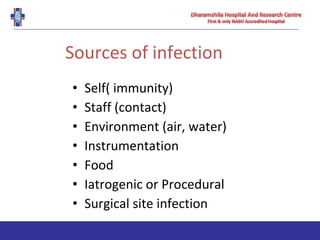
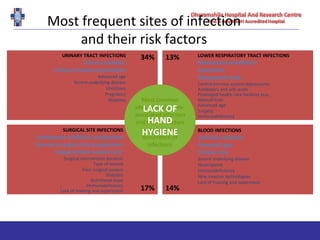
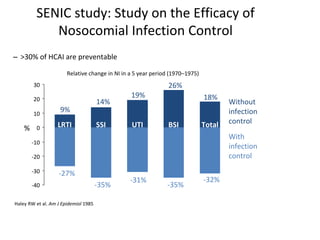
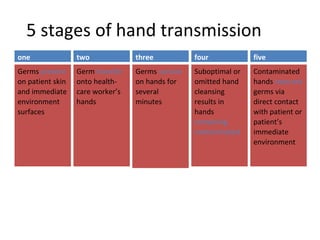
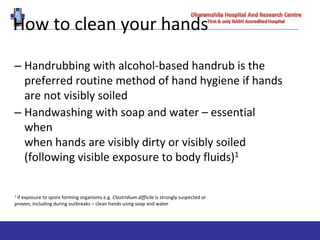
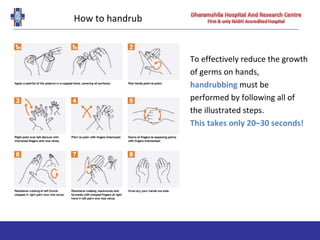
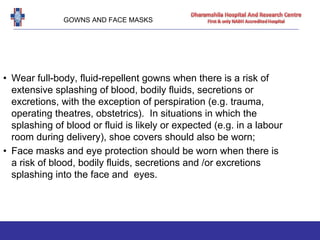
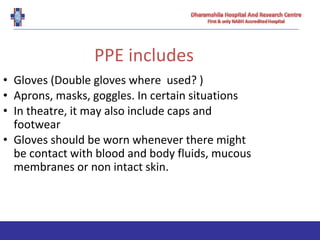
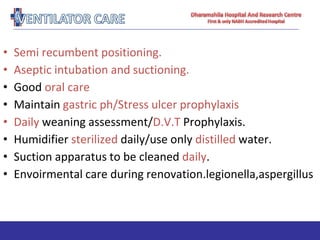
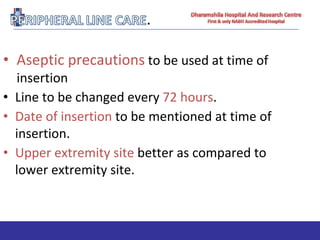
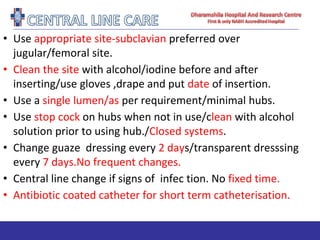
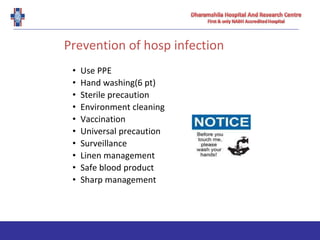
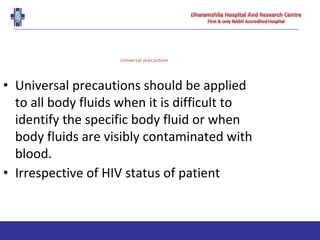
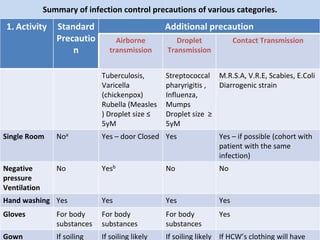
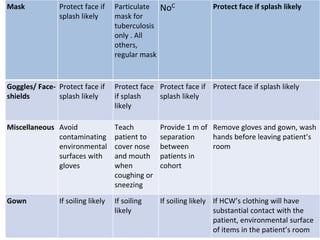
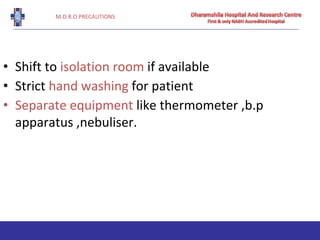
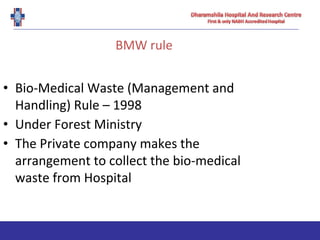
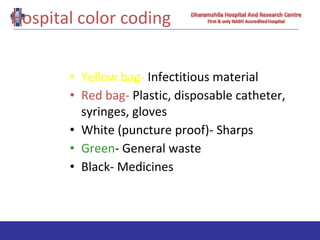
Hospital-associated infections, also known as nosocomial infections, can occur in patients receiving healthcare in hospitals or other facilities. They are caused by a variety of microorganisms that are able to spread via the hands of healthcare workers, medical equipment, other environmental surfaces, or through procedures. Proper hand hygiene and the use of personal protective equipment are essential for preventing the transmission of pathogens between patients and healthcare workers. Adhering to standard and transmission-based precautions can significantly reduce the risk of hospital-associated infections.