This document provides information about elbow disarticulation amputations including the level of amputation, statistics, causes, management, surgical issues, prosthetic components, and functional restoration. Some key points are:
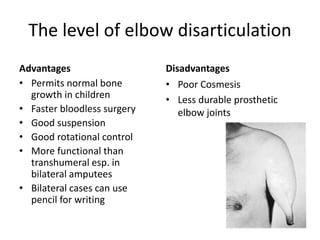
- Elbow disarticulation permits normal bone growth in children and allows for a faster and bloodless surgery compared to higher levels of amputation.
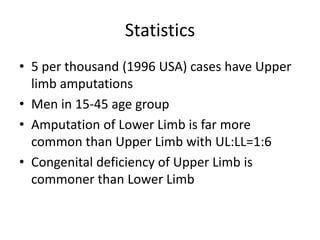
- In the US in 1996, 5 per 1000 amputation cases involved the upper limb, mostly affecting men aged 15-45. Upper limb amputations are less common than lower limb with a ratio of 1:6.
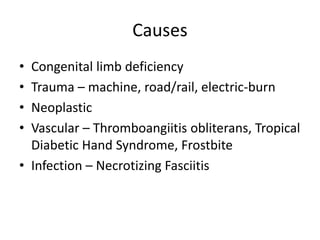
- Causes include congenital limb deficiencies, trauma, neoplasms, vascular issues like frostbite, and infections.