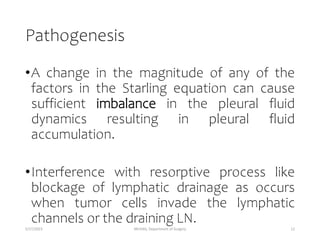
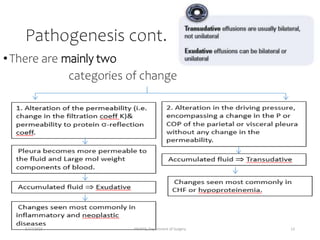
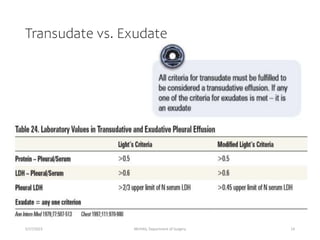
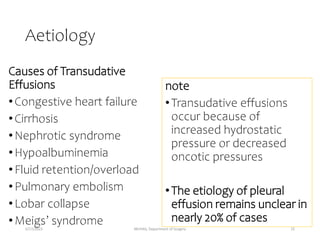
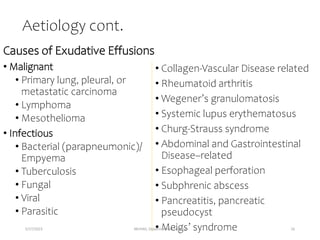
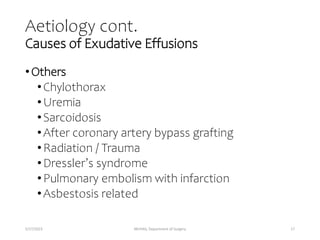
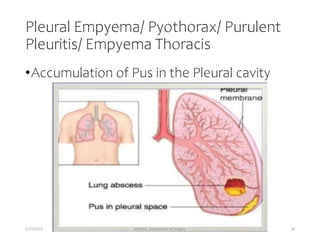
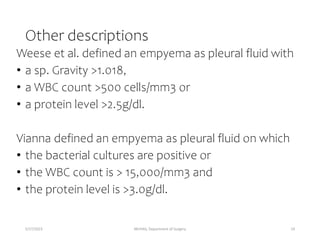
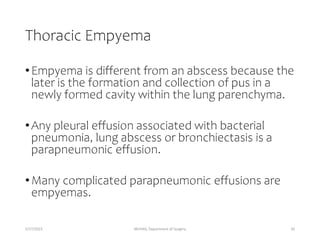
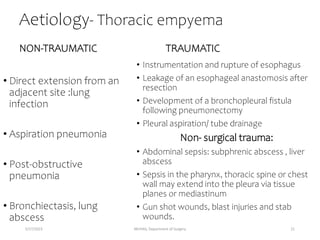
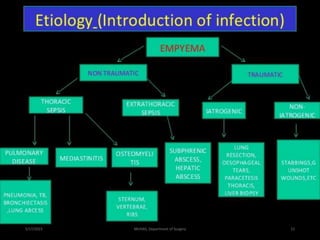
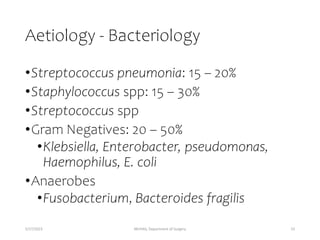
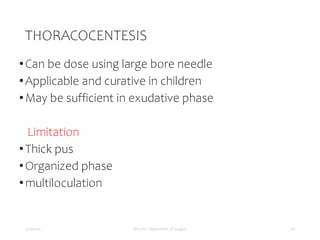
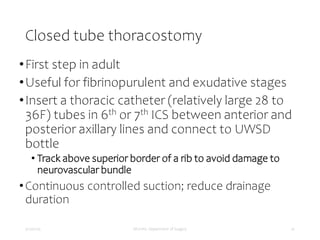
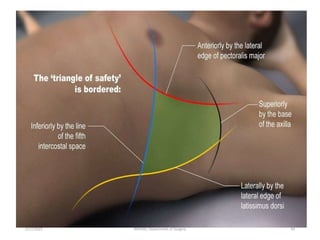
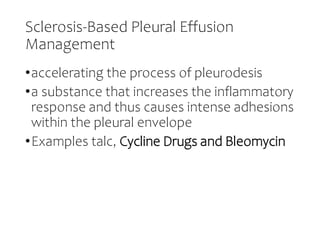
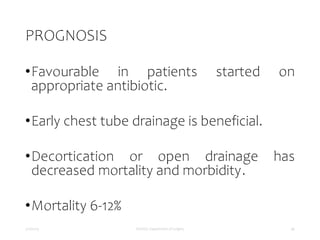
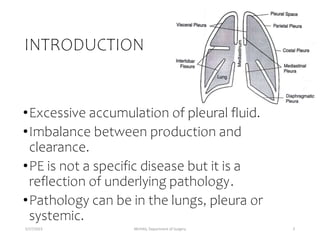
This document provides information on pleural effusion and thoracic empyema. It begins with objectives and introductions. It then covers anatomy and physiology of the pleura, pathogenesis and causes of pleural effusion and empyema. It discusses the classification of transudative versus exudative effusions. It also covers clinical presentation, complications, and treatment options for pleural effusion, empyema and malignant pleural effusions. Treatment methods discussed include thoracentesis, tube thoracostomy, drainage-based methods, and obliteration of the pleural space.

![Physiology cont.
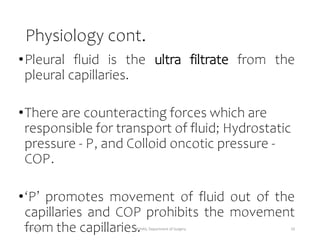
Fluid movement = K[(Pc –Pis ) – σ(COPc –COPis )]
Starlings equationcan be
applied to parietal pleura:
Pc = 30 cm H2 O,
Pis (mean intrapleural pressure)=
- 5 cm H2 O,
COPc = 32 cm H2 O,
COPis = 6 cm H2 O,
=1, K=1
Fluid movement at parietal
pleura = [30-(-5)]-1(32-6)
= 9 cm H2 O
5/17/2023 MUHAS, Department of Surgery 11](https://image.slidesharecdn.com/effusion-230517002707-fd0c5ae9/85/effusion-pptx-11-320.jpg)