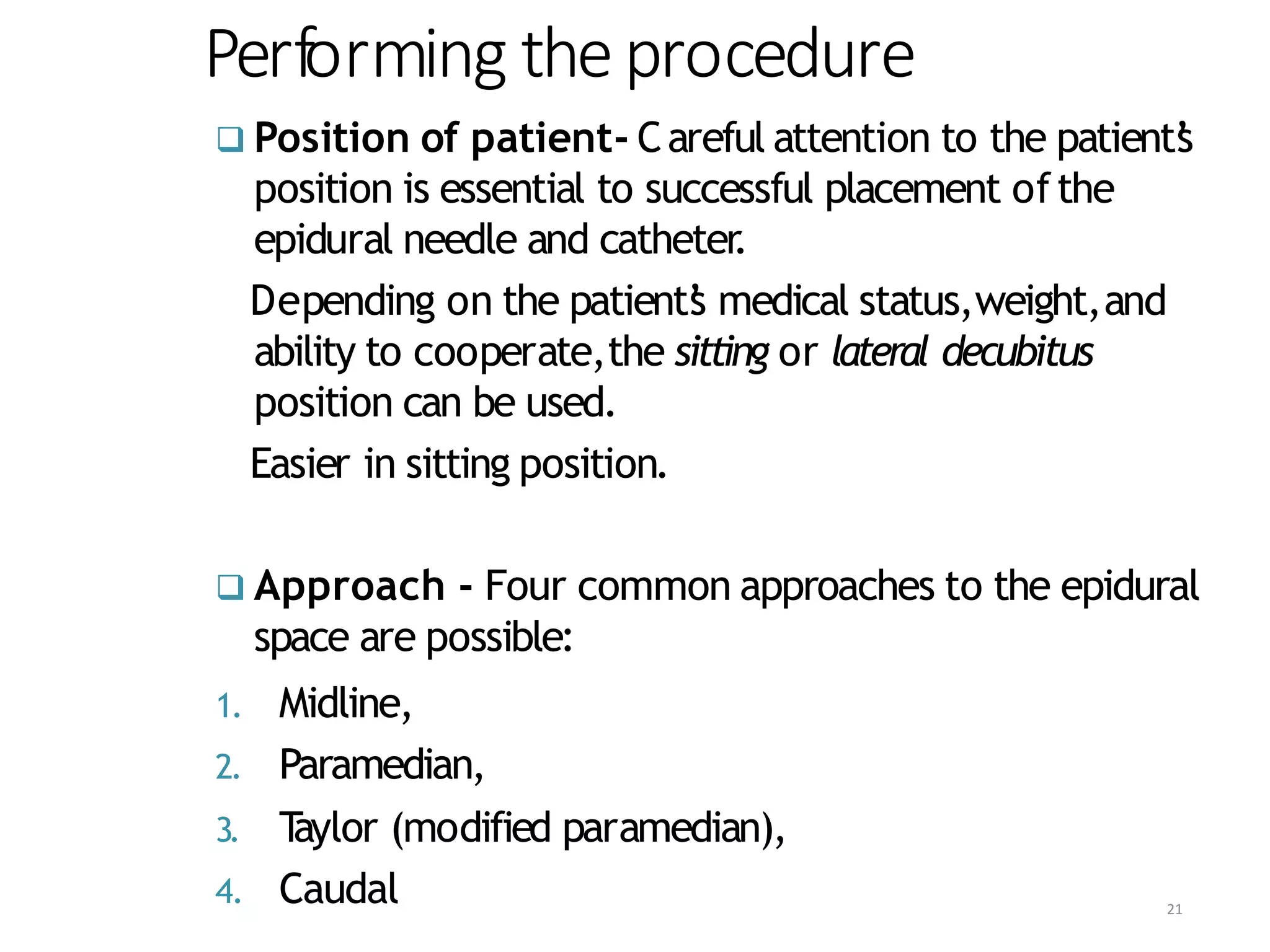
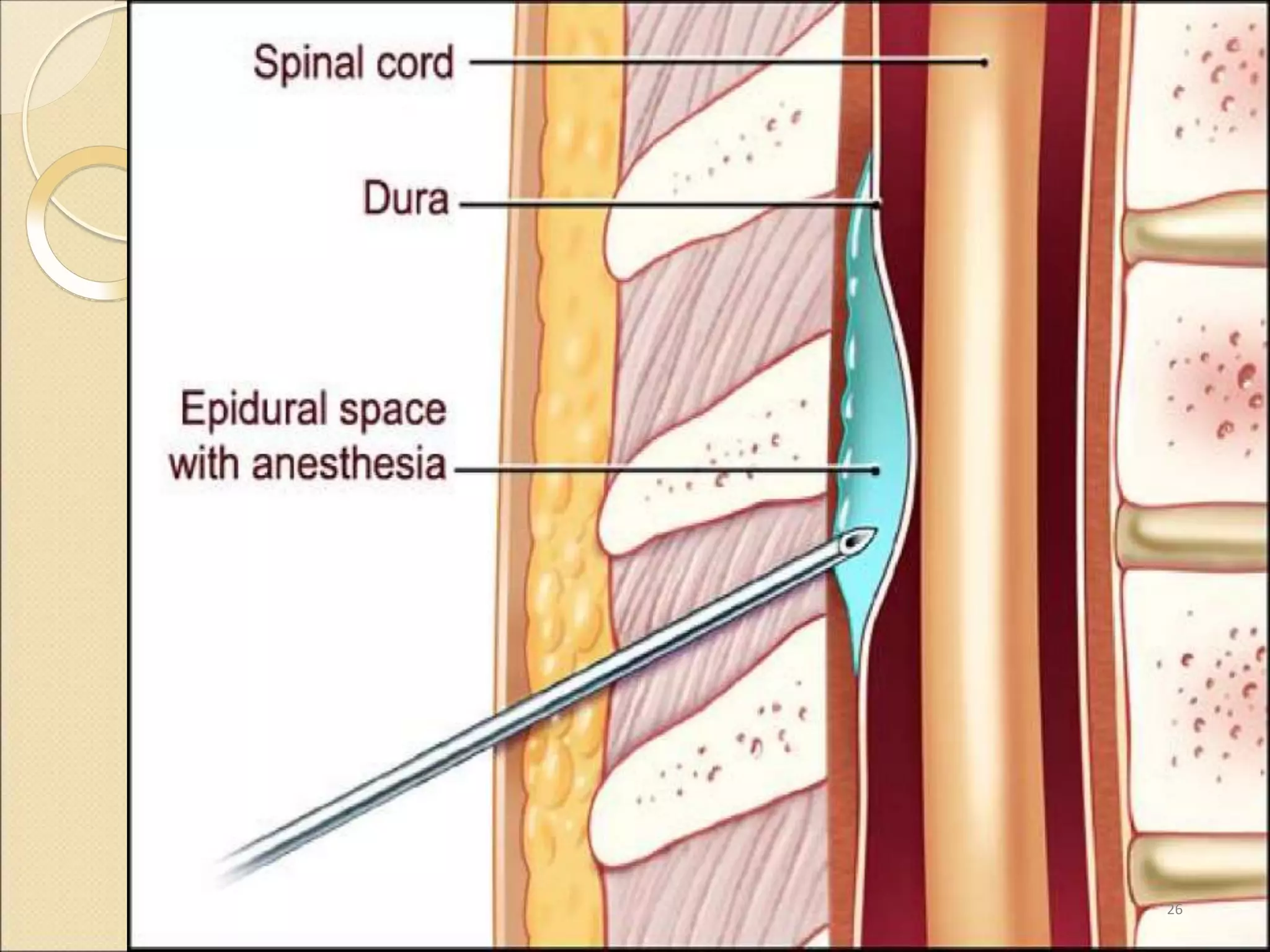
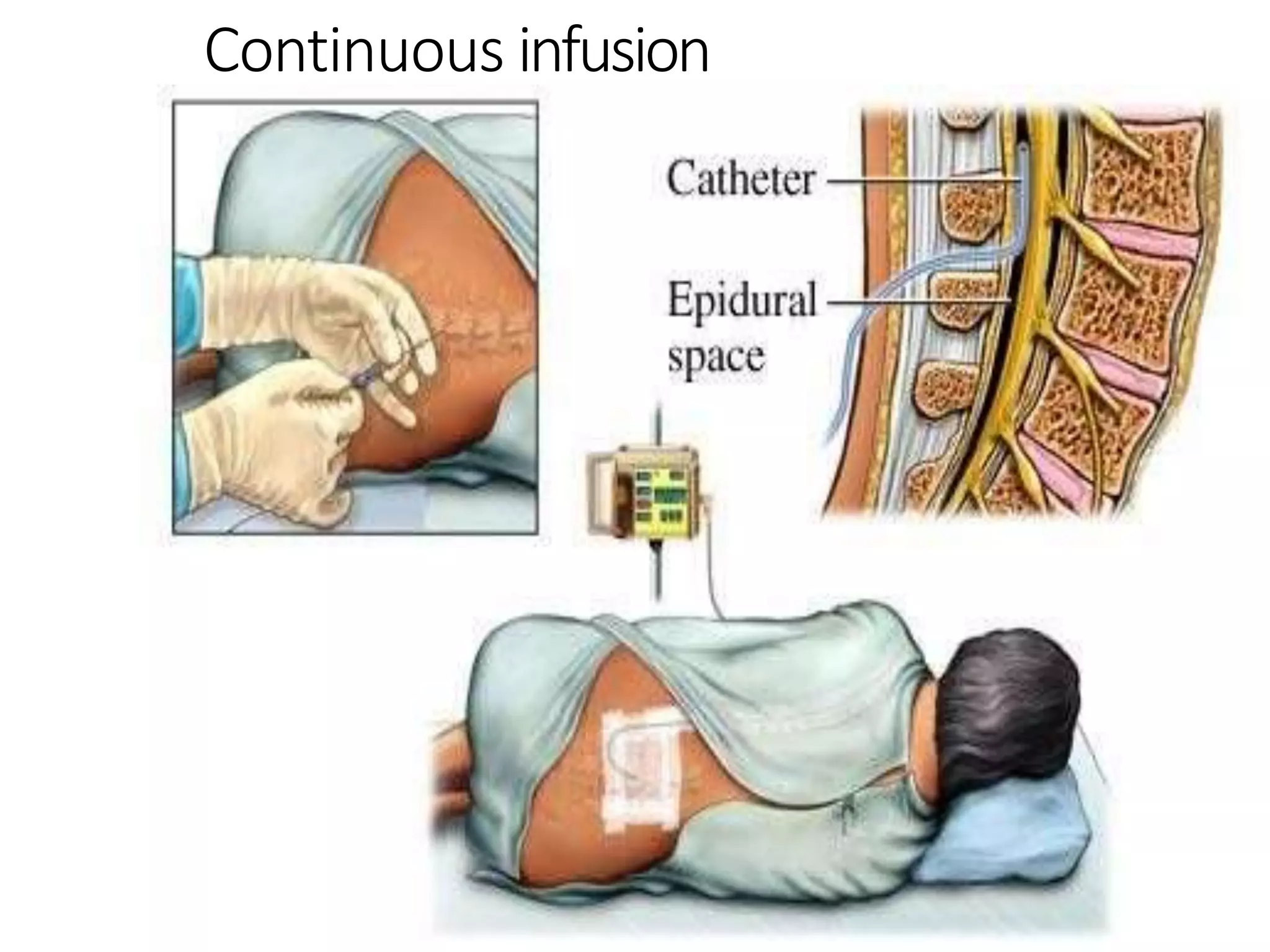
This document discusses epidural, caudal, and paravertebral block techniques. It begins with a brief history of epidural anesthesia and describes relevant anatomy like the epidural space and its boundaries. It then covers the indications, contraindications, advantages, and disadvantages of epidural anesthesia. The document discusses epidural needle and catheter types and placement techniques. It also provides details on pharmacology, dosing, and procedures related to epidural anesthesia.