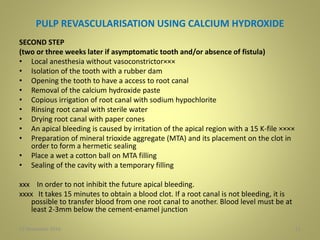
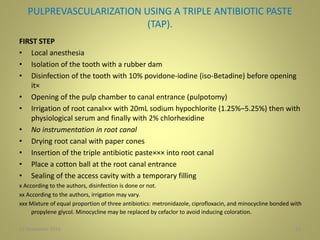
This document discusses revascularization procedures for immature permanent teeth with necrotic pulps. It begins by introducing the challenges of treating such teeth and the potential for revascularization to encourage continued root development. The history of revascularization is then reviewed, from early case studies in the 1960s demonstrating new tissue formation in root canals, to more recent definitions and understanding of the process. Key aspects of revascularization techniques using calcium hydroxide, triple antibiotic paste, and their two-step protocols are then outlined. Considerations for instrumentation, irrigation, and medication of the root canal are also presented.
![DEFINITION
• Trope [2008] claimed that the term revascularization was chosen
because the nature of the tissue formed posttreatment was
unpredictable, and the only certainty was the presence of a blood
supply; hence it was ‘‘revascularized.’’
• Lenzi and Trope 2012 suggested the term revitalization as being
more appropriate because it is descriptive of the nonspecific vital
tissue that forms in the root canal. Huang GT, 2008
Revascularization can be broadly defined as the restoration of
vascularity to a tissue or organ.
• Wigler R 2013 suggested that the term apexogenesis be used for
procedures designed to encourage continued apical development
in teeth with some vital tissue in the root canal, and the term
maturogenesis be used for procedures that promote continued
root development in infected immature permanent teeth, rather
than revascularization or revitalization.
627 November 2016](https://image.slidesharecdn.com/revascularisation-161127062752/85/Revascularisation-6-320.jpg)
![INSTRUMENTATION.
• Two types of cells are required to achieve a normal root
development: odontoblasts and epithelial cells of
Hertwig’s sheath. These two cell types are present in
abundance in the apical area of immature teeth and are
able to resist inflammation phenomena [N. Shah et al.
2008, A. Nosrat et al 2011].
• These cells will be able to differentiate into secondary
odontoblasts that will generate dentin on root canal
walls and thus allow root maturation.
• No instrumentation procedure remains consistent with
vital stem cells preservation and avoids weakening of
already thin root canal walls. Thus, elements
mentioned so far in favor of no instrumentation
protocol seem to be more advised.
1927 November 2016](https://image.slidesharecdn.com/revascularisation-161127062752/85/Revascularisation-19-320.jpg)
![Sodium Hypochlorite.
• It has a solvent action on necrotic tissue and an antiseptic
effect widely demonstrated. However, it must be
supplemented by a desalting.
• Recommended concentrations vary between 0.5% and
5.25%. Cytotoxicity of sodium hypochlorite is proportional
to its concentration.
• The concentration of 2.5% seems to be the best
compromise between efficiency and lack of toxicity [M.
Zehnder, 2006].
• Cunningham (1980) showed that elevation of the
temperature at 37°C of the 2.5% sodium hypochlorite
solution potentiates its solvent power and its efficiency
becomes comparable to that of the solution to 5,25% .
2327 November 2016](https://image.slidesharecdn.com/revascularisation-161127062752/85/Revascularisation-23-320.jpg)
![Ethylene Diamine Tetraacetic Acid
(EDTA)
• Chelators are weak acids, which react with the mineral
portion of dentinal walls. They replace calcium ions with
sodium ions, which combine with the dentin to give soluble
salts.
• EDTA-type chelating allows better wettability of the irrigator
and a removal of the smear layer.
• 17% of EDTA is often used in cases of bacterial infection to
remove the smear layer and allow access to the entrance of
dentin tubules (allowing a better chance of joining tissue of
regeneration) and induce a better penetration of the irrigator
(increases wettability of the irrigator) and of root canal
medications [B.O. Aktener andU. Bilkay, 1993]
2627 November 2016](https://image.slidesharecdn.com/revascularisation-161127062752/85/Revascularisation-26-320.jpg)
![CaOH
• Calcium hydroxide used at a concentration of
0.01 mg/mL for canal disinfection allows survival
of 100% of the apical stem cells.
• Even at higher concentration, 1mg/mL,
Ca(OH)would also give a maximal survival of stem
cells. At the same concentration, antibiotics paste
only allows between 33% and 56%cells survival.
Used in normal concentrations, antibiotics paste
is more toxic than Ca(OH), unless if they are used
in appropriate concentrations (lower
concentrations) [N. B. Ruparel et al 2012].
2927 November 2016](https://image.slidesharecdn.com/revascularisation-161127062752/85/Revascularisation-29-320.jpg)
![Triple Antibiotic Paste (TAP)
• No antibiotics have a spectrum large enough to be
active against all types of bacteria present in root
canals and apical regions; a combination of antibiotics
is essential to cover a maximum range of action.
• Antibiotics pastes must be used in proper
concentration for a balance between a lower
cytotoxicity against stem cells (cytotoxicity increases
with dose) and a maximum bacterial disinfection. An in
vitro study has shown that a TAP concentration of 39𝜇
g/mL would be best for application in disinfection root
canal [S.Chuensombat, 2013].
