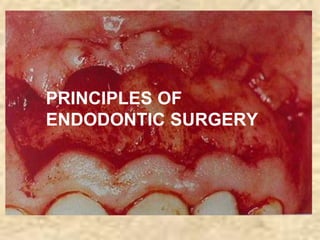
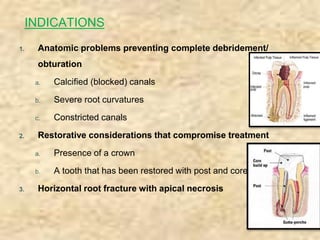
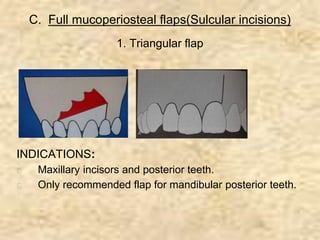
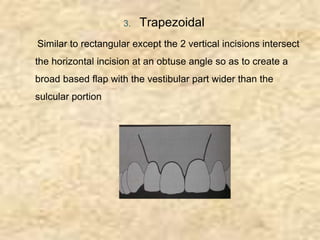
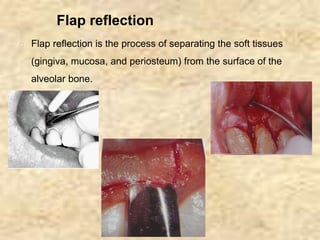
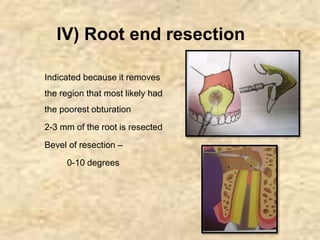
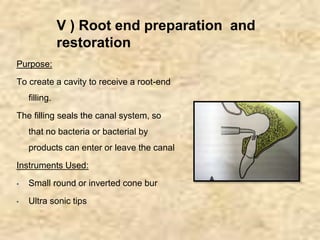
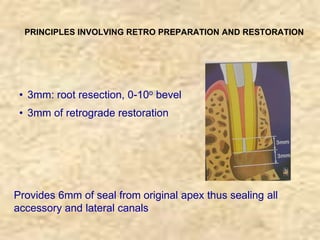
Endodontic surgery involves surgical management of periradicular pathosis. It includes procedures like abscess drainage, periapical surgery, corrective surgery, and root removal. The objectives are to remove causative agents of pathology, restore periodontal health, and provide a proper seal between the root canal and surrounding tissues. Periapical surgery may be indicated for anatomical issues preventing complete root canal treatment, restorative factors compromising treatment, root fractures with apical necrosis, retained materials, procedural errors, large periapical lesions not resolved by root canal treatment, or persistent symptoms after root canal treatment. Key steps involve flap design and reflection, periapical exposure, curettage, root-end resection, retrograde