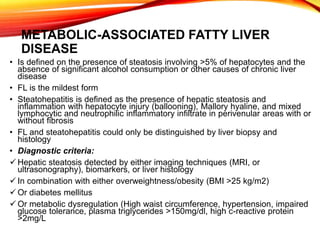
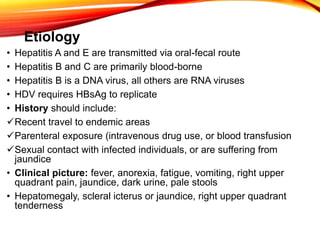
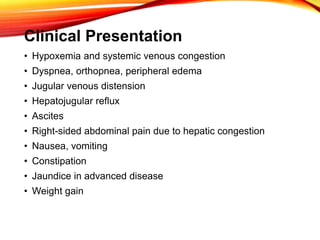
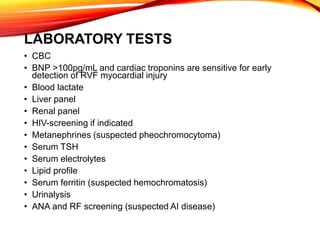
This document discusses the differential diagnosis of hepatomegaly, which can be caused by heart failure, viral hepatitis, or fatty liver disease. Heart failure leads to hepatomegaly through hepatic congestion from right-sided heart failure. Viral hepatitis involves inflammation of the liver from viruses like hepatitis A, B, C, etc. Fatty liver disease, which includes fatty liver and steatohepatitis, is associated with obesity, diabetes, and metabolic abnormalities that cause fat accumulation in the liver. The document provides details on the evaluation, diagnosis, and features of these conditions.