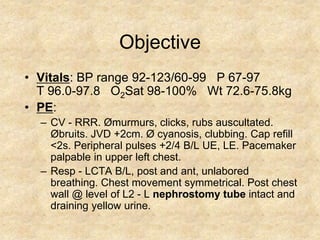
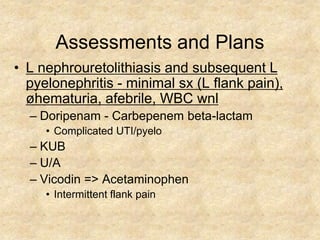
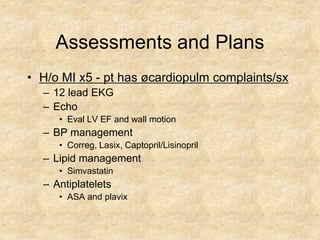
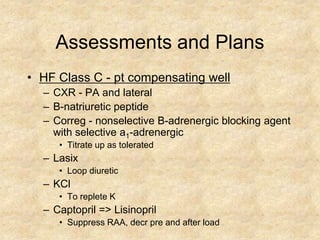
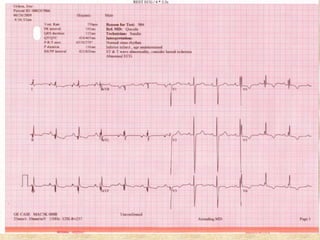
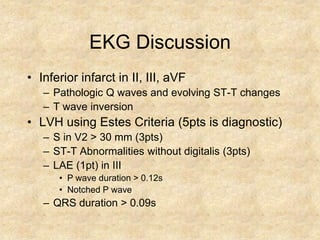
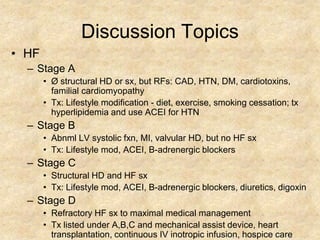
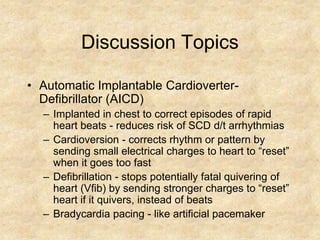
This document presents a cardiology case of a 56-year-old Hispanic male with a history of heart failure, ischemic cardiomyopathy, myocardial infarctions, hypertension, and strokes who was transferred for outpatient IV antibiotics and cardiology consultation. The patient's medical history, medications, physical exam findings, assessments, and treatment plans are summarized. Discussion topics include the patient's heart failure stage, electrocardiogram and chest x-ray findings, and automatic implantable cardioverter-defibrillator.