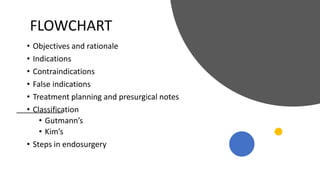
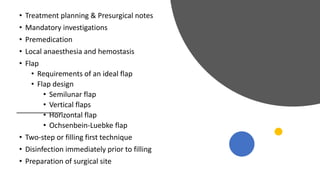
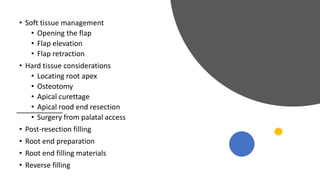
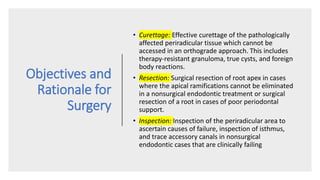
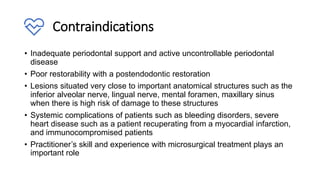
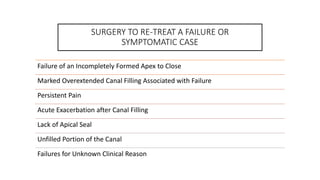
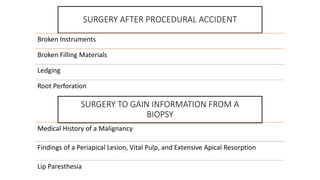
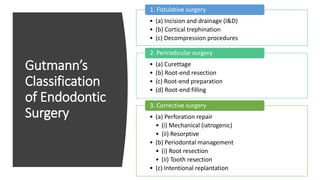
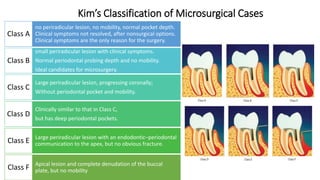
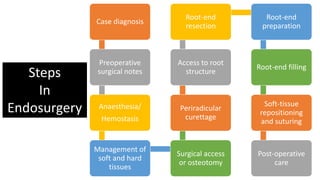
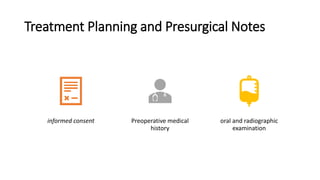
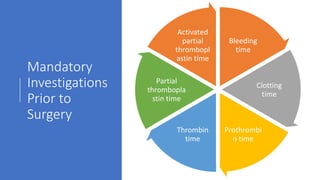
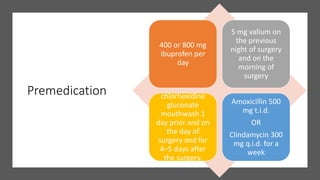
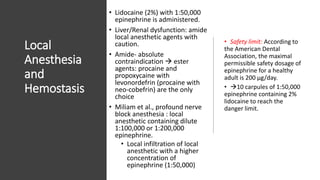
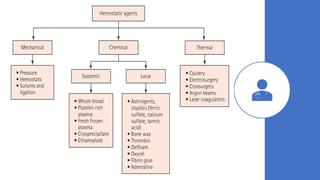
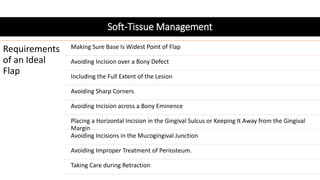
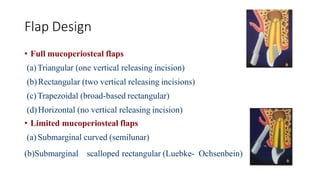
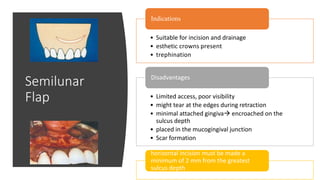
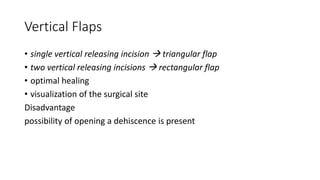
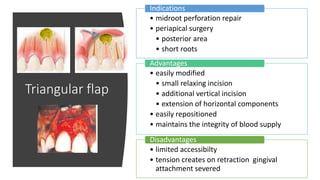
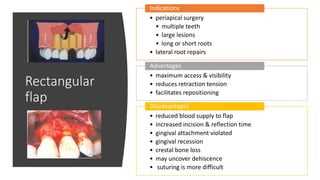
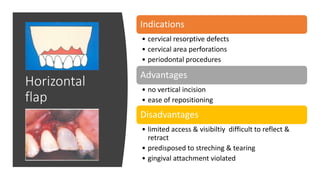
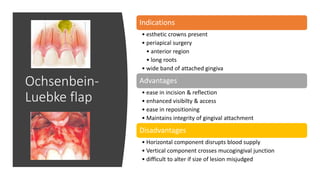
