This document discusses factors that influence embryo transfer techniques and outcomes. It summarizes 3 key points:
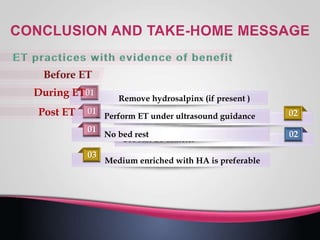
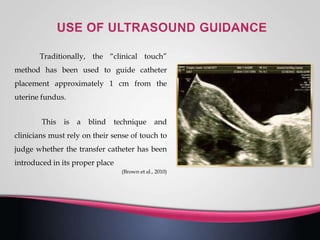
I. Embryo quality, endometrial receptivity, and the techniques used during embryo transfer all impact outcomes. Proper evaluation of the uterine cavity and cervical canal as well as techniques like ultrasound guidance and catheter selection are important.
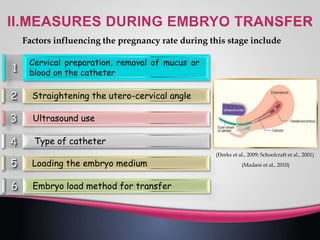
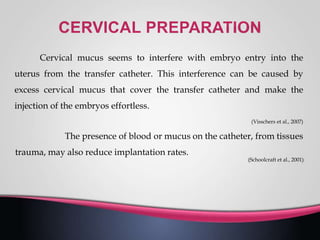
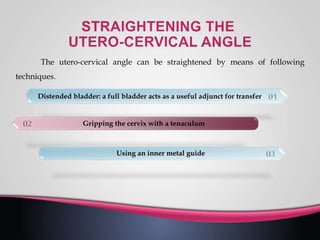
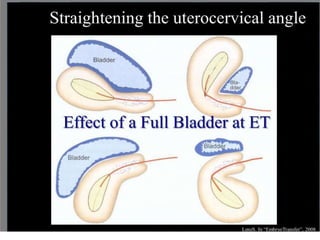
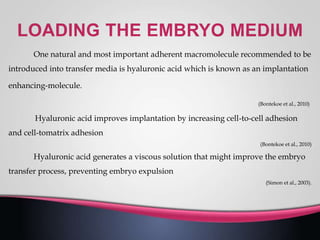
II. Factors during transfer like mucus removal, straightening the uterine angle, and catheter loading technique can also influence implantation and pregnancy rates.
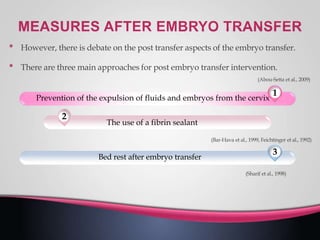
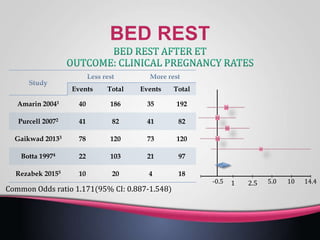
III. Some measures taken immediately after transfer like bedrest position may further optimize outcomes, though evidence is mixed on some post-transfer aspects. Overall, optimizing multiple steps before, during, and after embryo transfer can help maximize
![WeightTotalEventsTotalEvents
1.1.1 Injury in the pervious cycle
2.54
[0.88, 7.36]
37.4%5154911Narvekar 2010
2.42
[1.06, 5.51]
62.6%50125022
Selcuk University
2011
2.46
[1.28, 4.72]
100.0%10199Subtotal (95%CI)
1733Total events
Heterogeneity: Chi2= 0.01, df= 1 (P= 0.94); I2= 0%
Test for overall effect: Z= 2.71 (P= 0.007)
2.46 [1.28, 4.72]
100.0
%
10199Total (95% CI)
1733Total events
Heterogeneity: Chi2= 0.01, df= 1 (P= 0.94); I2= 0%
Test for overall effect: Z= 2.71 (P= 0.007)
Test for subgroup differences: Not applicable
Peto Odds Ratio
Peto, Fixed, 95% CI
Favor End.
Injury
0.1 0.2 10.5 2 105
Favor Control
NNT= 6](https://image.slidesharecdn.com/embryotransfer-200513000156/85/Embryo-transfer-15-320.jpg)
![WeightTotalEventsTotalEvents
1.3.1 Injury in the pervious cycle
3.36 [1.20, 9.37]16.9%5748513Karimzadeh 2009
2.88 [1.14, 7.28]20.7%5174916Narvekar 2010
2.01 [0.97, 4.19]33.2%60186028Nastri 2011
2.81 [1.29, 6.14]29.2%50175030Selcuk University 2011
2.61 [1.71, 3.97]100.0%218217Subtotal (95%CI)
4687Total events
Heterogeneity: Chi2= 0.79, df= 3 (P= 0.85); I2= 0%
Test for overall effect: Z= 4.45 (P= 0.00001)
1.3.2 Injury on the day of oocyte retrieval
0.30 [0.14, 0.63]100.0%7926779Karimzade 2010
0.30 [0.14, 0.63]100.0%7977Subtotal (95% CI)
269Total events
Heterogeneity:Not applicable
Test for overall effect: Z= 3.17 (P= 0.002)
Peto Odds Ratio
Peto, Fixed, 95% CI
Favor End.
Injury
0.1 0.2 10.5 2 105
Favor Control
NNT= 5](https://image.slidesharecdn.com/embryotransfer-200513000156/85/Embryo-transfer-16-320.jpg)
![Peto Odds Ratio
Fixed, 95% CI
1.14 [0.80, 1.62]
0.01 0.1 1 10 100
Flushing No Flushing
Empty bladder
72/126
26/93
13/50
269
72/12657/127Glass 2000
26/9328/91Kyono 2001
13/5018/50Sallam 2000
269268Total](https://image.slidesharecdn.com/embryotransfer-200513000156/85/Embryo-transfer-21-320.jpg)
![25/6426/67Lorusso 2005
13/7612/66Mitchell 1989
140133Total
No effect on the pregnancy rate for women
undergoing ET with a full or an empty bladder
Peto Odds Ratio
Fixed, 95% CI
0.98 [0.57, 1.68]
0.02 0.1 1 10 50
Empty bladder
25/64
13/76
140](https://image.slidesharecdn.com/embryotransfer-200513000156/85/Embryo-transfer-25-320.jpg)

![TotalEventsTotalEvents
193124193137Balaban 2014
4895419Dittmann-Muller 2009
93159443Friedler 2005
5055118Friedler 2007
411655Hazlett 2008
1583013830Korosec 2007
305309Mahani 2007
42214117Morbeck 2007
69217921Ravhon 2005
84439158Schoolcraft 2002
40214025Simon 2003
643312639349Urman 2008
65226426Yakin 2004
Peto Odds Ratio
Fixed, 95% CI
1.14 [0.80, 1.62]
0.01 0.1 1 10 100
Favours no
or low HA
Favours HA](https://image.slidesharecdn.com/embryotransfer-200513000156/85/Embryo-transfer-35-320.jpg)