3027 November 2016](https://image.slidesharecdn.com/revascularisation-161127062752/85/Revascularisation-30-320.jpg)
![TAP
Ph :
• Acidic pH of minocycline is not favorable for cultivation of stem
cells; it would probably facilitate cell permeability of the antibiotic,
which would keep long-term cytotoxicity.
• Ciprofloxacin has also an acidic ph.
• Metronidazole is the only antibiotic of the mixture to have a neutral
pH and thus it has no cytotoxicity for needed stem cells.
• Metronidazole and ciprofloxacin could induce the formation of
fibroblasts .
• According to Bose et al.,[2009] the use of triple antibiotic paste
shows the highest percentage increase in thickness of the dentinal
canal walls compared to the two other intracanal medications
(calcium dihydroxide and formocresol)
• According to Adl et al., antibiotics have a better action against
Enterococcus faecalis than calcium dihydroxide.
3227 November 2016](https://image.slidesharecdn.com/revascularisation-161127062752/85/Revascularisation-32-320.jpg)
![Limitations of TAP
1. Bacterial resistance. Recent reports have shown that this is already
developing in bacteria recovered from endodontic infections [sedgley CM,
lee EH. Et al. 2008].
2. A risk of precipitating an allergic reaction in a sensitive patient or inducing
sensitivity in a patient who has never been sensitive. These concerns
highlight the need for a full and comprehensive medical and dental
history of the patient before treatment, regardless of the method of
administering the antibiotic during the course of treatment.
3. Tooth discoloration due to tetracycline.
• Tetracycline would have ability to inhibit collagenase and
metalloproteinases; it is not cytotoxic and is capable of increasing the level
of interleukin-10 (anti-inflammatory cytokine). Minocycline is a
semisynthetic tetracycline derivative with a similar action spectrum. It may
be replaced by cefaclor in order to avoid any risk of unaesthetic coronary
coloring because minocycline binds to ions Ca++ by chelation and form
insoluble complexes. However, cefaclor appears to be less effective against
enterococci. An alternative could be to previously seal the dentinal tubules
of the pulp chamber (etching and bonding). 3327 November 2016](https://image.slidesharecdn.com/revascularisation-161127062752/85/Revascularisation-33-320.jpg)
![PULP-CAPPING MATERIALS (MTA AND
BIODENTINE)
• In vitro studies have demonstrated that calcium
dihydroxide and MTA, with their high pH, exert a severe
weakening effect on dentin walls during a period of two
weeks to two months [A. P. Leiendecker, Y.-P. Qi, A. N.
Sawyer et al.2012] However, samples sealed with MTA
seem to recover their mechanical properties as fracture
toughness after one year. It is not the case with
calciumdihydroxide [S. Hatibovi´c-Kofman, et al 2008].
• Biodentine has the same mechanical characteristics as
human dentin. Moreover, upon application of this material
in a cavity, it seems to fully expand and fill the space by its
plasticity.
• Another advantage is absence of coloring the cervical area
unlike MTA, excepted using white MTA.
3627 November 2016](https://image.slidesharecdn.com/revascularisation-161127062752/85/Revascularisation-36-320.jpg)
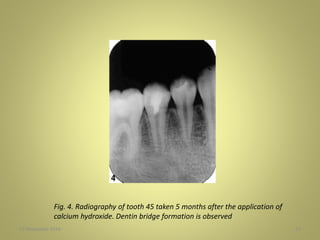
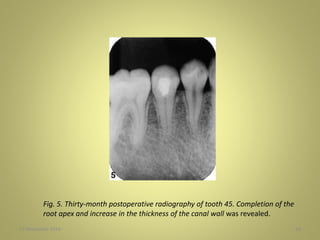
![THE TISSUE REGENERATION
• Claus et al. [2004] and Ritter et al. [2004] described histological
tissue regeneration in animals. They described the existence of a
significant neovascularization and the presence of connective cells.
• Through studies on animal cuts, the apposition material-inducing
thickening of root walls may be of different nature dentin,
cementum, or even bone [X. Wang et al. 2010].
• Therefore, this procedure is not a process of pulp revascularization
but a process of tissue regeneration.
• The inability to obtain sections of human teeth after
revascularization is a handicap for understanding and validating
this process. Only radiographic assessments of in vivo clinical
studies and the use of a laser quantifying blood flow (laser Doppler
flowmetry) can give us an idea of treatment success. [H. Strobl et
al. 2003]. Testing vitality with cold also seems to be a good
indicator of success. 3727 November 2016](https://image.slidesharecdn.com/revascularisation-161127062752/85/Revascularisation-37-320.jpg)
![UNFAVOURABLE OUTCOMES
• Lenzi and Trope 2012 found empty root canal space after
treatment of an immature maxillary central incisor with a necrotic
pulp.
• Nosrat et al. 20 12 showed the absence of vital tissue inside the
root canal space of treated immature maxillary incisors with
necrotic pulps after 6 years.
• Nosrat et al. 2013 presented a case where root maturation
occurred in a maxillary central incisor, even though a regenerative
endodontic procedure resulted in an empty root canal space.
• Even after using tissue engineering strategies, cementum-like hard
tissue was deposited on root canal walls, and bony islands were
found throughout the root canals.[Yamauchi N et al . 2011]
• Formation of a hard-tissue barrier inside the canals between the
coronal MTA plug and the root apex[ Chen MY et al. 2011] is
another reported unfavorable outcome.27 November 2016 41](https://image.slidesharecdn.com/revascularisation-161127062752/85/Revascularisation-41-320.jpg)