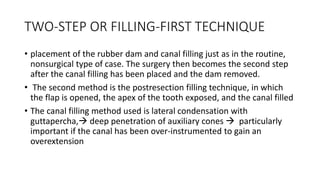
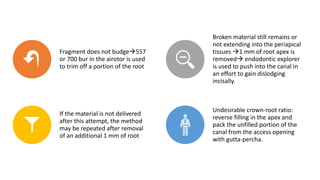
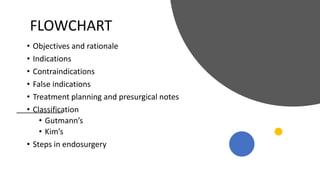
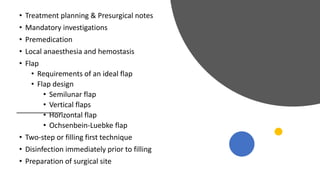
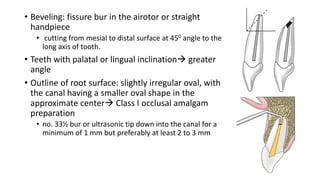
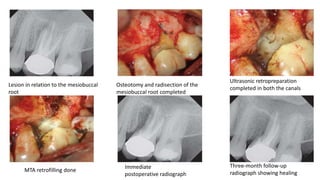
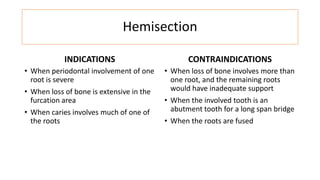
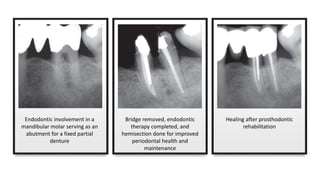
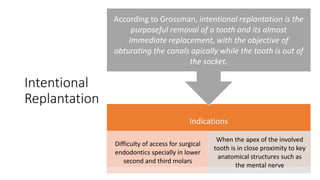
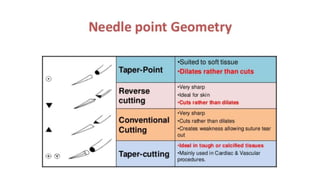
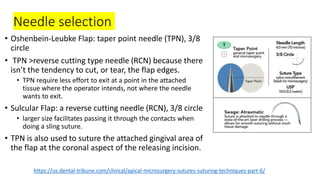
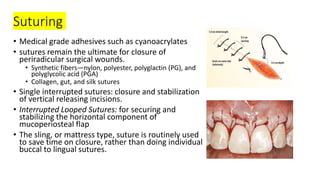
The document outlines endodontic surgery procedures, detailing objectives, indications, contraindications, classifications, and treatment planning essentials. It provides comprehensive insights into surgical techniques, flap designs, local anesthesia protocols, and postoperative care. Various classifications of endodontic surgery, including Gutmann's and Kim's, as well as specific procedural steps like osteotomy and apical curettage, are also covered.